Major Findings Of Present Work
In this study, we compared cognitive and motor symptoms of patients with mild DLB and PDD. The main finding was that DLB patients showed more attention/executive and visuoconstructive deficits as compared to PDD patients. The logistic regression analysis was able to correctly classify 88.2% of the patients with DLB or PDD, based on the cognitive profile. The strongest predictor of diagnostic category was the variable pentagon drawing. Additionally, PDD patients demonstrated more significant motor deterioration based mostly on dopaminergic symptoms compared to DLB patients.
Recommended Reading: Signs And Symptoms Of Early Parkinsons Disease
Building A Lewy Body Dementia Care Team
After receiving a diagnosis, a person with LBD may benefit from seeing a neurologist who specializes in dementia and/or movement disorders. Your primary doctor can work with other professionals to follow your treatment plan. Depending on an individuals particular symptoms, physical, speech, and occupational therapists, as well as mental health and palliative care specialists, can be helpful.
Support groups are another valuable resource for people with LBD and their caregivers. Sharing experiences and tips with others in the same situation can help people find practical solutions to day-to-day challenges and get emotional and social support.
Lewy Bodies: More Than Lbd
LBD is characterized by the presence of Lewy bodies in the nerve cells of the brain, meaning that LBD patients have Lewy bodies in the brain.2 However, Lewy bodies are also common with other conditions, such as Alzheimers and Parkinsons disease. In fact, most people with PD also have Lewy bodies in their brain. However, even if they have Lewy bodies, not all Parkinsons patients will also develop LBD.2
Read Also: Medications For Tremors In Parkinson’s
Behavioral And Mood Symptoms Of Lewy Body Dementia
Changes in behavior and mood are possible in LBD and may worsen as the persons thinking abilities decline. These changes may include:
- Depression
- Apathy, or a lack of interest in normal daily activities or events and less social interaction
- Anxiety and related behaviors, such as asking the same questions over and over or being angry or fearful when a loved one is not present
- Agitation, or restlessness, and related behaviors, such as pacing, hand wringing, an inability to get settled, constant repeating of words or phrases, or irritability
- Delusions, or strongly held false beliefs or opinions not based on evidence. For example, a person may think his or her spouse is having an affair or that relatives long dead are still living.
- Paranoia, or an extreme, irrational distrust of others, such as suspicion that people are taking or hiding things
Treatments For Parkinsons Disease Dementia And Dementia With Lewy Bodies
Treatments for DLB are similar to PDD and are aimed at symptom control. The motor symptoms of slowness, stiffness and walking difficulties can be treated with Levodopa. However, Levodopa can cause or exacerbate hallucinations, making it difficult to use it as a treatment for patients who have or are at risk of having hallucinations. Sometimes, clinicians will need to treat the hallucinations more aggressively in order for a patient to tolerate Levodopa given to help the motor symptoms. On the flipside, anti-psychotic medications to control hallucinations can worsen motor symptoms, so treating all the symptoms of LBD simultaneously can be a tricky balancing act.
Recommended Reading: Parkinson’s And Memory Loss
Genetics Of The Lewy Body Dementias
A number of genetic mutations have been associated with DLB and PDD, which are interesting clinically but also hold promise to elucidate fundamental mechanisms of disease. Some genetic errors appear to be dose dependent. For example, mutation or duplication of -synuclein causes autosomal dominant PD, but triplication is often associated with both parkinsonism and dementia.40 Several other genes also confer risk for DLB and PDD. The most prominent of these is GBA, the gene encoding glucocerebrosidase.41,42 While double mutations of GBA cause Gaucher disease , single GBA mutations are associated with DLB as well as with a variant of PD that carries an increased risk of cognitive impairment. Not all PD-related genes confer such risk, however. For example, the LRRK2 mutation causes autosomal dominant PD without cognitive impairment.43 In addition, a small number of genes have been identified that carry risk for DLB but not PDD, including the apolipoprotein E 4 allele.44 Mutations in the MAPT gene, which have been associated with the tauopathies such as FTD with parkinsonism, and in the COMT gene, have also been variably observed in PDD.45 In patients with a strong family history, genetic counseling should be provided and genetic studies should be considered.
