Characteristics Of Restless Leg Syndrome
There are certain features of RLS that make it a unique and specific disorder.
Treatment Of Rls In Pd
Regardless of the above discussion, it is clear that many people with PD have difficulty falling asleep because of annoying sensations in the legs accompanied by a sometimes unbearable sense of restlessness in the legs. For these people, taking dopamine agonists before bed can be helpful. Caution is in order, of course, because in some patients with PD, especially older or more advanced patients, these medications can cause confusion and hallucinations and are thus not well-tolerated. A long-acting levodopa formulation or medications such as gabapentin, gabapentin enacarbil and pregabalin can also be effective. Trying to address sleep issues such as RLS in patients who have sleep complaints can be an important aspect of maximizing therapy for PD.
Tips and Takeaways
Do you have a question or issue that you would like Dr. Gilbert to explore? Suggest a Topic
Dr. Rebecca Gilbert
APDA Vice President and Chief Scientific Officer
In Vivo Corneal Confocal Microscopy
All participants underwent IVCCM bilaterally, or unilaterally if one eye met exclusion criteria. The central corneal subbasal nerve plexus was imaged as previously described. Briefly, a topically anesthetized eye was examined with the Heidelberg Retinal Tomograph 3 laser-scanning confocal microscope with the Rostock Corneal Module . A single examiner performed all eye scanning, recording images of the subbasal nerve plexus across a wide area of the plexus using the built-in fixation light to access paracentral regions and continually adjusting the focus to the plexus depth. Mosaics were generated with an automated computer algorithm to select nerve plexus images from the recorded data using tissue classification and to stitch together adjacent images. Depth variations of subbasal nerve fiber paths were mapped onto a single two-dimensional mosaic image. A separate automated algorithm was used for detection and tracing of nerve paths and branching points, from which the mean values of CNFL and CNBD were calculated,. Averaged values between both eyes were used where applicable.
Recommended Reading: Diseases Similar To Parkinsons
Home Care Tips For Restless Legs Syndrome
The following approaches can reduce symptoms in patients with mild or moderate RLS and may be used in combination with medication in RLS patients who have severe symptoms.
- Sleep hygiene: Good sleep hygiene means maintaining a bedroom environment and a daily routine that supports high-quality sleep. Avoiding alcohol and caffeine is especially important for RLS patients because these substances can worsen symptoms.
- Exercise: Because physical inactivity often triggers RLS symptoms, exercise may be helpful. A research study found that RLS patients showed af 39% reduction in symptom severity after six weeks of engaging in an exercise program compared to an 8% symptom reduction in patients who did not exercise.
- Pneumatic pressure therapy: Pneumatic compression devices increase blood flow to the legs by filling with air to squeeze the legs. Researchers found that the device improved RLS symptoms, quality-of-life, and fatigue after one month of daily use compared to a control group.
- Massage and hot baths: Using massage and hot baths to stimulate the legs is widely recommended in RLS literature however, there is limited scientific evidence supporting the effectiveness of these methods at this time.
Learn more about treating RLS here.
- Was this article helpful?
Pathological Evidence Of Dopamine Dysfunction In Pd And Rls
Post-mortem studies in PD demonstrate loss of nigral neurons resulting in striatal dopamine deficiency, with differing morphological lesion patterns according to the clinical subtypes of PD. Cell loss in the ventrolateral part of the substantia nigra pars compacta projecting to the dorsal putamen is more prominent in the akinetic-rigid type, whereas tremor-dominant PD shows predominantly medial SNPC cell loss . Variability in lesion patterning might explain why some patients with PD may develop RLS. In addition, loss of dopamine 2 receptors has been documented in advanced PD .
At autopsy of 8 patients with primary RLS, there was a significant decrease in dopamine 2 receptors in the putamen compared to a neurologically normal control group. The decrease in the D2 receptors correlated to the severity of the RLS . This evidence that the nigrostriatal dopaminergic system is affected in both RLS and PD might provide a stronger argument for an etiologic link between the two. Moreover, there were significant increases in tyrosine hydroxylase in the substantia nigra, but not in the putamen of the RLS group. Phosphorylated tyrosine hydroxylase was found to be increased in both the substantia nigra and putamen. These findings are consistent with data from animal iron deficiency models demonstrating increased presynaptic dopaminergic activity .
Don’t Miss: Adaptive Silverware For Parkinson’s
Who Gets Restless Legs Syndrome
About 10% of people have restless legs syndrome, also called RLS. About 2% to 3% of them have moderate to severe symptoms that affect their quality of life. Also:
- Slightly more women than men get it.
