What Is Parkinsons Disease
Parkinsons disease is a chronic neurological condition. It is progressive and symptoms worsen over time. It is named after Dr James Parkinson who first described the condition in 1817.
People with Parkinsons disease experience a loss of nerve cells in the part of their brains responsible for controlling voluntary movements. This part of the brain is called the substantia nigra . The nerve cells in the substantia nigra usually produce a chemical called dopamine which helps transmit messages from the brain to the rest of the body via the central nervous system . As these cells are lost, people with Parkinsons disease experience a loss of dopamine and the messages controlling movement stop being transmitted efficiently.
Parkinsons disease is more common as people get older but it can affect younger adults. Men tend to be affected in slightly higher numbers than women.
Preparing For A Parkinsons Mri
A Parkinsons MRI is completely painless, but you do have to lie still while being scanned. Some patients feel claustrophobic in this situation. If youre worried about that, talk with your doctor about the possibility of having an anti-anxiety medication before the procedure.
On the day of the appointment, follow any instructions provided to you by your doctor. Remove metal jewelry and dont wear make-up as that can also have metal in it. If you are in the advanced stages of Parkinsons or if you are taking a sedative, you should arrange transportation to and from the appointment.
What Are The Treatments
Currently there is no cure for Parkinsons disease.
Symptoms can be mild in the early stages of the condition and people might not need immediate treatment. Your doctor and specialist will monitor your situation.
There are several different types of drugs used to treat Parkinsons disease. Drug treatments are tailored to each individuals needs and are likely to involve a combination of different drugs. Your medication should be reviewed regularly. It is likely that, over time, changes will be made to the types of drugs you take and the doses you take each day.
The main types of drug treatment for Parkinsons disease are:
- drugs which replace dopamine
- drugs which mimic the role of dopamine
- drugs which inhibit the activity of acetylcholine
- drugs which prevent the body breaking down dopamine
- other drugs such as anti-sickness medication
Everybody is affected differently by medication. The possible side effects of Parkinsons disease drugs include nausea , vomiting , tiredness and dizziness. Some people might experience confusion, nightmares and hallucinations. For some people, dopamine agonists have been linked to compulsive behaviour such as addictive gambling or hypersexuality .
The effectiveness of the main drug treatment levodopa can wear off over time and its long-term use can cause some people to develop involuntary twisting or writhing movements of the arms, legs or face . To reduce the risk, doctors might delay the use of levodopa for younger people.
Don’t Miss: Can You Recover From Parkinson’s Disease
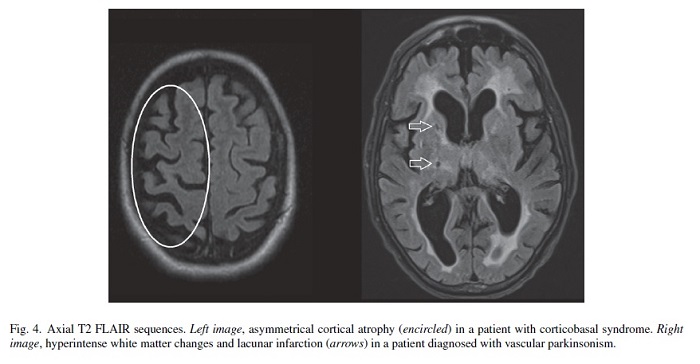
Exclusion Of Alternative Diagnoses
Structural MRI with conventional MR sequences is usually normal in early PD patients limiting its application in clinical routine for the detection of early PD. Recent studies, however, identified imaging correlates of underlying neuropathology in PD patients through advanced MRI techniques. These imaging abnormalities will be discussed in detail later in this review. Nevertheless, cMRI was repetitively shown to be useful in discriminating PD from APDs such as MSA and PSP. Latter are characterized by disease-specific atrophy patterns and signal intensity changes. In addition, current operational diagnostic criteria require the exclusion of symptomatic causes of parkinsonism in the work-up of patients with PD .
