Is Parkinsons Disease Inherited
Scientists have discovered gene mutations that are associated with Parkinsons disease.
There is some belief that some cases of early-onset Parkinsons disease disease starting before age 50 may be inherited. Scientists identified a gene mutation in people with Parkinsons disease whose brains contain Lewy bodies, which are clumps of the protein alpha-synuclein. Scientists are trying to understand the function of this protein and its relationship to genetic mutations that are sometimes seen in Parkinsons disease and in people with a type of dementia called Lewy body dementia.
Several other gene mutations have been found to play a role in Parkinsons disease. Mutations in these genes cause abnormal cell functioning, which affects the nerve cells ability to release dopamine and causes nerve cell death. Researchers are still trying to discover what causes these genes to mutate in order to understand how gene mutations influence the development of Parkinsons disease.
Scientists think that about 10% to 15% of persons with Parkinsons disease may have a genetic mutation that predisposes them to development of the disease. There are also environmental factors involved that are not fully understood.
Lrrk2 Plasticity And Behavior
Collectively the data support that LRRK2 mutation alters vesicle recycling, trafficking and possibly protein synthesis during development in ways that are sustained, impacting certain cellular behaviors over the lifespan, and in other ways that are transient, but have permanent consequences for the assembly of neural circuits and the eventual behaviors they support. Given the impact of the G2019S mutation on LTP in the dorsal striatum, it is likely that striatal behaviors like action-outcome learning or other forms of goal-directed behaviors will be affected similarly to what has been observed in reward-based circuits modified by social stress paradigms.
How Is Parkinsons Disease Diagnosed
Diagnosing Parkinsons disease is sometimes difficult, since early symptoms can mimic other disorders and there are no specific blood or other laboratory tests to diagnose the disease. Imaging tests, such as CT or MRI scans, may be used to rule out other disorders that cause similar symptoms.
To diagnose Parkinsons disease, you will be asked about your medical history and family history of neurologic disorders as well as your current symptoms, medications and possible exposure to toxins. Your doctor will look for signs of tremor and muscle rigidity, watch you walk, check your posture and coordination and look for slowness of movement.
If you think you may have Parkinsons disease, you should probably see a neurologist, preferably a movement disorders-trained neurologist. The treatment decisions made early in the illness can affect the long-term success of the treatment.
Recommended Reading: Voice Amplifiers For Parkinson’s
How Is Parkinsons Disease Treated
There is no cure for Parkinsons disease. However, medications and other treatments can help relieve some of your symptoms. Exercise can help your Parkinsons symptoms significantly. In addition, physical therapy, occupational therapy and speech-language therapy can help with walking and balance problems, eating and swallowing challenges and speech problems. Surgery is an option for some patients.
James Parkinson And Parkinsons Disease
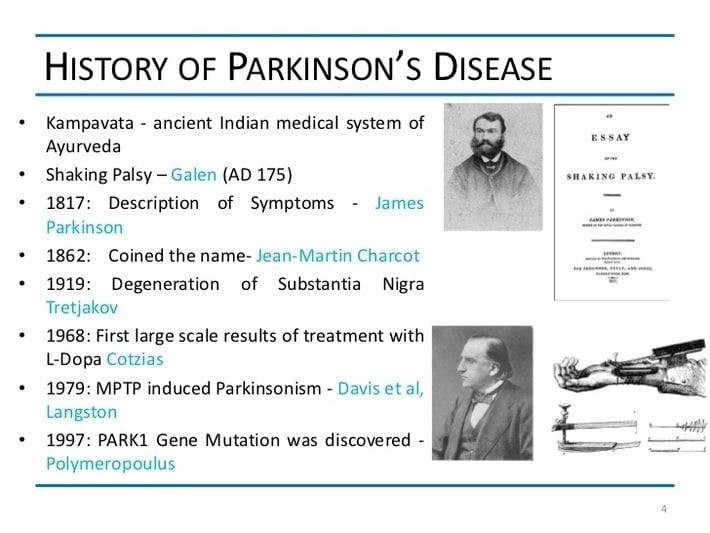
Parkinson’s disease was formally recognized in James Parkinson’s 1817 classic paper, “An Essay on the Shaking Palsy.”
Parkinson was a doctor in London who observed what are now known as the classic symptoms of Parkinson’s disease in three of his patients, and in three people he saw on the streets of the city. His essay contained clear descriptions of some of the main symptoms: tremors, rigidity, and postural instability. He theorized that the disease developed because of a problem in the brain’s medulla region.
Although Parkinson encouraged the medical community to study the disease and had hoped for a cure, his essay received little attention until 1861. It was then that French neurologist Jean-Martin Charcot and his colleagues distinguished the disease from other neurological conditions and termed it “Parkinson’s disease.”
