Building A Lewy Body Dementia Care Team
After receiving a diagnosis, a person with LBD may benefit from seeing a neurologist who specializes in dementia and/or movement disorders. Your primary doctor can work with other professionals to follow your treatment plan. Depending on an individual’s particular symptoms, physical, speech, and occupational therapists, as well as mental health and palliative care specialists, can be helpful.
Support groups are another valuable resource for people with LBD and their caregivers. Sharing experiences and tips with others in the same situation can help people find practical solutions to day-to-day challenges and get emotional and social support.
What You Need To Know
- Lewy body dementia is a form of progressive dementia that affects a persons ability to think, reason, and process information.
- Diagnosing Lewy body dementia can be challenging an estimated 1.4 million Americans are living with the disease.
- LBD has three features that distinguish it from other forms of dementia:
- Fluctuating effects on mental functioning, particularly alertness and attention, which may resemble delirium
- Recurrent visual hallucinations
- Parkinson-like movement symptoms, such as rigidity and lack of spontaneous movement.
Lewy bodies are clumps of abnormal protein particles that, for reasons that are not fully understood, accumulate in the brain. These deposits cause a form of dementia called Lewy body dementia, or LBD which is what the late actor and comedian Robin Williams suffered from.
LBD is not the same as Parkinsons, but the two are closely related: LBD causes some or all of the motor symptoms of Parkinsons. More than 1 million people in the U.S. are affected by Lewy body dementia, according to the Lewy Body Dementia Association.
Number Of People Affected
Parkinsons disease is thought to affect about 2 percent of Americans over 65. Of those, about 50 to 80 percent will go on to develop Parkinsons-related dementia.1 The Parkinsons Foundation estimates that nearly 1 million Americans will be living with Parkinsons by 2020. The disease affects 1.5 times more men than women.7
Approximately 5.8 million Americans are currently living with Alzheimers disease. That number is expected to increase to 14 million by 2050.8 There is little difference between numbers of men and women who develop Alzheimers, but there are more women with the disease, because women tend to live longer than men.3
Also Check: Medications For Parkinson’s Patients
What Causes Lewy Body Dementia
The causes of LBD are not yet well understood, but research is ongoing in this area. There are probably multiple factors involved, including genetic and environmental risk factors that combine with natural aging processes to make someone susceptible to LBD.
For more information, visit www.lbda.org.
Modified with permission from the Lewy Body Dementia Association
To learn more about motor symptoms related to Parkinsons, visit here.
To learn more about non-motor symptoms related to Parkinsons, visit here.
Comparing Disorders And Subtypes
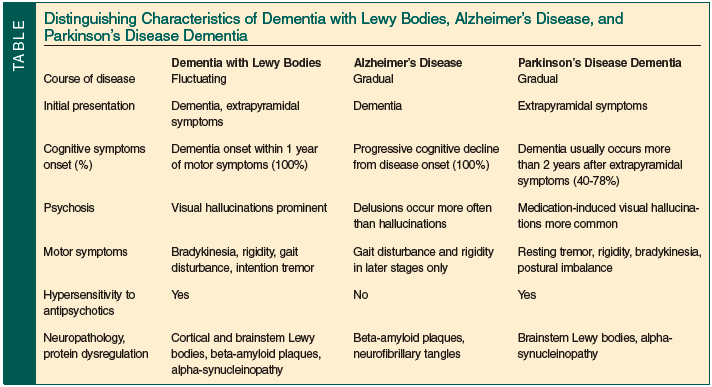
The following table provides a brief summary of the differences among atypical parkinsonism disorders. Most exhibit parkinsonism symptoms some exhibit dementia symptoms each is identified by specific mis-folded proteins visible in the brain upon autopsy.
Atypical parkinsonism disorders are difficult to diagnose because there is no chemical test of blood or tissue, there is no imaging test, and the various disorders have similar symptoms and even share symptoms with non-parkinsonism disorders.
