Prevalence Incidence And Risk Factors For Motor Complications
Nearly all patients develop motor fluctuations and LID by 15 to 20 years from time of diagnosis . However, prevalence and incidence figures through the course of PD vary depending on the study methodology employed and by the predominant treatment strategies of the time. Early literature suggested that approximately 10% of patients per year following initiation of treatment with levodopa develop motor fluctuations, with 40% of patients developing these complications within 46 years of treatment . A large cross-sectional study of 617 patients with PD found an overall prevalence of wearing off of 57% as assessed by neurologists and 67% as assessed by a patient-completed questionnaire . Of patients with disease duration < 2.5 years, wearing off was identified in 41.8% by the WOQ-19 and in 21.8% by neurologists, indicating that motor fluctuations can emerge as early as several months to a few years after the initiation of levodopa, as has also been observed in other studies . A retrospective analysis of an incident cohort of PD found estimated rates of dyskinesia of 30% by 5 treatment years and 59% by 10 treatment years .
Diagnosis Of Parkinsons Disease
The diagnosis of PD is clinical and requires bradykinesia, defined as slowness of movement and decrement in amplitude or speed, usually assessed using finger tapping, foot tapping or pronationsupination hand movements. In addition, rest tremor or rigidity is required to confirm a parkinsonian syndrome. Tremor was absent at presentation in 30% in one series of pathologically proven PD. Patients with suspected PD should be referred quickly and untreated to a specialist in movement disorders for evaluation. Key points for discussion at diagnosis include the need to inform vehicle licensing agencies and insurers, signposting to written or web-based information on newly diagnosed PD, and provision of contact details for the local PD nurse specialist .
Current International Parkinson and Movement Disorder Society diagnostic criteria for Parkinsons disease adapted from Postuma RB, Berg D, Stern M et al. MDS clinical diagnostic criteria for Parkinsons disease. Mov Disord 2015 30:1591601. At least two supportive criteria and no red flags required for a diagnosis of clinically established Parkinsons disease. Conditions in italics should be considered if the corresponding exclusion criteria or red flags are present.
You May Like: Does Parkinsons Cause Weight Gain
How Soon After Treatment Will I Feel Better And How Long Will It Take To Recover
The time it takes to recover and see the effects of Parkinson’s disease treatments depends strongly on the type of treatments, the severity of the condition and other factors. Your healthcare provider is the best person to offer more information about what you can expect from treatment. The information they give you can consider any unique factors that might affect what you experience.
Also Check: Parkinson’s Tips And Tricks
Diagnosis And Management Of Parkinsons Disease
There are no diagnostic tests for Parkinsons. X-rays, scans and blood tests may be used to rule out other conditions. For this reason, getting a diagnosis of Parkinsons may take some time.
No two people with Parkinsons disease will have exactly the same symptoms or treatment. Your doctor or neurologist can help you decide which treatments to use.
People can manage their Parkinsons disease symptoms through:
- seeing a Doctor who specialises in Parkinsons
- multidisciplinary therapy provided for example, by nurses, allied health professionals and counsellors
- deep brain stimulation surgery .
Who Does It Affect
The risk of developing Parkinsons disease naturally increases with age, and the average age at which it starts is 60 years old. Its slightly more common in men or people designated male at birth than in women or people designated female at birth .
While Parkinsons disease is usually age-related, it can happen in adults as young as 20 .
Read Also: Late Stage Parkinson’s Symptoms
Support For People With Parkinsons Disease
Early access to a multidisciplinary support team is important. These teams may include doctors, physiotherapists, occupational therapists, speech therapists, dietitians, social workers and specialist nurses. Members of the team assess the person with Parkinsons disease and identify potential difficulties and possible solutions.There are a limited number of multidisciplinary teams in Victoria that specialise in Parkinsons disease management. But generalist teams are becoming more aware of how to help people with Parkinsons disease.
Dietary Considerations With Medications
Treatments are only effective in moderating the symptoms of the disease, mainly with drugs including levodopa and dopamine agonists. Once too many dopamine producing cells have been lost however, the effects of L-DOPA become less effective. Once this occurs, a complication known as dyskenesia commonly occurs in which subjects undergo involuntary writhing movements despite the use of L-DOPA. The effects of dyskenesia vary between periods of high symptoms and low symptoms. In order to limit the onset of dyskenesia, typical L-DOPA dosages are kept as low as possible while still achieving desired results. Lastly, in cases in which drugs are ineffective, deep brain stimulation and surgery can be used to reduce symptoms.
