Effects Of Surgery On Nms
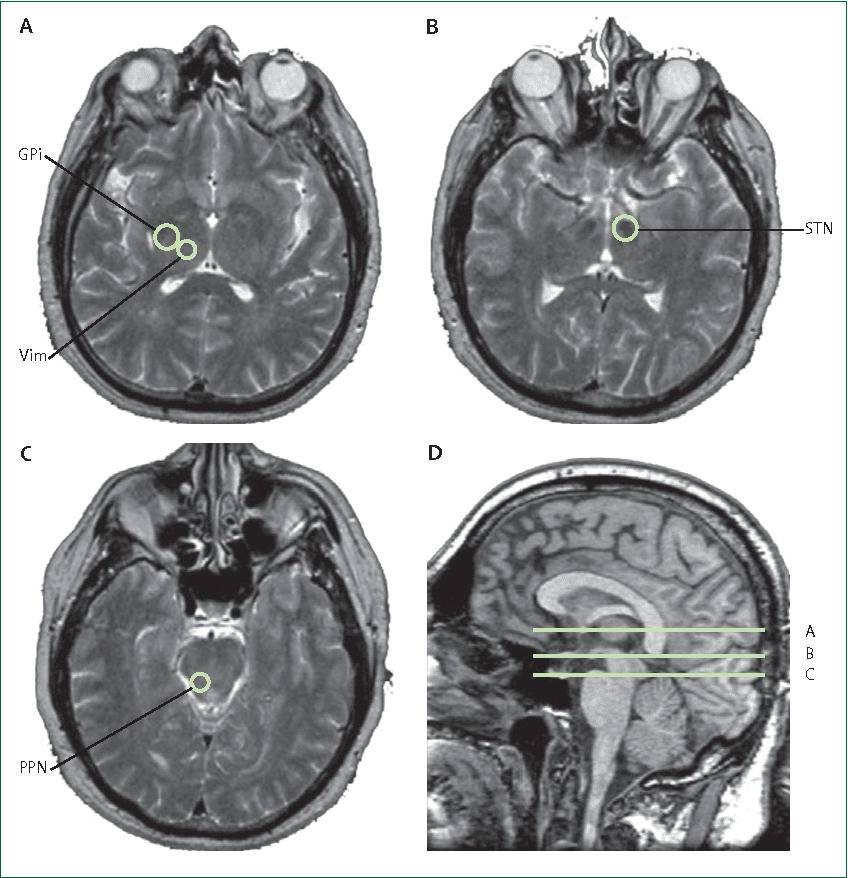
DBS of the subthalamic nucleus is an effective treatment for motor symptoms not controlled by medical therapy in advanced PD . STN-DBS has been associated with improvements in sleep architecture , urodynamics , constipation and also nonmotor fluctuations particularly sensory, dysautonomic and cognitive fluctuations . There has been concern regarding the effect of DBS on global cognition but any deterioration appears modest in very carefully selected patients . The most common complications are decreased verbal fluency and mild impairments in executive function and memory . The effect of STN-DBS on neurobehavioural symptoms is more contentious with both improvements and deleterious effects reported on depression, anxiety, apathy, impulse control disorder and dopamine dysregulation syndrome . Suicide and suicidal ideation have been reported postoperatively in case reports. Factors influencing the outcome of surgery include presurgical comorbidities, e.g. cognitive impairment, psychiatric or personality disorder, surgical issues such as target selection and postoperative management, as well as psychosocial adjustment to a major life event and natural disease progression. A full discussion of the effects of DBS on NMS is outside the scope of this contribution: Lim and colleagues provide a full review .
Depression And Parkinsons Disease
Depression is a common problem in patients with Parkinsons disease. Prevalence rates have been reported from 11% to 44% depending upon the presence of minor or major depressive symptoms and the assessment scales used. Prevalence of 31% was reported in a recent meta-analysis.
The manifestations include apathy, psychomotor retardation, memory impairment, pessimism, irrationality, and suicidal ideation without suicidal behaviour. Depression has been strongly related to the patients quality of life in Parkinsons disease.