When a Board-certified neurologist delivers a diagnosis for any of the four atypical [arkinsonism disorders, the probability that the diagnosis is incorrect is approximately 50%. The only way to definitively diagnose an atypical parkinsonism disorder is by postmortem microscopic analysis of brain tissue.
| Atypical Parkinsonism Disorder |
|---|
Recommended Reading: Early Indications Of Parkinson’s Disease
Treatment And Care For Lewy Body Dementia
While LBD currently cannot be prevented or cured, some symptoms may respond to treatment for a period of time. An LBD treatment plan may involve medications, physical and other types of therapy, and counseling. A plan to make any home safety updates and identify any equipment can make everyday tasks easier.
A skilled care team often can suggest ways to improve quality of life for both people with LBD and their caregivers.
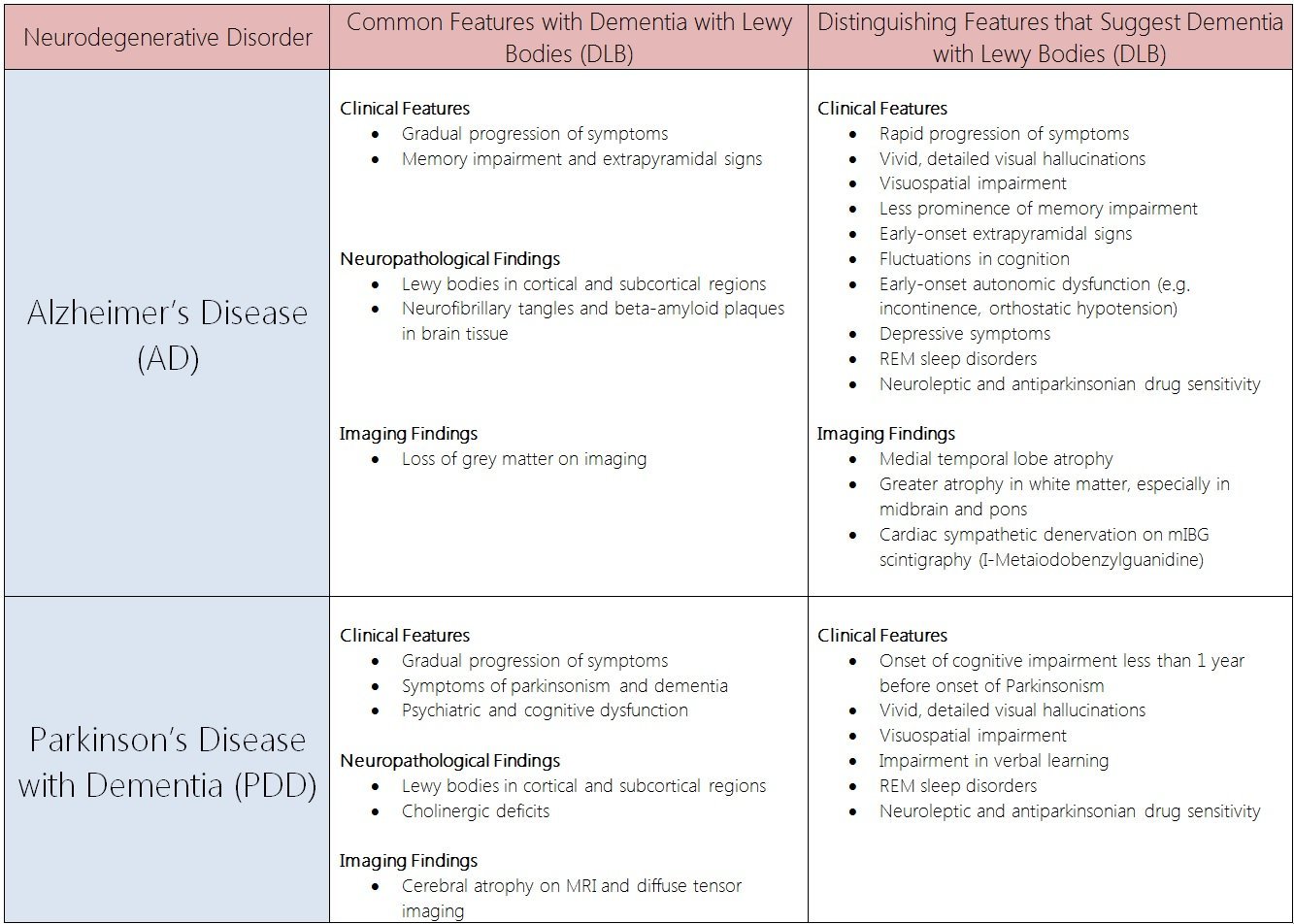
Major Findings Of Present Work
In this study, we compared cognitive and motor symptoms of patients with mild DLB and PDD. The main finding was that DLB patients showed more attention/executive and visuoconstructive deficits as compared to PDD patients. The logistic regression analysis was able to correctly classify 88.2% of the patients with DLB or PDD, based on the cognitive profile. The strongest predictor of diagnostic category was the variable pentagon drawing’. Additionally, PDD patients demonstrated more significant motor deterioration based mostly on dopaminergic symptoms compared to DLB patients.