- Most people with severe RLS are middle-aged or older.
- Only 2% of children get RLS.
- People with RLS in their family usually get it at a younger age.
Pd And Rls: An Overview
PD is a progressive neurodegenerative disorder characterised by pathologic intraneuronal alpha-synuclein-positive Lewy bodies and neuronal cell loss. In particular, involvement of dopaminergic cells in the substantia nigra pars compacta is associated with development of the motor features of the disease. The cardinal clinical symptoms and signs of PD are bradykinesia, rigidity, tremor, postural instability and freezing attacks . The prevalence of PD increases with age, affecting 1-2% of the population over the age of 65 years, and 3% of those over 85 years . Several monogenic forms of PD and numerous genetic susceptibility factors have been identified . Sleep disturbances have been widely reported in PD, although an increased incidence of periodic leg movements of sleep is debatable, with polysomnography studies revealing mixed findings .
RLS can be associated with medical conditions such as renal failure, iron deficiency, neuropathy, and pregnancy . Family history, with an autosomal dominant mode of inheritance may be present in more than half of the cases. Five genetic loci for RLS have been reported in different pedigrees, of which 4 are autosomal dominant and one autosomal recessive . The detection of PLMS during overnight polysomnography is the the most frequent objective abnormality and can be demonstrated in the majority of RLS patients . However, the absence of PLMS does not exclude RLS .
Recommended Reading: Zhichan Capsule
What Is The Connection Between Iron And Restless Legs Syndrome
Not enough iron in the diet is one cause of restless legs syndrome. Taking iron pills may improve RLS in these people.
Even in people who are not anemic and have normal iron levels, iron levels may be involved. Studies show a “brain iron deficiency” in many people with restless legs syndrome. A doctor may prescribe iron supplements even if a person’s iron levels are within normal range. However, too much iron can lead to liver damage and other health problems.
What Treatment Is Available
RLS is a condition that is treatable and generally susceptible to pharmacologic therapy. A wide range of different treatment options is available, including drugs that modulate certain calcium-channels, dopaminergic agents, opioids, and benzodiazepines. However, the medical condition most commonly associated with RLS is iron deficiency so your doctor should first check your ferritin levels . If levels are low you will be given an iron supplement. For some people increasing the ferritin levels will eliminate or reduce the RLS symptoms.
Some Parkinson’s medications can make RLS worse and should be avoided. For example, some people who take levodopa complain that RLS symptoms occur during the day, as well as evenings, and may also involve the arms and the face. These symptoms typically worsen late in the night as the medication wears off. It is therefore often preferable to use dopamine agonists such as pramipexole or ropinirole tablets, or rotigotine skin patches instead of levodopa when treating Parkinsons and RLS.
If you are already taking dopamine agonists to manage Parkinson’s symptoms and you still experience RLS symptoms, then your doctor may suggest you try other medications, such as gabapentin, pregabalin, opioids or clonazepam, although these may or may not be licenced to treat RLS in your country.
Read Also: Does Sam Waterston Have Parkinsons
People With Parkinsons Disease More Likely To Have Leg Restlessness Than Restless Leg Syndrome
The American Academy of Neurology, an association of more than 24,000 neurologists and neuroscience professionals, is dedicated to promoting the highest quality patient-centered neurologic care. A neurologist is a doctor with specialized training in diagnosing, treating and managing disorders of the brain and nervous system such as Alzheimers disease, stroke, migraine, multiple sclerosis, brain injury, Parkinsons disease and epilepsy.For more information about the American Academy of Neurology, visit .
Fatigue Sleep Difficulties And Restless Legs
Although Parkinsons is classified as a movement disorder, it can affect people in various different ways. Sometimes the non-movement symptoms can be more troublesome and can have a bigger impact on the daily life of someone living with Parkinsons.
Some of the more common non-movement symptoms of Parkinsons are:
- Fatigue
- Restless legs
Don’t Miss: Parkinson’s Bike Therapy
What Causes Restless Legs Syndrome
The cause of restless legs syndrome is usually unknown. Experts think that RLS may be connected to how the brain uses dopamine and iron.
Genetics also plays a role. About half of people with restless legs syndrome have a family member with it.
Many medical conditions are linked to RLS, including iron deficiency, diabetes, end-stage kidney disease, Parkinson’s disease, and pregnancy. But most people with restless legs syndrome do not have one of these conditions. If you have one of these conditions, treating it can improve RLS symptoms.