Levodopa is taken orally and is absorbed through the small intestines into the blood, competing for access with natural proteins. Additionally, once the drug has entered the blood stream, L-DOPA utilizes the same pathways to cross the blood brain barrier as natural protein. Only about 5 10% of levodopa crosses the blood brain barrier, while the remaining is metabolized elsewhere in the body. The metabolism of medications elsewhere is known to cause side effects such as nausea, dsykinesias, and stiffness.
Also Check: Non Motor Features Of Parkinson Disease
Stay Safe With Your Medicines
Read all labels carefully.
- Tell all your health care providers about all the medicines and supplements you take.
- Know all the medicines and foods youâre allergic to.
- Review any side effects your medicines can cause. Most reactions will happen when you start taking something, but thatâs not always the case. Some reactions may be delayed or may happen when you add a drug to your treatment. Call your doctor right away about anything unusual.
- Use one pharmacy if possible. Try to fill all your prescriptions at the same location, so the pharmacist can watch for drugs that might interact with each other.
- You can use online tools to see if any of your medicines wonât work well together.
You have the right and responsibility to know what medications your doctor prescribes. The more you know about them and how they work, the easier it will be for you to control your symptoms. You and your doctor can work together to create and change a medication plan. Make sure that you understand and share the same treatment goals. Talk about what you should expect from medications so that you can know if your treatment plan is working.
Show Sources
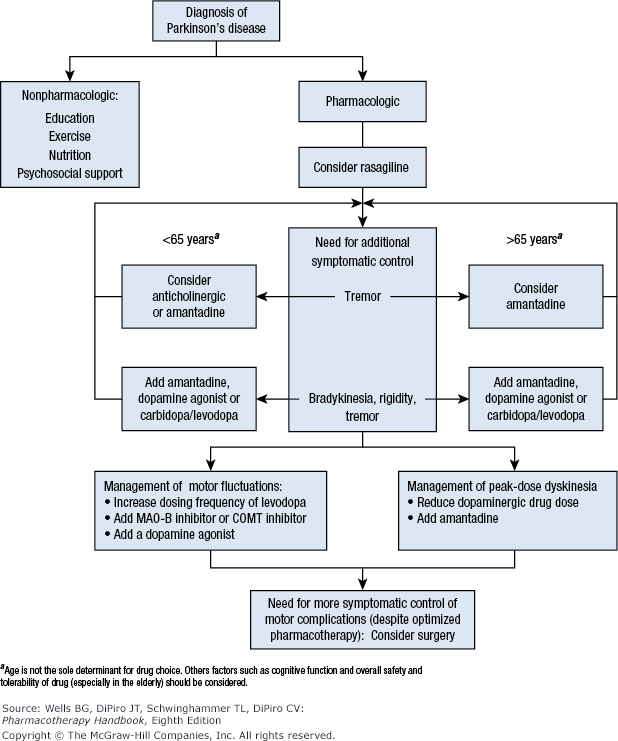
Medical Management Of Motor Complications
Medication approaches to the management of motor fluctuations include shortening the interdose interval of carbidopa-levodopa immediate release , switching to a longer acting CD-LD oral formulation, adding a maintenance or on-demand adjunctive medication, or employing infusion therapy. Medication management of peak-dose LID may include reducing individual levodopa doses, fractionating the levodopa dose , or adding an amantadine formulation. In the following sections, evidence for these medication options is reviewed, followed by a discussion of the clinical application of these options during the course of advancing PD. These medications are also summarized in Table 1.
Table 1 Medications in the treatment of motor complications in Parkinsons disease
Don’t Miss: Parkinson’s Disease Charity Donations
Surgery For People With Parkinsons Disease
Deep brain stimulation surgery is an option to treat Parkinsons disease symptoms, but it is not suitable for everyone. There are strict criteria and guidelines on who can be a candidate for surgery, and this is something that only your doctor and you can decide. Surgery may be considered early or late in the progression of Parkinsons. When performing deep-brain stimulation surgery, the surgeon places an electrode in the part of the brain most effected by Parkinsons disease. Electrical impulses are introduced to the brain, which has the effect of normalising the brains electrical activity reducing the symptoms of Parkinsons disease. The electrical impulse is introduced using a pacemaker-like device called a stimulator. Thalamotomy and pallidotomy are operations where the surgeon makes an incision on part of the brain. These surgeries aim to alleviate some forms of tremor or unusual movement, but they are rarely performed now.