Also Check: Parkinsons Disease And Sleep
Regional Cerebral Glucose Metabolism And Pd
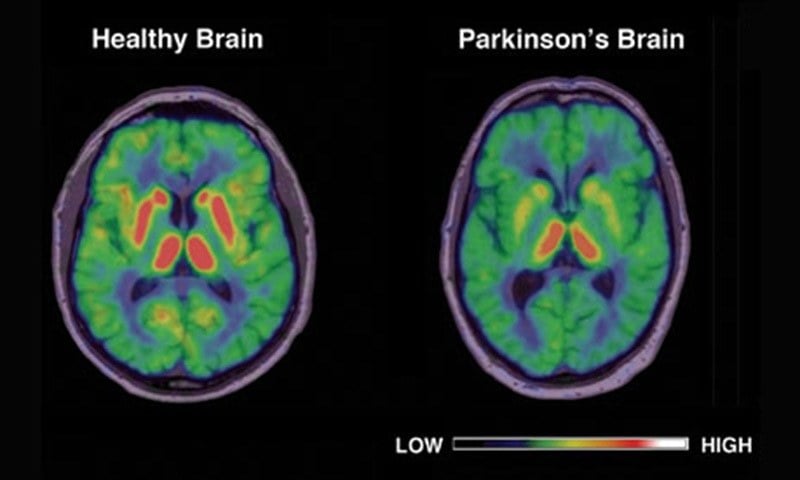
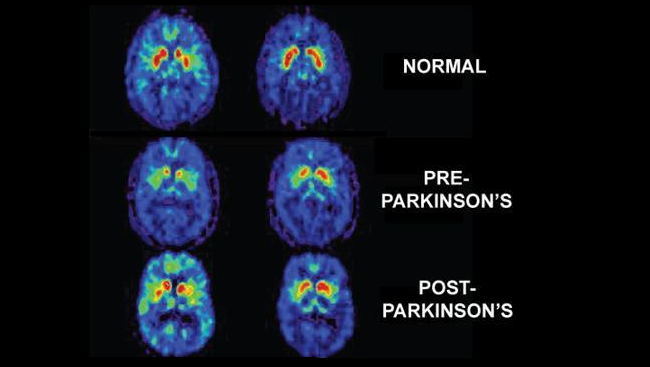
18F-FDG PET can be used to assess levels of resting regional cerebral glucose metabolism. Absolute levels in the lentiform nucleus lie within the reference range in PD however, covariance analysis reveals an abnormal profile of relatively raised resting lentiform nucleus and lowered frontal and parietotemporal metabolism . The degree of expression of this PD-related profile correlates with clinical disease severity, thus providing a potential biomarker of disease progression. Successful treatment with levodopa or deep brain stimulation reduces expression of the PD-related profile . Given this, changes in treatment could result in a potential confounding factor if 18F-FDG PET were to be used as a biomarker to follow PD progression.
Eckert et al. performed 18F-FDG PET on 8 patients with suspected early parkinsonism but normal findings on 18F-dopa PET . None of these 8 patients expressed a PD-related profile of glucose metabolism, and over 3 y none of them showed any clinical progression of their disorder. This finding reinforces the viewpoint that normal dopaminergic imaging excludes the presence of a degenerative parkinsonian syndrome.
Recommended Reading: What Are Some Signs Of Parkinson’s Disease
How Parkinsons Disease Is Diagnosed
Parkinsons disease is usually diagnosed clinically, meaning that a physician looks for the presence or absence of the possible symptoms of Parkinsons disease by interviewing the patient and performing a detailed neurologic examination.
While there is presently no definitive test for Parkinsons, it can often be identified by a general neurologist, who is trained to diagnose and treat neurologic disorders. To avoid misdiagnosis, consultation with a movement disorder specialist is recommended. A movement disorder specialist is a physician who has undergone additional, subspecialty training in the diagnosis and treatment of movement disorders, such as Parkinsons, after training in general neurology.
What to expect during your visit with a physician
Typically, a trained physician will only consider the diagnosis of Parkinsons disease if the person being examined has at least two of the core motor symptoms of Parkinsons, including tremor, the characteristic bradykinesia , or rigidity. At the end of your visit, the physician should discuss with you why you may or may not have Parkinsons disease and the level of certainty about the diagnosis. This determination is based on your medical history and examination at this visit.