Recommended Reading: Signs And Symptoms Of Early Parkinson’s Disease
Robin Williams Would Have Been 70 This Year Here’s What We Know About Lewy Body Dementia Suicide And Parkinson’s
On July 21, actor and comedic genius Robin Williams would have turned 70. Williams not only amplified and brought awareness to the life-changing, prevalent disease known as Lewy Body Dementia, but his passing brought much needed attention to the importance of mental health and the non-movement symptoms of depression and anxiety that can accompany a neurodegenerative disease.
Nearly seven years after his passing, what do we know about Lewy Body Dementia? How can we help people with a neurological disease experiencing suicidal thoughts?
Dementia With Lewy Bodies Without Parkinsonism
I agree with the proposal of new criteria for the diagnosis and management of dementia with Lewy bodies . Previous criteria did not adequately differentiate DLB from Parkinson disease with dementia as outlined in the article’s accompanying editorial.
Lewy body disease includes PD and DLB, thus there should be DLB without parkinsonism as well as PDD. The new criteria outlined four core clinical features: fluctuating cognition with pronounced variations in attention and alertness detailed, recurrent visual hallucinations REM sleep behavior disorder, which may precede cognitive decline and one or more spontaneous cardinal features of parkinsonism including bradykinesia, rest tremor, or rigidity. According to this criteria, a patient who has the first three clinical features but does not have parkinsonism may be diagnosed as DLB.
Braak et al. proposed that brainstem synucleinopathy progresses rostrally to affect the substantia nigra, which may cause parkinsonism. . However, these described patterns of synucleinopathy are not often observed in DLB, especially when synucleinopathy occurs in the absence of parkinsonism. Braak et al.’s hypothesis would indicate that visual hallucinations are a result of occipital dysfunction. Meanwhile, attention and alertness are due to frontal dysfunction, which does not necessarily follow Braak’s hypothesis. In addition, DLB patients with predominantly frontal dysfunction may not have parkinsonism.
Recommended Reading: Parkinson’s Disease How Long To Live
Deficits In Attention/executive Functions
In the domain of attention/executive functions, DLB patients performed significantly worse on digit span backward and MCST than PDD patients. In 2014, Yoon et al. also found that the attention/executive domain is more affected in DLB compared to PD even in the mild cognitive impairment stage. A recent neuroimaging study showed that numbers of categories achieved and perseverative errors in the Wisconsin Card Sorting Test should be differentially estimated, because they reflect the function of different brain regions in patients with early dementia , i.e. categories achieved mainly reflect the function of the precentral segments, whereas perseverative error scores correlate with metabolic activity in the right thalamus.
Coping With Cognitive Changes
Some medications used to treat Alzheimer’s disease also may be used to treat the cognitive symptoms of LBD. These drugs, called cholinesterase inhibitors, act on a chemical in the brain that is important for memory and thinking. They may also improve hallucinations, apathy, and delusions. The U.S. Food and Drug Administration has approved one Alzheimer’s drug, rivastigmine, to treat cognitive symptoms in Parkinson’s disease dementia. Several other drugs are being tested as possible treatments for LBD symptoms or to disrupt the underlying disease process.