Future Prospects: Questions To Be Answered
The link between PD and RLS has yet to be clearly determined with clinical association studies differing widely in their findings, with some finding the incidence of RLS to be much greater in PD patients, and others finding no difference from that in the general population. These discrepancies could be addressed with prospective long-term clinical studies of PD patients who develop RLS and vice versa, with documentation of exposure to dopaminergic therapies.
With the exception of the parkin mutation, genetic studies have been failed to reveal any associations. We propose that population based genetic association studies of PD plus RLS and linkage studies of PD plus RLS as well as comparative studies of PD vs. PD-RLS vs. RLS should be conducted.
Sonographic studies reveal notable differences between PD and PD-RLS patients. Functional MRI studies have yet to focus on those patients with PD-RLS. Prospective functional imaging studies of PD vs. PD-RLS are needed to better understand the mechanisms involved in these disorders. To our knowledge, there have been no pathological studies looking at patients with PD-RLS. Establishing the pattern of decreased D2 receptor density in PD vs. PD and RLS vs. RLS may be valuable in understanding common pathophysiology. The reports purporting to DBS and RLS are conflicting, and more studies need to be done to clarify the effect, with attention to adjustments in dopaminergic medications.
Don’t Miss: Parkinson Silverware
Restless Legs Syndrome And Periodic Limb Movement Disorder
Most people who have RLS also have a condition called periodic limb movement disorder . PLMD involves repetitive flexing or twitching of the limbs while asleep at night. It is different from RLS in that these movements are not accompanied by uncomfortable sensations and because they occur during sleep, patients are often not aware of them. However, PLMD-associated movements can cause a person to wake up and therefore can compound sleep issues in patients who also have RLS.
Although most people with RLS have PLMD, many with PLMD do not have RLS.
How Can I Get A Good Night’s Sleep Despite Restless Legs Syndrome
Experts agree that simply changing your behavior can often help you sleep if you have restless legs syndrome. For people with mild to moderate RLS, these steps can reduce or prevent symptoms:
- Cut down on caffeine.
- Stop smoking, or at least cut back.
- Go to bed and get up at the same time each day, including weekends.
- Exercise regularly, but moderately .
- Apply heat or ice, or soak in a hot bath.
Read Also: Voice Amplifiers For Parkinson’s
How Is Restless Legs Syndrome Diagnosed
There are no objective tests for the diagnosis of RLS, which is based entirely on the description of symptoms.
A diagnosis of RLS is made if a person displays all five primary clinical features set out in 1995 and amended in 2014 by the International Restless Legs Syndrome Study Group:
In addition, other features that may suggest a diagnosis of RLS are:
- periodic limb movements when asleep
- improvement of symptoms on dopaminergic treatment
- a family history of RLS.
If RLS is diagnosed, your doctor should also check that you are not taking drugs which make RLS worse . You may also be referred for a neurological examination to see whether damage of the nerves in the legs is causing the urge to move and uncomfortable sensations.
Association Between Restless Legs Syndrome And Other Movement Disorders
Several reports describe a possible association between restless legs syndrome and Parkinson disease , as well as Tourette syndrome and RLS, according to a literature review published in Neurology.