Brain imaging and other tools to aid diagnosis of Parkinsons
Caring For Someone With Parkinsons
Practice patience and understanding when dealing with Parkinsons. You may be very frustrated and challenged as a caregiver, but those with Parkinsons are just as frustrated. Their physical and mental conditions can be debilitating, depressing, and humiliating.
Diet and nutrition can have a huge impact on the health and comfort of a Parkinson patient. Eating well, getting more rest, sleeping well, fresh air, and exercise can make a difference. Getting the right medication and complementary therapies is also important.
As Parkinsons impacts a patients motor skills, modifications to the living environment may have to be made to accommodate wheelchairs and limited mobility issues. Professional in-home assistance for Parkinsons can allow Parkinson patients to remain independent and can enhance quality of life.
Most importantly, seek help and support from family, friends, and caregiving support groups. Take advantage of the resources in your community. Shouldering all the burden can take a toll on a caregiver.
Take care of yourself or you wont be able to take care of your loved one. Follow the preventive advice provided above for yourself as well, and take deep breaths!
Resources
Also Check: First Line Treatment For Parkinson’s
What Can You Detect With A Parkinsons Mri
Generally, you can receive a Parkinsons diagnosis in a clinical setting, but an MRI can help to assess various aspects of the disease and its progress. In particular, a Parkinsons MRI can do the following for patients who have or are suspected to have Parkinsons disease:
- Evaluate tissue loss and how the brain is atrophying
- Check for changes to the basal ganglia region of the brain
- Find out if there are abnormal iron deposits in the basal ganglia or brainstem
- Look at changes to white matter
- Examine the diffusion of restricted tissues in acute infarction and neurodegenerative diseases
- Help to diagnose atypical parkinsonism
- Exclude treatable causes of parkinsonism such as normal pressure hydrocephalus
You May Like: Parkinsons Life Center Of Southern New Jersey
Researchers Examine How Parkinsons Disease Alters Brain Activity Over Time
Tracking neural changes could help researchers test therapies that slow disease progression.
Neuroscientists peered into the brains of patients with Parkinsons disease and two similar conditions to see how their neural responses changed over time. The study, funded by the NIHs Parkinsons Disease Biomarkers Program and published in Neurology, may provide a new tool for testing experimental medications aimed at alleviating symptoms and slowing the rate at which the diseases damage the brain.
If you know that in Parkinsons disease the activity in a specific brain region is decreasing over the course of a year, it opens the door to evaluating a therapeutic to see if it can slow that reduction, said senior author David Vaillancourt, Ph.D., a professor in the University of Floridas Department of Applied Physiology and Kinesiology. It provides a marker for evaluating how treatments alter the chronic changes in brain physiology caused by Parkinsons.
For decades, the field has been searching for an effective biomarker for Parkinsons disease, said Debra Babcock, M.D., Ph.D., program director at the NIHs National Institute of Neurological Disorders and Stroke . This study is an example of how brain imaging biomarkers can be used to monitor the progression of Parkinsons disease and other neurological disorders.
The study was supported by the NIH .
NIHTurning Discovery Into Health®
You May Like: How To Get Checked For Parkinson’s Disease
Detection Of Preclinical Pd
For every patient who presents with clinical PD there may be 10 subclinical cases with incidental brain stem Lewy body disease in the community . Subjects at risk of developing PD include carriers of genetic mutations known to be associated with parkinsonism , relatives of patients with the disorder, elderly subjects with idiopathic hyposmia, and patients with rapid-eye-movement sleep behavior disorders.
Relatives of PD patients with idiopathic hyposmia are at risk of PD. Ponsen et al. collected 40 such relatives after screening 400 subjects for hyposmia and, with 123I–CIT SPECT, found that 7 of these showed reduced striatal DAT binding . Four of these 7 subsequently converted to clinical PD over a 2-y period.