Recommended Reading: What Diseases Are Similar To Parkinson’s
Parkinson’s Disease Dementia And Dementia With Lewy Bodies
The key pathological hallmark found in brains of Parkinson’s disease and Parkinson’s disease dementia patients are abnormal microscopic deposits composed of alpha-synuclein. This protein is found widely in the brain but its normal function is not yet well understood. The deposits are called “Lewy bodies”. Lewy bodies are also found in several other neurodegenerative brain disorders, including dementia with Lewy bodies . Evidence suggests that Parkinson’s disease and Parkinson’s disease dementia, and dementia with Lewy bodies, may be linked to the same underlying abnormalities in brain processing of alpha-synuclein.
Movement Problems And Lewy Body Dementia
Some people with LBD may not experience significant movement problems for several years. Others may have them early on. At first, movement symptoms, such as a change in handwriting, may be very mild and easily overlooked. Movement problems may include:
- Muscle rigidity or stiffness
You May Like: Can Vyvanse Cause Parkinson’s
Memory And Thinking Problems
You may experience forgetfulness, slowed thinking and difficulty concentrating. You might find it harder to follow conversations, and remember some words and names. This can make communication difficult.
You may also find it increasingly difficult to make decisions, plan activities and solve problems. This can make everyday activities harder.
The Difference Between Parkinson’s Disease And Lewy Body Dementia
One of the most confusing concepts to explain in the clinic is the difference between Parkinson’s Disease, Parkinson’s Disease Dementia and Lewy Body Dementia. Ultimately people with Parkinson’s can look very similar with motor and non-motor problems. This is particularly tricky when PwP first present but the easiest way to consider Lewy Body Dementia is like having a very aggressive progression of Parkinson’s where patients are dementing in the first year of their condition whereas this process is much slower when patients develop Parkinson’s Disease Dementia. Indeed, clinically Lewy Body Dementia patients look like they have a cross between Parkinson’s and Alzheimer’s, which is actually close to what is seen down the microscope when researchers study the brain. Understanding the differences between Parkinson’s Disease and Lewy Body Dementia is not only difficult for patients and their families but has led some professional groups to try and lump all of these patients together under one umbrella, which probably does little to help individual families appreciate what the future holds.
Hopefully this video will help you to gain a more complete understanding of the differences between Parkinson’s Disease, Parkinson’s Disease Dementia and Lewy Body Dementia.
_____________________________________________________________________________________
Don’t Miss: Hearing Loss And Parkinson’s
Two Of The Following Are Present :
- Fluctuating cognition: Mental problems varying during the day, especially attention and alertness.
- Visual hallucinations: Detailed and well-formed visions, which occur and recur.
- RBD: Physically acting out dreams while asleep.
A DLB diagnosis is even more likely if the individual also experiences any of the following: repeated falls, fainting, brief loss of consciousness, delusions, apathy, anxiety, problems with temperature and blood pressure regulation, urinary incontinence, and chronic constipation, loss of smell, or sensitivity to neuroleptic medications that are given to control hallucinations and other psychiatric symptoms.
Finally, the timing of symptoms is a reliable clue: if cognitive symptoms appear before or within a year of motor symptoms, DLB is more likely the cause than Parkinsonâs disease. Signs of stroke or vascular dementia usually negate the likelihood of DLB.
Testing is usually done to rule out other possible causes of dementia, motor, or behavioral symptoms. Brain imaging can detect brain shrinkage and help rule out stroke, fluid on the brain , or subdural hematoma. Blood and other tests might show vitamin B12 deficiency, thyroid problems, syphilis, HIV, or vascular disease. Depression is also a common cause of dementia-like symptoms. Additional tests can include an electroencephalogram or spinal tap .