Patients Disposition And Demography
The patients disposition is summarized in Fig. 1. Out of the 307 patients randomized, 267 patients completed the study treatment . A total of 40 patients withdrew from the study . The most common reason for discontinuation was AEs , followed by withdrawal by patient and physician decision . None of the patients withdrew from the study because of coronavirus disease 2019. The mean treatment duration was 15.4 weeks in the safinamide group and 14.4 weeks in the placebo group. At day 15, all patients received the 100-mg dose and more than 97% had a treatment adherence of 100% at week 16.
Fig. 1
Recommended Reading: The Progression Of Parkinson’s
Parkinson’s Disease Nurse Specialists
The development of specialist peripatetic nurses for Parkinson’s disease has been led by the Parkinson’s Disease Society in the UK. From small beginnings, around 100 are now funded from various sources including the NHS. The nurses have a number of roles but they primarily act as a key worker for the patient with Parkinson’s disease, liaising with therapists, social services, the primary and secondary care teams, etc. They serve to educate the patient, relatives, and members of the medical and allied professions about the condition. Their ability to help the patient with complex changes in medication, including apomorphine infusions, within set limits can be invaluable. Parkinson’s disease nurse specialists have been the subject of a recent large RCT which showed significant improvements in an open label patient global impression scale at no additional cost to the NHS. No advantages in quality of life or mortality were found, but the study was confounded by selegiline withdrawal.
Symptomatic And Neuroprotective Therapy
Pharmacologic treatment of Parkinson disease can be divided into symptomatic and neuroprotective therapy. At this time, there is no proven neuroprotective or disease-modifying therapy.
Levodopa, coupled with carbidopa, a peripheral decarboxylase inhibitor , remains the gold standard of symptomatic treatment for Parkinson disease. Carbidopa inhibits the decarboxylation of levodopa to dopamine in the systemic circulation, allowing for greater levodopa distribution into the central nervous system. Levodopa provides the greatest antiparkinsonian benefit for motor signs and symptoms, with the fewest adverse effects in the short term however, its long-term use is associated with the development of motor fluctuations and dyskinesias. Once fluctuations and dyskinesias become problematic, they are difficult to resolve.
Monoamine oxidase -B inhibitors can be considered for initial treatment of early disease. These drugs provide mild symptomatic benefit, have excellent adverse effect profiles, and, according to a Cochrane review, have improved long-term outcomes in quality-of-life indicators by 20-25%.
Neuroprotective therapy aims to slow, block, or reverse disease progression such therapies are defined as those that slow underlying loss of dopamine neurons. Although no therapy has been proven to be neuroprotective, there remains interest in the long-term effects of MAO-B inhibitors. Other agents currently under investigation include creatine and isradipine.
Recommended Reading: Parkinson’s Disease Education Handout
Basics Of Parkinsons Disease
Parkinsons disease , or paralysis agitans, is a common neurodegenerative condition, which typically develops between the ages of 55 and 65 years. This disease was first named and described by James Parkinson in 1817. The progression of this disease is gradual and prolonged. It has a plausible familial incidence, although the estimates of these occurrences are low and usually sporadic. This disease is organized into two classifications: genetic and sporadic. Genetic PD follows Mendelian inheritance. Sporadic PD, which accounts for about 90% of all Parkinsons cases, is a more complex category in which the pathogenic mechanisms that underlie it are not yet fully understood. Nonetheless, it is known that the byzantine interactions of genetic and environmental influences play roles in the determination of sporadic PD. Several subtypes of PD exist. Each has its own set of causative factors and susceptibilities, pathology, and treatment courses. General risk factors, symptoms, and pathology will be discussed first, before addressing some of the subtypes.
What Can I Expect If I Have This Condition
Parkinsons disease is a degenerative condition, meaning the effects on your brain get worse over time. However, this condition usually takes time to get worse. Most people have a normal life span with this condition.
You’ll need little to no help in the earlier stages and can keep living independently. As the effects worsen, youll need medication to limit how the symptoms affect you. Most medications, especially levodopa, are moderately or even very effective once your provider finds the minimum dose you need to treat your symptoms.
Most of the effects and symptoms are manageable with treatment, but the treatments become less effective and more complicated over time. Living independently will also become more and more difficult as the disease worsens.
How long does Parkinsons disease last?
Parkinsons disease isnt curable, which means its a permanent, life-long condition.
Whats the outlook for Parkinsons disease?
Parkinson’s disease isn’t fatal, but the symptoms and effects are often contributing factors to death. The average life expectancy for Parkinson’s disease in 1967 was a little under 10 years. Since then, the average life expectancy has increased by about 55%, rising to more than 14.5 years. That, combined with the fact that Parkinson’s diagnosis is much more likely after age 60, means this condition doesn’t often affect your life expectancy by more than a few years .