The symptoms of depression in Parkinsons disease vary slightly from the typical symptom profile of primary depression. Depressed parkinsonian patients experience less guilt and self reproach and more irritability, sadness, and concern with health. Depression associated with agitation creates additional functional incapacity to which young onset parkinsonian patients appear particularly prone.
Mood fluctuations can accompany motor fluctuations of on-off states. Depression increases in the off state and improves in the on state. Completed suicide appears to be rare in the Parkinson population even though verbalised suicidal ideation is not uncommon. Younger onset patients appear to be more at risk for suicide and suicidal gestures than older patients. Severe depression in Parkinsons disease may anticipate the development of intellectual impairment. Depression may also present as pseudodementia that resolves with effective treatment of the depression.
Cognitive Impairment And Dementia
Cognitive impairment is common in PD even from the early stages. Specific deficits include set switching difficulty, impaired executive function and reduced verbal fluency and visuospatial abilities . Many patients with mild cognitive deficit will develop dementia as the disease progresses and the point prevalence overall in PD is around 30% with the incidence rate increased four to six times as compared with controls . In the Sydney cohort follow-up study, 83% of the survivors were diagnosed with dementia at 20 years . Established risk factors for early dementia are old age, severity of motor symptoms , mild cognitive impairment and visual hallucinations . Genetic factors may also be pertinent. The CamPaIGN longitudinal study of cognitive impairment and dementia recently reported that age > 72 years, reduced semantic fluency and inability to copy an intersecting pentagons figure, were significant predictors of dementia at 5 years. The microtubule-associated protein tau H1/H1 genotype was associated with increased risk of dementia at 5 years with functional effects on tau transcription. In contrast, COMT genotype had no effect on dementia but was associated with effects on frontostriatal function which may have a more dopaminergic basis and better prognosis.
Glutamatergic overactivity may also play a part in cognitive decline in PD. Memantine is a low affinity N-methyl D-aspartate antagonist drug which has shown promise in the treatment of PD dementia in a short-term study .
You May Like: Foods That Prevent Parkinson’s Disease
Mixed Kernel Svr Addressing Parkinsons Progression From Voice Features
-
Contributed equally to this work with: Roberto Bárcenas, Ruth Fuentes-García, Lizbeth Naranjo
Roles Conceptualization, Data curation, Formal analysis, Investigation, Methodology, Software, Validation, Visualization, Writing original draft, Writing review & editing
* E-mail:
Affiliation Departamento de Matemáticas, Facultad de Ciencias, Universidad Nacional Autónoma de México, Ciudad Universitaria, Mexico City, Mexico
- Ruth Fuentes-García ,
Contributed equally to this work with: Roberto Bárcenas, Ruth Fuentes-García, Lizbeth Naranjo
Roles Conceptualization, Formal analysis, Funding acquisition, Investigation, Methodology, Project administration, Resources, Supervision, Writing original draft, Writing review & editing
Affiliation Departamento de Matemáticas, Facultad de Ciencias, Universidad Nacional Autónoma de México, Ciudad Universitaria, Mexico City, Mexico
-
Contributed equally to this work with: Roberto Bárcenas, Ruth Fuentes-García, Lizbeth Naranjo
Roles Conceptualization, Funding acquisition, Investigation, Methodology, Project administration, Resources, Supervision, Writing original draft, Writing review & editing
Affiliation Departamento de Matemáticas, Facultad de Ciencias, Universidad Nacional Autónoma de México, Ciudad Universitaria, Mexico City, Mexico
Psychosis In Parkinsons Disease
Psychosis affects nearly one third of patients with Parkinsons disease. This usually manifests as vivid dreams, hallucinations, delusions, and in severe cases as confusional psychosis. It drastically reduces the quality of life for those affected. It also results in increased trauma for caregivers, an earlier transfer to a nursing home, and shorter lifespan. Although there were rare reports of hallucinations and delusions in medication-free Parkinsons disease patients before the advent of effective drug therapy, these cases are exceptionally rare. When hallucinations occur, the usual clinical context involves one of two situations. First, a medical illness can be superimposed on Parkinsons disease with resultant hallucinations that are part of the complications of infection, dehydration, or drug toxicity. These patients usually are confused and agitated in the midst of their hallucinations. Alternatively, in chronic Parkinsons disease on dopaminergic therapy, patients can gradually develop hallucinations that are usually visual in content and without marked agitation or confusion.