Wait So What Is Parkinsonism
Parkinsonism refers to the motor symptoms that are typically associated with PD, such as tremors, stiffness, and walking/balance problems. Both PD and LBD are forms of Parkinsonism, meaning that PD patients and LBD patients may experience these motor symptoms.2 Because the Parkinsonism motor symptoms of PD and LBD can be very similar, it can be difficult to differentiate between the two conditions.
Recommended Reading: Symptoms Of Parkinsons In Women
What Is The Link Between Parkinsons And Lewy Body Dementia
Being Patient: Are Parkinsons disease and Lewy body dementia related?
Dag Aarsland: Yes, theyre related in terms of symptoms and the brain changes. Many scientists consider Parkinsons and Lewy body dementia as a continuum of disease rather than two separate diseases. But there are very active and lively discussions about that. There are arguments for separating and combining them, but there are many similarities.
Being Patient: Do you group Lewy body dementia with Parkinsons disease in your research?
Dag Aarsland: From a research point-of-view, we try to separate them. We identify the specifics and categorize patients in different groups and study them carefully in order to see how they relate. In clinical practice, its different. I also see patients with Parkinsons and unfortunately, many of them develop dementia and hallucinations or memory problems. In clinical practice, its very much the same challenges for patients, carers and the doctor in terms of findings and the right therapy.
What Causes Parkinson Disease
Parkinson disease arises from decreased dopamine production in the brain. The absence of dopamine makes it hard for the brain to coordinate muscle movements. Low dopamine also contributes to mood and cognitive problems later in the course of the disease. Experts dont know what triggers the development of Parkinson disease most of the time. Early onset Parkinson disease is often inherited and is the result of certain gene defects.
There are many rarer diseases and conditions that can lead to dementia, or dementia-like symptoms.
These conditions account for only 5% of dementia cases in the UK.
They include:
- problems with planning and reasoning
These symptoms are not severe enough to cause problems in everyday life.
MCI can be caused by an underlying illness, such as depression, anxiety or thyroid problems.
If the underlying illness is treated or managed, symptoms of MCI often disappear and cause no further problems.
But in some cases, people with MCI are at increased risk of going on to develop dementia, which is usually caused by Alzheimers disease.
These measures can help you live well with Parkinson disease:
You May Like: What Color Ribbon Is Alzheimers
Don’t Miss: Are There Service Dogs For Parkinson’s Patients
Parkinson’s Disease And Lewy Body Dementia Explained
- Learn more about Parkinson’s disease and Lewy body dementia. These degenerative brain disorders are caused by abnormal clumps of protein called Lewy bodies.
Parkinson’s disease and Lewy body dementia are degenerative brain disorders. Both diseases are linked to protein deposits in the nerve cells of the brain known as Lewy bodies.
The two disorders have similar symptoms. People with LBD may experience tremors and muscle stiffness like those who have Parkinson’s. And, while Parkinson’s disease affects motor function, about 40% of people with Parkinson’s also develop dementia as the disease advances.
Here’s a closer look at the connection between Parkinson’s disease and Lewy body dementia.