Patients with idiopathic rapid-eye-movement sleep behavior disorder are at high risk of developing parkinsonism or dementia. Using 123I-IPT SPECT, Eisensehr et al. found reduced striatal DAT binding in all 5 of their patients with idiopathic rapid-eye-movement sleep behavior disorder . In another series, 11 patients with sleep disorders were investigated with FP-CIT SPECT, and reduced striatal DAT binding was found in 3, 1 of whom had evidence of clinical parkinsonism .
Brain Mri Advances For Parkinsons Disease
In Parkinsons disease, the damage to brain cells begins long before any symptoms develop. Therefore, at-risk patients can benefit from early diagnosis, and efforts to slow the progression of the disease can start early.
Researchers are working on newer MRI approaches to precisely detect Parkinsons disease-related structural and metabolic activity in the brain and correlate it to the function of the organ. For example, scientists from Oxford University used a technique called the resting-state functional MRI to assess the strength of nerve cells in the a region of the brain called the basal ganglia to send and receive information. Because the physical signs of brain cell damage in Parkinsons disease are not recognizable by conventional MRI, this approach may help visualize the impact of the damage on the activity of brain cells and aid in early diagnosis.
Similarly, MRI is used to identify Parkinsons disease-specific biomarkers. Tracking the biomarkers using high-field and ultra-high field MRI can identify Parkinsons disease patients and help follow the progression of the condition.
Although many of these advancements are yet to be implemented in the clinical setting, such adaptations may help better understand the disease and develop new treatments.
Read Also: How Hereditary Is Parkinsons Disease
Recommended Reading: Lifespan For Parkinson’s Disease
Is Parkinsons Diagnosed In The Brain
Parkinsons disease is one of the most challenging neurological disorders to diagnose and treat. If your doctor suspects you have Parkinsons disease, you will usually be referred to a neurologist for further tests. These tests will involve certain movements and exercises to check your symptoms.
A neurologist will look for motor symptoms such as:
- A tremor that occurs at rest
- Slowed movement
- Muscle stiffness
If you have two or more of these symptoms and your doctor has taken blood tests to rule out other causes, its likely you will be diagnosed with Parkinsons disease. Your symptoms will be closely monitored to see any progression of Parkinsons disease, which can take years.
Recommended Reading: Clinical Trials On Parkinsons Disease
Moving To A Care Home
As your dementia progresses looking after yourself or having someone care for you at home may not be enough especially towards the later stages of the disease.
Dementia is a difficult disease for family and friends and looking after someone with dementia can be exhausting. When this happens a care home can provide the level of care needed.
Going into care can be expensive but there is help out there. Your local council may be able to help with partial or full funding depending on the capital you own.
Read Also: Parkinson’s Disease Emotional Symptoms
Gray Matter Density And Disease Duration Associations
To confirm that group level differences in regional GMD were related to disease duration, a set of regression analyses that examined the relationship between GMD and disease duration controlling for chronological age and sex was performed. The individual regression analyses were conducted using the data of both early and advanced PD patients to increase the range of disease duration present in the sample. For subcortical regions, Ch4 GMD declined with disease duration and Ch123 GMD declined with disease duration . The centromedial amygdala GMD declined with disease duration , superficial amygdala GMD declined with disease duration , laterobasal amygdala GMD declined with disease duration , amygdala-striatal transition area GMD declined with disease duration , and HATA GMD declined with disease duration . Entorhinal cortex GMD declined with disease duration . For cortical regions, only the GMD of the secondary auditory association area TE3 declined with disease duration .
Patient And Public Involvement
The OPDC Discovery Cohort is designed by and for patients and is closely linked with the Parkinsons UK local support group. Patient representatives are also involved in the funding/renewal and strategic oversight processes, and sit on the data access panel with casting votes. Results are disseminated to the study participants through annual newsletters, the OPDC website, and series of talks at participants open days.