There may be a bimodal onset of hallucinations, with early onset associated with motor fluctuations and large doses of medication, and more commonly a late onset associated with cognitive impairment.
Abnormal dreaming and increased sleep disruption may precede the development of psychotic symptoms by weeks to months and provide an important early clue to their potential occurrence.
Recommended Reading: Evaluation For Parkinson’s Disease
Nms Presentation According To Disease Stage
Previous studies have shown that the severity of motor findings and NMS in PD patients are closely related , suggesting that the mechanisms of cellular degeneration underlying this disease parallelly affect multiple neuronal systems over time. Hence, in order to determine differences in the frequency of NMS presentation according to the degree of motor dysfunction, here we also grouped study participants according to their HY stage. As expected, we found that age at onset was higher in patients presenting at initial stages of disease, and disease duration was significatively longer in those presenting at late disease stages . Furthermore, we observed that the total number of NMS per patient increased as the HY staging progressed. Despite most patients were at HY2 stage at the moment of their enrollment, the proportion of patients presenting symptoms of the gastrointestinal tract, urinary tract, mood/cognition, cardiovascular, and sexual function NMS domains was higher in the HY 45 group . Interestingly, sleep/fatigue and attention/memory symptoms were more frequent at HY1 stage. Only difficulty in swallowing and loss of libido/hypersexuality were significatively more frequent at advanced stages of disease , whereas feeling sadness was most common at HY 3 stage .
Table 5. Frequency of NMS in PD patients according to the stage of disease.
Aetiopathology Of Dementia In Parkinsons Disease
Deficits in dopaminergic, cholinergic, and noradrenergic mechanisms have been proposed as the basis of cognitive impairment in Parkinsons disease. However, there is no direct evidence for or against this postulation. In some patients, dopaminergic drugs provide benefit in cognition when treated for off periods. In a recent study, reduced fluorodopa uptake in Parkinsons disease in the caudate nucleus was related to impairment in neuropsychological tests measuring verbal fluency, working memory, and attentional functioning . This indicates that dysfunction of the dopamine system has an impact on the cognitive impairment of patients with Parkinsons disease. Acetylcholinesterase inhibitors may be useful because of their cholinergic effects. Defective noradrenergic transmission is considered to be important for attention deficit.
You May Like: Stage 5 Parkinson’s Life Expectancy
Box : Psychosis In Parkinsons Disease
-
Psychosis affects nearly third of patients with Parkinsons disease.
-
It is usually a result of an intercurrent infection, electrolyte imbalance, or drug use .
-
Psychosis results into poor quality of life for patient and caregivers, early institutionalisation, and increased mortality.
-
Hallucinations are common manifestation of psychosis.
-
Typical neuroleptics tend to worsen Parkinsons disease and therefore should be avoided. Newer atypical neuroleptics have been shown to be effective in the management of psychosis of Parkinsons disease.
Finding The Right Treatment
The long list of Parkinson’s non-motor symptoms includes constipation, memory and thinking changes, low blood pressure, depression or anxiety, sleep problems and others. A number of therapies are available to treat Parkinson’s disease non-motor symptoms, but many patients are left wanting not responding well to therapies or seeing enough relief. Some drugs are approved by the U.S. Food and Drug Administration to treat these conditions in people with PD. Most, however, are FDA-approved for the general population but have not been studied in large numbers of people with PD. Still, doctors commonly prescribe them, and people with Parkinson’s often find them beneficial.
Here we describe Parkinson’s non-motor symptom treatments. With all Parkinson’s symptoms, discuss treatment options with your doctor and work together to find a regimen that fits your needs.
Dementia
Parkinson’s disease dementia is when memory or thinking changes interfere with a person’s job, daily activities or social interactions.
Also Check: Trichloroethylene And Parkinson’s Disease
There Are Many Simple Non
- Wearing compression socks
- Elevating your legs when sitting
- Drinking more fluids
- Increasing your salt intake
- Elevating the head of your bed by 30 degrees
A physical therapist can also show you exercises to reduce the problems of dizziness when you stand. Since your heart also helps control blood pressure, it is important to discuss lightheadedness or dizziness with your physician.