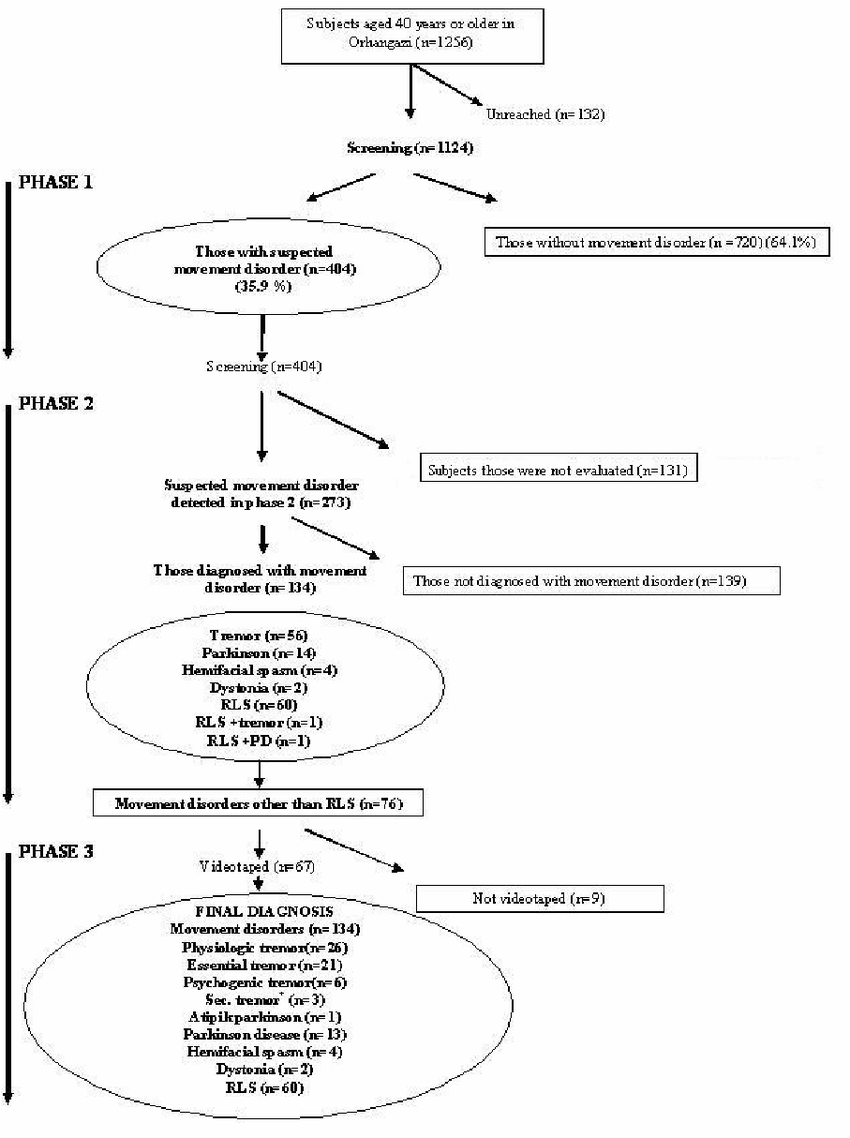
RLS is a common sensorimotor disorder, and epidemiologic studies have demonstrated an association between it and other movement disorders such as PD, essential tremor, choreic and dystonic syndromes, TS, and heredodegenerative ataxias. However, the underlying pathophysiologic associations are unclear, and therefore researchers conducted a meta-analysis of eligible studies that focus on the possible association between RLS and other movement disorders, and discussed the possible common pathophysiologic mechanisms.
Read Also: On And Off Phenomenon
Does Having Rls Increase The Risk Of Developing Pd
Since RLS affects as much as 4-10% of the US adult population, it is clear that the vast majority of those with RLS do not ever develop PD.
Despite this, it still might be the case that RLS increases the risk of subsequently developing PD. There have been many studies trying to figure this out with conflicting results. Some studies show that there is no increased risk and others show that having RLS confers about a two-fold increased risk of developing PD over the general population.
Want To Learn More About The Latest Research In Parkinsons Disease Ask Your Questions In Our Research Forum
Having RLS in 2002 and/or 2008 was associated with a higher risk of constipation in 2012, compared with controls. Only individuals who had RLS in both 2002 and 2008 showed higher odds of having possible RBD alone, and both constipation and possible RBD in 2012, indicating a potential association between continuous/recurrent RLS and , according to the researchers.
They cautioned that constipation is a relatively non-specific Parkinsons symptom and may not indicate a direct link between RLS and Parkinsons.
No differences were found between olfactory scores of men with or without RLS. However, the team noted that olfactory scores were only available from a subset of participants. Additionally, the timing of the smell sense analysis may also have influenced this result, since a loss of sense of smell has been reported as a relatively late symptom in the early stages of Parkinsons compared with RBD and constipation, they said.
We assessed the association between RLS and prodromal signs, but not between RLS and incidence. However, our focus was on identifying whether RLS is an early indicator of the underlying common disease process in , the authors wrote.
The findings warrant future studies for RLS and Parkinsons incidence in the long-term, they said.
Among the studys limitations, the authors mentioned that the link between Parkinsons and RLS may differ by gender, since women, although they have a reduced risk for Parkinsons, are more susceptible to RLS.
You May Like: Parkinson’s Double Vision
What Is Restless Leg Syndrome
Restless Leg Syndrome is a sleep and movement disorder. Those with this condition will have an urge to move their legs and abnormal feelings of tingling or prickling . The urge to move will feel worse at rest, and only be relieved by movement such as stretching or walking. All of these symptoms will only occur or worsen at night. Some people with RLS will move their legs during their sleep as well. This is known as Periodic Limb Movement during Sleep , and may cause so much movement they will wake themselves up.