Read Also: Neck Brace For Parkinson’s
Anticholinergics For Early On
The first pharmacological agents used in PD therapy were anticholinergic drugs. They reduce the activity of acetylcholine by acting as antagonists at choline receptors, hoping to restore the balance between dopamine and acetylcholine levels that was disturbed by PD. These drugs have largely been replaced by L-DOPA and other centrally acting dopaminergic agonists, but they still remain available for use in the treatment of PD. Benztropine, biperiden, diphenhydramine, ethopropazine, orphenadrine, procyclidine, and trihexyphenidyl are included in this therapeutic class of drugs, though there is little pharmacokinetic information available on them because of their low plasma drug concentrations. Typically, anticholinergic drugs have a greater role in tremor-predominant PD and can be a monotherapy in early stages, but are usually done in adjunct with L-DOPA or other prescribed medications.
You May Like: Parkinsons Disease Exercise Program
A New Era For Parkinsons Disease Treatment
March 2, 2022 | By
A non-invasive ultrasound treatment for Parkinsons disease that was tested in a pivotal trial led by University of Maryland School of Medicine researchers is now broadly available at the University of Maryland Medical Center .
Howard Eisenberg, MD, Dheeraj Gandhi, MD, MBBS, Paul Fishman, MD, PhD, Bert W. OMalley, MD.
The device, called Exablate Neuro, was approved in November by the U.S. Food and Drug Administration to treat advanced Parkinsons disease on one side of the brain. The approval was based on findings from the UMSOM clinical trial and effectively expands access to focused ultrasound beyond clinical trial participation.
Rapid Reversal of Symptoms
Focused ultrasound is an incisionless procedure, performed without the need for anesthesia or an in-patient stay in the hospital. Patients, who are fully alert, lie in a magnetic resonance imaging scanner, wearing a transducer helmet. Ultrasonic energy is targeted through the skull to the globus pallidus, a structure deep in the brain that helps control regular voluntary movement. MRI images provide doctors with a real-time temperature map of the area being treated. During the procedure, the patient is awake and providing feedback, which allows doctors to monitor the immediate effects of the tissue ablation and make adjustments as needed.
Patient: Focused Ultrasound Changed My Life
A New Era for Parkinsons Disease Treatment
Don’t Miss: How Does Parkinson Disease Affect The Muscular System
Can Parkinson’s Disease Be Cured
No, Parkinson’s disease is not curable. However, it is treatable, and many treatments are highly effective. It might also be possible to delay the progress and more severe symptoms of the disease.
A note from Cleveland Clinic
Parkinson’s disease is a very common condition, and it is more likely to happen to people as they get older. While Parkinson’s isn’t curable, there are many different ways to treat this condition. They include several different classes of medications, surgery to implant brain-stimulation devices and more. Thanks to advances in treatment and care, many can live for years or even decades with this condition and can adapt to or receive treatment for the effects and symptoms.
Symptoms Of Parkinsons Disease
The type, number, severity and progression of Parkinsons disease symptoms vary greatly. Every person is affected differently they may not get every symptom.
Some of the more common symptoms are:
- blood pressure fluctuation
People living with Parkinsons for some time may experience hallucinations , paranoia and delusions . These symptoms are able to be treated so have a talk with your doctor.
Also Check: Stretching Exercises For Parkinson’s Patients
What Is Parkinsons Disease
Parkinsons disease is a nervous system disease that affects your ability to control movement. The disease usually starts out slowly and worsens over time. If you have Parkinsons disease, you may shake, have muscle stiffness, and have trouble walking and maintaining your balance and coordination. As the disease worsens, you may have trouble talking, sleeping, have mental and memory problems, experience behavioral changes and have other symptoms.
Recommended Reading: Parkinsons And Bad Taste In Mouth
The Surgical Option: Deep Brain Stimulation
Some patients with Parkinsons disease may benefit from deep brain stimulation , a surgical therapy that has been FDA approved for over a decade. DBS involves implanting an electrode into a targeted area of the brain, usually the subthalamic nucleus or the globus pallidus interna . The implants can be done on one side or both sides of the brain as needed. The electrodes are stimulated through a connection to a pacemaker-like device located under the skin in the chest. Patients that are considered good candidates for this procedure are those with a robust response to Levodopa, no significant cognitive or psychiatric problems, and no significant problems with balance. The procedure can help patients with medication-resistant tremors. It can also help patients who have significant motor fluctuations in which medication response varies during the day and dyskinesias or extra movements may occur as a side effect of medication.
Read Also: What Are The Signs Symptoms Of Parkinson’s Disease