While psychosis is usually associated with mental disorders like schizophrenia, sometimes Parkinsons itself or side effects of medications can change your perception of reality resulting in Parkinsons psychosis. Estimates suggest as many as 40% of people living with Parkinsons may experience some type of psychosis.
Parkinsons psychosis typically takes the form of hallucinations , delusions or both. Hallucinations and delusions are more common in people who have been living with Parkinsons for a long time. Some people are aware that what they are experiencing is not actually real, while others are not.
Hallucinations in Parkinsons can be common, especially during later stages of living with it. Often, they are non-threatening visual hallucinations or visions of things that are not really there.
Weakening Sense Of Smell And Taste
This may be due to degeneration of the anterior olfactory nucleus and olfactory bulb, one of the first parts of the brain affected by Parkinsons. This can happen so gradually that youre not even aware of it.
Losing your sense of smell and taste can make you lose interest in food. You may miss out on important nutrients and lose weight.
Also Check: Ok Google Parkinson’s Disease
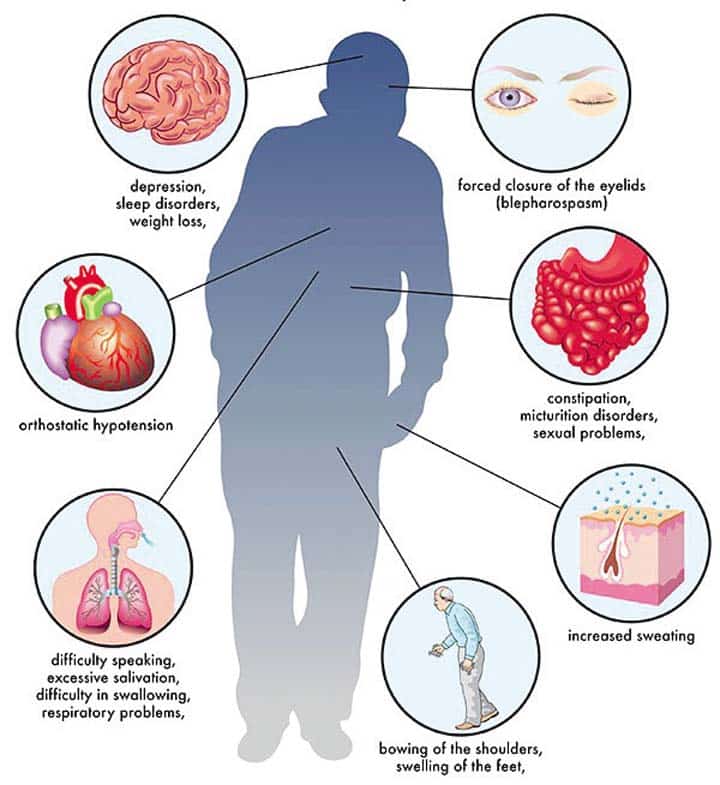
Nonmotor Symptoms Of Parkinsons Disease
Parkinsons disease is a neurodegenerative disorder of the brain and central nervous system that most people recognize by its motor symptoms, which include tremors, muscle rigidity, impaired balance, and slowness of movement . Many Parkinsons patients, however, also develop nonmotor symptoms, which ultimately may be even more disabling.
Such nonmotor symptoms can include depression and anxiety, sleeping problems, fatigue, and cognitive changes.
While these symptoms do not affect movement, coordination, or physical tasks, they usually worsen over time and can make managing the disease more difficult. Some nonmotor symptoms of Parkinsons also can begin years before a person is diagnosed with the disease.
Parkinsons motor and nonmotor symptoms often are considered as separate problems. But its important to note that these symptoms can overlap and affect each other, informing each persons disease experience. For example, problems with the muscles that control the mouth and throat a motor symptom can lead to complications that arent directly motor-related, such as excessive drooling and difficulties with speech.
Sudden drops in blood pressure another nonmotor symptom can lead to dizziness and, in extreme cases, to a loss of balance that can cause falls.