Epidemiology And Natural History Of Dlb And Pdd
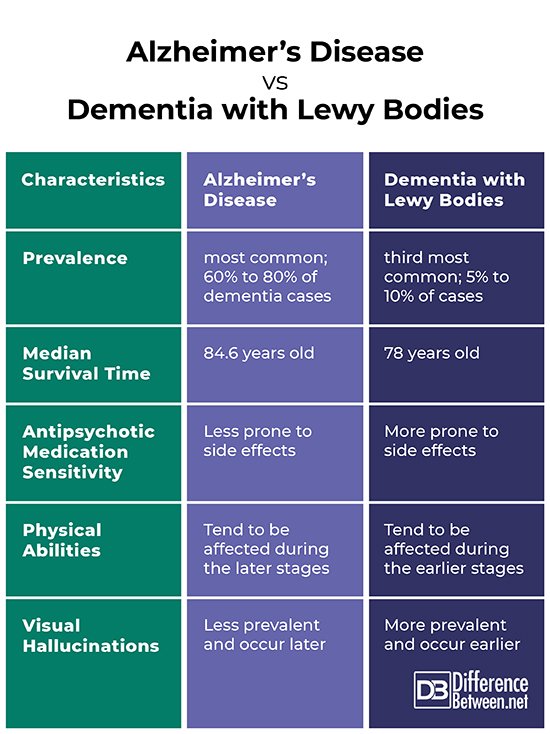
Approximately 12% of those aged above 65 years are diagnosed with DLB worldwide , affecting approximately 5% of all dementia cases in those over the age of 75 . Its incidence is 0.71.4 new cases/100,000 person-years or 3.5/100,000 person-years . For PDD, the cumulative prevalence is of 75% of PD patients surviving more than 10 years , 83% after 20 years , and up to 95% by age 90 years , with an overall prevalence of 31.1% and incidence rates from 0.43 to 1.13/100,000 person-years , indicating that, annually, approximately 10% of a PD population will develop dementia . The data concerning age at disease or dementia onset are highly variable. Whereas in the Olmsted County study DLB patients were younger at symptom onset than those with PDD and had more hallucinations and cognitive fluctuations, others have reported younger age at disease onset in PDD , or no essential differences between disorders .
Read Also: Pump For Parkinson’s Disease
Differences Between Pdd And Dlb
So, how are PDD and DLB different from each other? That depends on whom you ask. Some clinicians feel that these two conditions are simply different versions of the same disorder. In fact, some professionals use the terms interchangeably. Yet, according to currently agreed-upon diagnostic guidelines, there are some differences.
Dementia With Lewy Bodies And Parkinson Disease Dementia
, MD, PhD, Department of Neurology, University of Mississippi Medical Center
Dementia with Lewy bodiesParkinson disease dementia
Dementia is chronic, global, usually irreversible deterioration of cognition.
Dementia with Lewy bodies is the 3rd most common dementia. Age of onset is typically > 60.
Lewy bodies are spherical, eosinophilic, neuronal cytoplasmic inclusions composed of aggregates of alpha-synuclein, a synaptic protein. They occur in the cortex of some patients who have dementia with Lewy bodies. Neurotransmitter levels and neuronal pathways between the striatum and the neocortex are abnormal.
Lewy bodies also occur in the substantia nigra of patients with Parkinson disease, and dementia may develop late in the disease. About 40% of patients with Parkinson disease develop Parkinson disease dementia, usually after age 70 and about 10 to 15 years after Parkinson disease has been diagnosed.
Because Lewy bodies occur in dementia with Lewy bodies and in Parkinson disease dementia, some experts think that the two disorders may be part of a more generalized synucleinopathy affecting the central and peripheral nervous systems. Lewy bodies sometimes occur in patients with Alzheimer disease, and patients with dementia with Lewy bodies may have neuritic plaques and neurofibrillary tangles. Dementia with Lewy bodies, Parkinson disease, and Alzheimer disease overlap considerably. Further research is needed to clarify the relationships among them.
Don’t Miss: 5 Signs You Ll Get Parkinson’s
The Four Atypical Parkinsonism Disorders
This section compares the four atypical parkinsonism disorders:
These diseases are frequently mistaken for each other and for Parkinsons Disease, Alzheimers Disease, stroke, and other neurological conditions. To some extent, we address the questions If its not Alzheimers Disease, what is it? and If its not Parkinsons Disease, what is it?
Excellent organizations focus on each of these atypical parkinsonism disorders. We list these organizations on our pages dedicated to each disorder. Brain Support Network casts a wider net, describing and comparing the four disorders and their subtypes.
Given our extensive experience with brain donation, we know that the diagnostic accuracy of these disorders is low. We know the diagnosis before the brain is delivered for autopsy and we learn the definitive diagnosis by the neuropathologist after autopsy. Accuracy hovers around 50%, even for diagnoses delivered by expert neurologists.
These disorders are rare, difficult to diagnose, and moving targets as new subtypes are described. One of BSNs missions is to sketch the landscape so that laypeople can have meaningful discussions with medical providers and can serve as effective advocates.