Parkinson’s Dementia Vs Dementia With Lewy Bodies
Have you ever wondered if there was any difference between dementia with Lewy bodies and Parkinson’s disease dementia? If you’ve ever heard the symptoms of these two disorders, they sound surprisingly alike. That’s because they’re both types of Lewy body dementia: dementia with Lewy bodies and Parkinson’s disease dementia .
Recommended Reading: Parkinson’s Getting Out Of Bed
Diagnostic Criteria For Parkinson Disease Dementia
Consensus criteria for PDD were developed in 2007 .6,29 These criteria require cognitive impairments across multiple domains but emphasize that noncognitive features such as hallucinations are common. As described previously in the article, the clinical and neuropsychological features of DLB and PDD are similar. Indeed, it is the relative timing of dementia and parkinsonism that defines the clinical distinction between DLB and PDD. Controversy exists over how or whether to distinguish these syndromes.30
Parkinsons Disease And Lewy Body Dementia Explained
- Learn more about Parkinsons disease and Lewy body dementia. These degenerative brain disorders are caused by abnormal clumps of protein called Lewy bodies.
Parkinsons disease and Lewy body dementia are degenerative brain disorders. Both diseases are linked to protein deposits in the nerve cells of the brain known as Lewy bodies.
The two disorders have similar symptoms. People with LBD may experience tremors and muscle stiffness like those who have Parkinsons. And, while Parkinsons disease affects motor function, about 40% of people with Parkinsons also develop dementia as the disease advances.
Heres a closer look at the connection between Parkinsons disease and Lewy body dementia.
You May Like: The Last Stages Of Parkinson’s Disease
Difference Between Parkinsons Disease Dementia And Dementia With Lewy Bodies
Technically, the difference between these two conditions lies in how quickly the cognitive difficulties and hallucinations develop in relation to the movement issues. In DLB, the cognitive difficulties and hallucinations develop much sooner in the disease course than in PDD, sometimes even prior to the movement difficulties. Because of the similarities between PD, PDD, and DLB, current thinking in the medical community is that they should be viewed as related diseases which fall along a continuum of Lewy body disorders.
APDAParkinsons Disease SymptomsLewy Bodies, Dementia, and Parkinsons What Does it all Mean?
Here are two common scenarios that may sound familiar:
Scenario 1A patient develops a series of neurologic symptoms, is evaluated by a neurologist and is told that she has Parkinsons disease . She then visits another neurologist for a second opinion and is told she has Lewy Body Dementia .
Scenario 2A patient has his first visit with his neurologist and is told that he has PD, at a subsequent visit the diagnosis is changed to Parkinsons disease dementia , and at a follow up visit the diagnosis is changed yet again to Dementia with Lewy Bodies .
Both of these situations understandably cause great uncertainty and frustration.
Parkinsons Disease With Dementia Versus Dementia With Lewy Bodies
Some patients with Parkinsons disease experience no or only subtle cognitive decline, and their primary limitation is their motor disorder. However, other patients with Parkinsons disease develop dementia as a consequence of the disease. When dementia develops after an established motor disorder, we call the disease Parkinsons disease with dementia . In contrast, when dementia develops prior to or at the same time as the motor disorder, we call the disease DLB. Although the initial sequence of symptoms differs in PDD and DLB, as the disorders progress, the symptoms and the underlying brain changes are much more similar than they are different. As such, many researchers and clinicians think of PDD and DLB as being on a continuum of a similar disease process rather than as two distinct entities.
Don’t Miss: Does Parkinson’s Disease Affect The Mind
Degeneration In The Mesocortical Dopamine Network Contributes To Executive Dysfunction
However, dopamine-dependent neural circuitry underlying executive deficits in Parkinsons disease may not be limited to the fronto-striatal network alone. The mesocortical dopamine network originates in the midbrain ventral tegmental area and projects diffusely to neocortical areas, particularly prefrontal, insular and cingulate cortices . Release of dopamine from this network modulates prefrontal D2 receptors and thereby facilitates cognitive flexibility, a core feature of executive processing . Insular cortex in particular is considered to mediate such flexibility, acting as a hub to recruit other cognitive circuits such as the fronto-parietal network . In support of this, insular lesions in human patients have been shown to impair performance on tasks requiring cognitive flexibility .