The following are the main nonmotor symptoms of Parkinsons:
Looking For An Inspection Copy
This title is not currently available on inspection
-
Non-motor Parkinson’s Disease is a burgeoning area of the movement disorders field, as patients increasingly live longer and encounter more late-stage symptoms. The spectrum of non-motor manifestations spans much of the body, with non-motor features occurring in all stages of the disease. Identification of symptoms is key for preserving quality of life and successful treatment. This is a practical manual on all aspects of pre-motor and non-motor manifestations of Parkinson’s. The genetic causes of non-motor symptoms are detailed and methods of patient evaluation summarized. Topics such as autonomic and sexual dysfunction, mood disorders, and drug-induced symptoms of non-motor Parkinson’s are covered in depth. This is an essential resource for movement disorder specialists, neurologists and other clinicians involved in caring for those with Parkinson’s disease.
- Brings together vital information about non-motor symptoms that has previously only been accessible in disparate sources
- Covers specific symptoms, their pathophysiology, neuroimaging and treatment along with general information on the genetic background of the disease and how to evaluate patients
- A practical manual with advice suitable for all involved in the care of patients with Parkinson’s disease, including movement disorder specialists, neurologists, primary care providers and cardiologists
Review was not posted due to profanity
Also Check: New Cure Parkinson’s Disease
There Are Different Ways To Address Mood Changes Including:
- Taking medications
- Changing medications that have mood-related side effects
- Exercising regularly
Identify mood triggers, add positive energy into your daily life and provide a way to talk with your doctor and healthcare team about treating depression with the help of our Depression Worksheet.
Parkinsons can have many different effects on your sleep, including trouble falling or staying asleep, vivid dreams, waking up frequently during the night and excessive sleepiness during the day. Like other non-motor symptoms, sleep problems can appear before the motor symptoms.
An estimated 30% of people with Parkinsons experience some combination of insomnia and sleep fragmentation . Studies have shown people with Parkinsons have different sleep patterns and that their deepest periods of sleep during the night are shorter and interrupted more often than people without Parkinsons. Often this is made worse by medications that may wear off in the night, causing tremor, painful stiffness or other symptoms to return and disrupt your sleep.
Anxiety, depression nighttime sweating and trouble moving in bed are other non-motor symptoms of Parkinsons that can make getting a good sleep difficult. Fragmented sleep is also exacerbated by how often some people with Parkinsons find themselves waking up often during the night to use the toilet because of the changes in the bladder that come with Parkinsons.
What You Can Do Right Now To Live Well
An evaluation by a neuropsychologist, a specialist trained in measuring thinking and behavioral functions, can help identify cognitive difficulty or dementia. Neuropsychological testing measures thinking abilities such as concentration, attention, memory, language abilities, abstract thinking, spatial skills and executive functions and can help your physician determine what could be causing thinking problems.
Some people experience improvements in cognitive function when they take certain medications or even change their current medications. Talk with your physician about which medications might work for you.
Physical exercise has also been proven to help not just the body, but the brain. Exercise can improve cognitive function as well as reduce the long-term risk of dementia.
Our Brain Health & Memory Worksheet includes more ways to maintain cognitive functions like memory, planning and problem-solving.
Parkinsons impact on emotions and mood are often overlooked because they are complicated and harder to talk objectively about than physical symptoms. While a Parkinsons diagnosis itself can bring feelings of grief and anxiousness for the future, there are also biological changes caused by Parkinsons that can result in mood changes such as anxiety, apathy and depression.
Depression, anxiety and apathy can have a significant impact on you and your familys quality of life.
You May Like: Parkinson’s And Stem Cell Treatment
Impulse Control Disorder And Dopamine Dysregulation Syndrome
A wide range of impulsive and compulsive behaviours such as pathological gambling, hypersexuality, compulsive shopping and binge eating likened to behavioural addictions have been reported in PD patients in the last decade and are usually triggered by dopaminergic therapy particularly dopamine agonists . Repetitive purposeless behaviours known as punding or excess hobbyism are also recognized. These behaviours may affect up to 14% of patients and are often covert and undeclared to family members and health professionals . The recent SIGN guideline highlights the need to warn patients and families of these iatrogenic NMS prior to initiation of therapy. Practitioners need to remain vigilant throughout the treatment course as these features may emerge some time after the introduction of treatment. Optimal management remains uncertain but reduction or withdrawal of dopamine agonists with a shift to levodopa-based therapy is associated with improvement in the majority, but not all cases .