Also Check: Using Cbd For Parkinson’s Disease
I Have Pd And Several Symptoms Should I Get A Datscan
Likely no. There is no need for DaTscan when your history and exam suggest Parkinsons disease and you meet the diagnostic criteria. Occasionally, if signs and symptoms are mild or you dont meet the diagnostic criteria, your doctor will refer you for a DaT scan. Keep in mind that ultimately the diagnosis is based on your history and physical exam. The DaT scan is most commonly used to complete the picture and is not a test for a diagnosis.
Presynaptic And Postsynaptic Dopaminergic Imaging
11C-DTBZ tracer or labels the vesicular monoamine transporter type-2 , important for packaging and storing monoamines into synaptic vesicles. 11C-DTBZ PET have shown decreased striatal VMAT2 binding in PD reflecting nigrostriatal degeneration, accompanied by rather minimal compensatory changes . Conversely, the binding potential for 11C-methylphenidate was reduced to a much greater extent relative to 11C-DTBZ, suggesting marked compensatory down-regulation of striatal DAT activity . Using a novel 18F-tetrabenazine derivative , Okamura et al. detected the greatest regional decrease in VMAT2 binding in the posterior putamen, followed by anterior putamen and caudate nucleus in PD .
Also Check: Fitflop Shoes For Parkinson’s
Strengths And Limitations Of This Study
-
High-quality 3T MRI data in a very well phenotyped and longitudinally followed cohort of Parkinsons and rapid eye movement sleep behaviour disorder were acquired on the same MRI scanner, quite unique for a study of this duration.
-
Clinical longitudinal data are acquired every 18 months, information about conversion to Parkinsons of the at-risk individuals will be available, and MRI follow-up is ongoing.
-
Statistical maps of published results and support data relative to the analyses are available to share.
-
Oxford Parkinsons Disease Centre-MRI phenotyping is deep and relatively frequent, however, the size of the cohort is not at the level of population-level cohort studies.
-
MRI sequences are high quality, but could not exploit the latest advances in the field in order to maintain continuity.
Tests To Rule Out Other Conditions
Blood tests can help rule out other possible causes of the symptoms, such as abnormal thyroid hormone levels or liver damage.
An MRI or CT scan can check for signs of a stroke or brain tumor, which may cause similar symptoms.
Hydrocephalus due to atrophy can occur with some types of dementia and would be visible with one of these imaging tests. If the person has neurologic symptoms but a normal scan result, Parkinsons disease may be present.
The doctor a lumbar puncture to rule out inflammation or a brain infection.
You May Like: Does Parkinson’s Make You Forget Things
Structural Magnetic Resonance Imaging
Magnetic resonance imaging takes advantage of abundant hydrogen atoms and strong magnetic fields to image brain tissues non-invasively. Conventional structural MRI uses distinct pulse sequences to obtain T1-weighted , T2-weighted , proton-density weighted, fluid-attenuated inversion recovery and/or susceptibility-weighted scans. SW imaging is sensitive to magnetic inhomogeneity effects, particularly due to iron accumulation, hemorrhages, and/or slow venous blood flow, allowing for an enhanced tissue contrast. These images can be analyzed selectively or in combination to obtain volumes of brain structures, regional cortical thickness, and to identify regional tissue abnormalities. Such structural profiles, including patterns and rates of atrophy, are important areas of research from a biomarker viewpoint.
Structural MRI profiles of Parkinsons disease
Structural MRI profiles of Lewy body spectrum disorders
Structural MRI profiles of multiple system atrophy
Fig. 1
Questions To Ask Your Doctor
Its a good idea to ask questions as you and your doctor discuss a treatment. Asking questions can help you make sure you understand your condition and the benefits of treatment. Here are some sample questions to ask your doctor:
- Is it possible something other than Parkinsons is causing my symptoms?
- Do I need additional tests?
- How will my condition progress?
- What can I expect as my condition progresses?
- How will Parkinsons affect my other medical conditions?
- What treatments are available?
- Which treatments are best for me?
- How will treatments help my current symptoms?
- Will treatment slow down the progression of Parkinsons?
- What side effects do your recommended treatments have?
- What happens if these treatments dont help?
- Can you recommend any resources or educational material for me?
Also Check: Laser Pointer For Parkinson’s