Also Check: Hoarse Voice Parkinsons Disease
What Is Dementia With Lewy Bodies
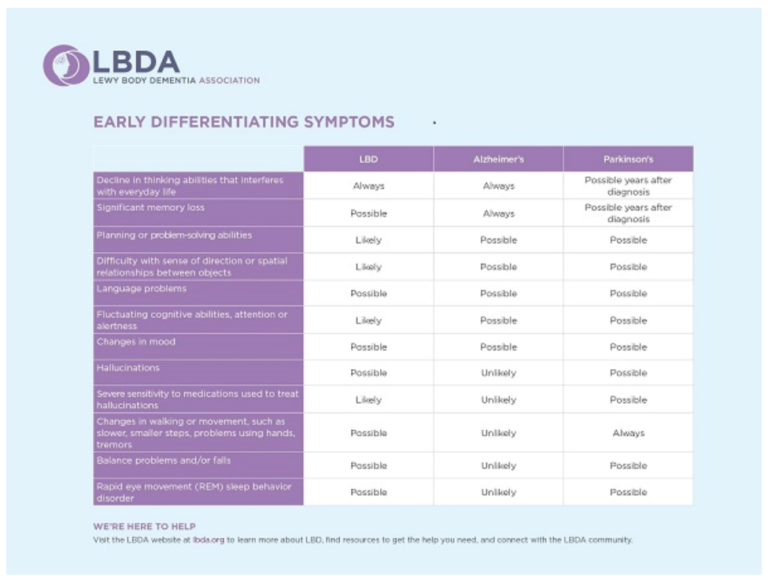
Dementia with Lewy bodies inhibits everyday activities by causing memory and thinking problems, specifically targeting problem-solving, planning, and visual learning abilities. In contrast to PDD, dementia usually always appears first or around the same time as parkinsonism) in patients with DLB. The motor symptoms of Parkinsons come as the disease progresses.
The main difference between Parkinsons disease and dementia with Lewy bodies is the timeline of the symptom onset. With Parkinsons, onset of symptoms usually happens gradually over years of having the illness. However, with Lewy body dementia, the onset of symptoms is much more aggressive, rapidly affecting patients within a year of diagnosis.
Also Check: Antipsychotics In Parkinson’s Disease
Treatment Of Motor Symptoms In Parkinsons Disease
Treatment of motor, psychological/psychiatric, and autonomous symptoms of Parkinsons disease should be symptomatic, depending on the degree of clinical impairment and independently of a diagnosis of dementia with Lewy bodies or Parkinsons disease dementia. Attention needs to be paid to the reduced response of motor symptoms, especially akinesis, to levodopa in 40% of patients with Lewy body dementia. Owing to the development of the dementia and the tendency to develop psychoses in dementia with Lewy bodies, monotherapy with levodopa is usually recommended. Studies of combination treatment with dopamine agonists and levodopa have not been conducted in patients with Lewy body dementia whether combination treatment with dopamine agonists is useful and tolerable depends on the individual case. This requires consideration, especially bearing in mind the patients age . Close monitoring for possible psychotic symptoms is urgently advised. The administration of anticholinergic drugs is contraindicated.
Living With Parkinson Disease
These measures can help you live well with Parkinson disease:
- An exercise routine can help keep muscles flexible and mobile. Exercise also releases natural brain chemicals that can improve emotional well-being.
- High protein meals can benefit your brain chemistry
- Physical, occupational, and speech therapy can help your ability to care for yourself and communicate with others
- If you or your family has questions about Parkinson disease, want information about treatment, or need to find support, you can contact the American Parkinson Disease Association.
You May Like: Average Age Of Parkinsons Onset
Read Also: Can Blows To The Head Cause Parkinson Disease
What Other Things Help
There are various ways to help a person with DLB. Speech therapy may help improve communication between people with DLB and others. Physical therapy may help strengthen and stretch stiff muscles and help to prevent falls.
Research has shown that physical exercise helps to enhance brain health and improves mood and general fitness. A balanced diet, enough sleep, and limited alcohol intake are other important ways to promote good brain health. Other illnesses that affect the brain, such as diabetes, high blood pressure, and high cholesterol, should also be treated if present.
Comparing Disorders And Subtypes
The following table provides a brief summary of the differences among atypical parkinsonism disorders. Most exhibit parkinsonism symptoms some exhibit dementia symptoms each is identified by specific mis-folded proteins visible in the brain upon autopsy.
Atypical parkinsonism disorders are difficult to diagnose because there is no chemical test of blood or tissue, there is no imaging test, and the various disorders have similar symptoms and even share symptoms with non-parkinsonism disorders.
When a Board-certified neurologist delivers a diagnosis for any of the four atypical [arkinsonism disorders, the probability that the diagnosis is incorrect is approximately 50%. The only way to definitively diagnose an atypical parkinsonism disorder is by postmortem microscopic analysis of brain tissue.
| Atypical Parkinsonism Disorder |
|---|
Recommended Reading: Early Indications Of Parkinsons Disease
Also Check: Stabilizing Spoon For Parkinson’s
How Can We Manage Hallucinations
It may not be necessary to treat all hallucinations of a person with DLB. Hallucinations are often harmless, and it is okay to allow them to happen, as long as they are not disruptive or upsetting to the person or his/her surroundings. Sometimes, recognizing the hallucination and then switching the topic might be an efficient way of handling frustrations that occur because of a hallucination. If hallucinations need medical treatment, your provider may be able to discuss and suggest some options. However, most medications used to treat hallucinations may make movement symptoms worse.
Are There Medicines To Treat Dlb
Though there is no cure for DLB yet, there are medications that help manage the symptoms. These medications are called cholinesterase inhibitors, and they can help if a person with DLB is having memory problems. Some examples of these medicines are donepezil, rivastigmine and galantamine. If a person with DLB has movement symptoms they may be treated with medications used for Parkinsons disease, such as levodopa. Sleep problems may be managed by sleep medications including melatonin.
Because people with DLB are usually very sensitive to medications, any new medication, even one that is not being used for the brain, needs to be reviewed with the persons provider to avoid potential contraindication.
Also Check: Cognition And Parkinson’s Disease
Fluctuations Of Attention And Arousal
Attention and alertness may fluctuate, leading to episodes of staring and perturbed flow of ideas, or to frequent daytime drowsiness and naps during the day. These episodes can be hard to quantify and need to be disentangled from toxic metabolic processes such as medication side effects or infections. A recent fluctuations scale vetted for this purpose is the Dementia Cognitive Fluctuation Scale,13 which aggregates prior scales. The fluctuations screen requires a positive response to at least three of the following: Does the patients inability to organize thoughts in a coherent way vary significantly over the course of the day? Does the patient spend more than 1 hour sleeping during the waking day? Is the patient drowsy and lethargic for more than 1 hour during the day, despite getting the usual amount of sleep the night before? Is the patient difficult to arouse on a usual day? This approach had a sensitivity of 80% and a specificity of 76% in differentiating clinical syndromes of DLB and PDD from AD and vascular dementia, but has yet to be neuropathologically validated.
What Is Parkinsons Disease Dementia
Parkinsons disease dementia is a term specifically used for those who have suffered with Parkinsons for multiple or several years and eventually develop dementia. Almost always in the early stages of Parkinsons, patients will experience inhibited motor skills and even sometimes cognitive change. Non-motor symptoms of Parkinsons may appear over time, such as memory loss, anxiety, fatigue, cognitive dysfunction, and more. However, not all individuals who are diagnosed with Parkinsons will receive a dementia diagnosis, and it is not yet possible to determine which Parkinsons patients will develop dementia as well.
Read Also: Parkinson’s Disease Foundation Grants
Causes Of Lewy Body Dementia
LBDs are poorly understood but are thought to be characterized by the buildup of Lewy bodies in the brain. Lewy bodies are groupings or clumps of badly formed proteins called alpha-synuclein proteins. Healthy alpha-synuclein proteins are normally found widely throughout the brain and are thought to play many roles, including participating in plasticity. This means that they affect how brain cells communicate with one another and change in response to a persons experience. However, when these proteins misfold and accumulate, the result is Lewy bodies, which lead to cell death in the brain.
The type of LBD a person has is determined by where in the brain the Lewy bodies first begin forming. When Lewy bodies first begin to form in the cortex, dementia with Lewy bodies is the most likely result. These initial protein deposits in the cortex lead to early cognitive changes, such as inattention. When the Lewy bodies first deposit in areas of the brain more related to motor control and movement, such as the substantia nigra, PDD is the most likely result.
But what causes these Lewy bodies to form in the first place?
Genetics or hereditary elements likely play a role. The following genes are thought to be involved in the spectrum of disorders related to PD, including dementia with Lewy bodies and PDD.
- APOE
APDAParkinsons Disease SymptomsLewy Bodies, Dementia, and Parkinsons What Does it all Mean?
Here are two common scenarios that may sound familiar:
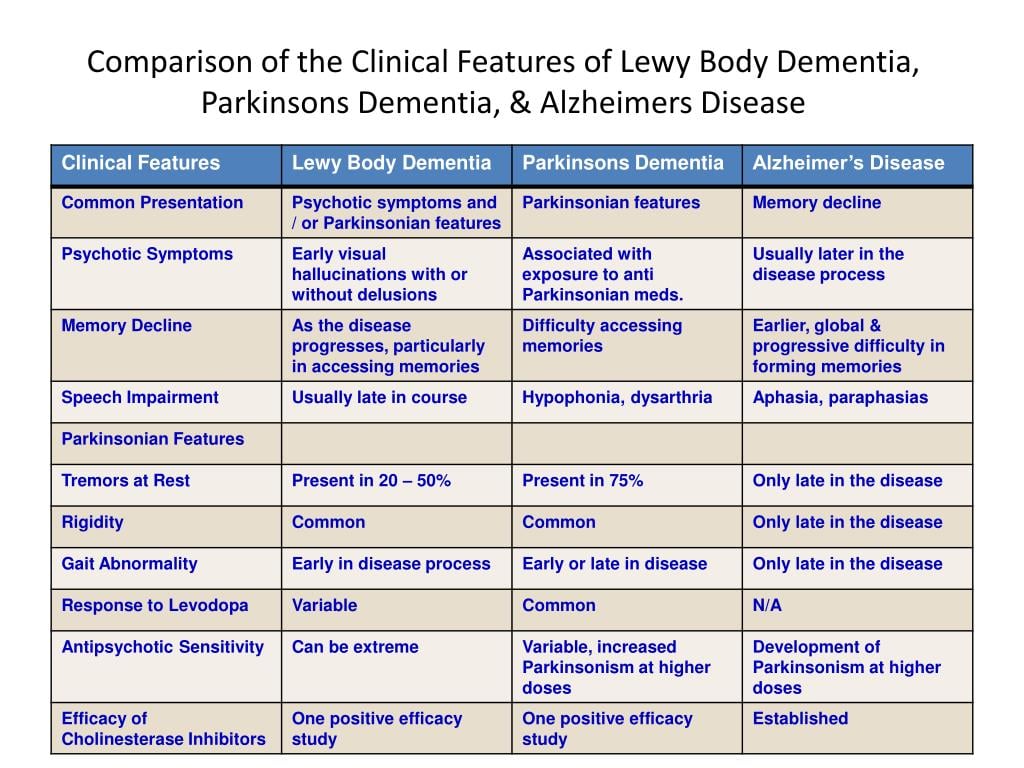
Whats The Difference Between Lewy Body Dementia Parkinsons Disease And Alzheimers Disease
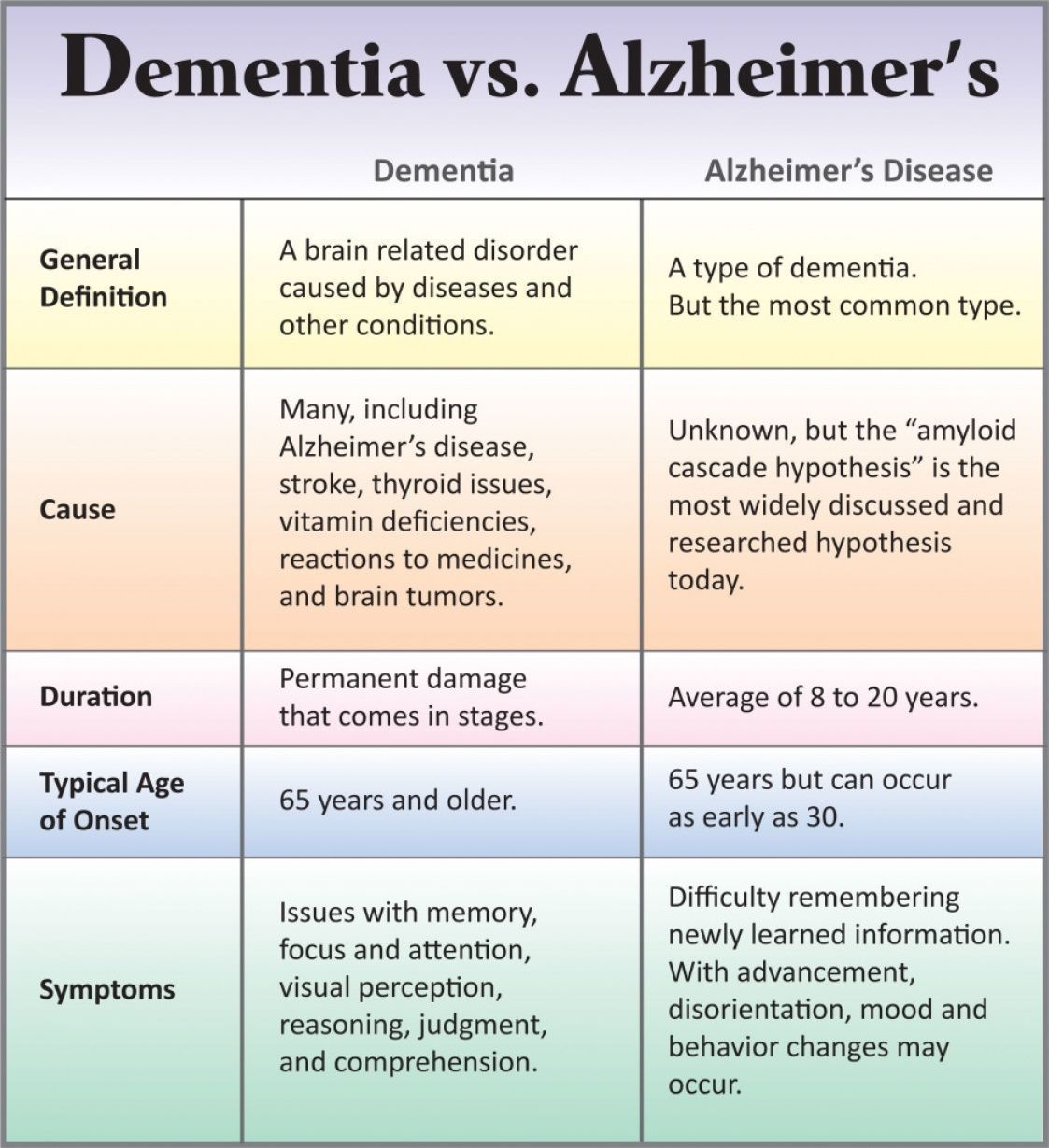
Lewy body dementia is an umbrella term for two related clinical diagnoses: dementia with Lewy bodies and Parkinsons disease dementia. These disorders share the same underlying changes in the brain and very similar symptoms, but the symptoms appear in a different order depending on where the Lewy bodies first form.
Dementia with Lewy bodies is a type of dementia that causes problems with memory and thinking abilities that are severe enough to interfere with everyday activities. It specifically affects a persons ability to plan and solve problems, called executive function, and their ability to understand visual information. Dementia always appears first in DLB. The motor symptoms of Parkinsons such as tremor, slowness, stiffness and walking/balance/gait problems usually become more evident as the disease progresses. Visual hallucinations, REM sleep behavior disorder, fluctuating levels of alertness and attention, mood changes and autonomic dysfunction are also characteristic of DLB.
Finally, Alzheimers is characterized by different abnormal clumps called amyloid plaques, and jumbled fiber bundles called tau tangles. These microscopic structural changes in the brain were discovered by Dr. Alois Alzheimer in 1906. These plaques and tangles, together with loss of connections between nerve cells, contribute to loss of coherence and memory, as well as a progressive impairment in conducting normal activities of daily living.
Recommended Reading: Boyd Gaines Parkinson’s Disease