Also Check: Cleveland Clinic Parkinson’s Bicycle Study 2017
Th Century And Beyond
The first speculations concerning the anatomical substrate of PD were made 80 years after Parkinson’s essay, when Ãdouard Brissaud proposed that it had its origin in the subthalamus or cerebral peduncle and might be caused by an ischemic lesion. In 1912 Frederic Lewy described a pathologic finding in affected brains, later named “Lewy bodies“. In 1919 Konstantin Tretiakoff reported that the substantia nigra was the main cerebral structure affected, but this finding was not widely accepted until it was confirmed by further studies published by Rolf Hassler in 1938. The underlying biochemical changes in the brain were identified in the 1950s, due largely to the work of Arvid Carlsson on the neurotransmitter dopamine and Oleh Hornykiewicz on its role on PD. Carlsson was eventually awarded a Nobel Prize for this work.
Thanks For Signing Up
We are proud to have you as a part of our community. To ensure you receive the latest Parkinsons news, research updates and more, please check your email for a message from us. If you do not see our email, it may be in your spam folder. Just mark as not spam and you should receive our emails as expected.
You May Like: Weighted Silverware
What Would Parkinson The Social Reformer Think
Parkinson was a social reformer writing under the nom de plume Old Herbit he campaigned for the rights of lunatics, children, and older people. Age is the strongest risk factor for PD. Worldwide prevalence of PD per 100,000 is 41 at 4049 years compared to 428 at 6069 years and 1,903 in those older than 80 years . 200 Years ago, when Parkinson wrote the Shaking Palsy, average life expectancy at birth in the UK was less than 45 years. For a women born in the UK 2010, this is now 82 years. In recent years life expectancy has also begun to increase in the developing world resulting in an increased burden of chronic disease. Traditionally healthcare systems in the developing world have been focused on managing communicable disease in younger populations. As their populations age the need to manage chronic disease in an ageing population will present an increasing challenge. Dorsey et al. have projected that the number of individuals living with PD will more than double between 2005 and 2030, and that the population of PD patients is set to become increasingly concentrated in the developing world .
What Lifestyle Changes Can I Make To Ease Parkinsons Symptoms
Exercise: Exercise helps improve muscle strength, balance, coordination, flexibility, and tremor. It is also strongly believed to improve memory, thinking and reduce the risk of falls and decrease anxiety and depression. One study in persons with Parkinsons disease showed that 2.5 hours of exercise per week resulted in improved ability to move and a slower decline in quality of life compared to those who didnt exercise or didnt start until later in the course of their disease. Some exercises to consider include strengthening or resistance training, stretching exercises or aerobics . All types of exercise are helpful.
Eat a healthy, balanced diet: This is not only good for your general health but can ease some of the non-movement related symptoms of Parkinsons, such as constipation. Eating foods high in fiber in particular can relieve constipation. The Mediterranean diet is one example of a healthy diet.
Preventing falls and maintaining balance: Falls are a frequent complication of Parkinson’s. While you can do many things to reduce your risk of falling, the two most important are: 1) to work with your doctor to ensure that your treatments whether medicines or deep brain stimulation are optimal and 2) to consult with a physical therapist who can assess your walking and balance. The physical therapist is the expert when it comes to recommending assistive devices or exercise to improve safety and preventing falls.
Don’t Miss: Zhichan Capsule
Pattern Of Symptoms In Parkinsons Disease
While the motor symptoms are the current standard for diagnosing PD, research has shown that PD non-motor symptoms, particularly gastrointestinal symptoms and the reduced sense of smell, may begin years before the motor symptoms appear. When the motor symptoms show up in the body, they generally begin on one side of the body. This is called unilateral presentation. As the disease progresses, the symptoms may spread to the other side of the body as well.3,6
PD is a progressive disease, and the symptoms worsen over time. This progression of symptoms is also noteworthy when considering a diagnosis of PD.3
What Causes Parkinsons Disease
Parkinsons disease occurs when nerve cells in an area of the brain called the substantia nigra become impaired or die. These cells normally produce dopamine, a chemical that helps the cells of the brain communicate . When these nerve cells become impaired or die, they produce less dopamine. Dopamine is especially important for the operation of another area of the brain called the basal ganglia. This area of the brain is responsible for organizing the brains commands for body movement. The loss of dopamine causes the movement symptoms seen in people with Parkinsons disease.
People with Parkinsons disease also lose another neurotransmitter called norepinephrine. This chemical is needed for proper functioning of the sympathetic nervous system. This system controls some of the bodys autonomic functions such as digestion, heart rate, blood pressure and breathing. Loss of norepinephrine causes some of the non-movement-related symptoms of Parkinsons disease.
Scientists arent sure what causes the neurons that produce these neurotransmitter chemicals to die.
Recommended Reading: Parkinson Bicycle Cleveland Clinic
The Future: Parkinson’s Clinical Trials
Researchers are continuously working on ways to slow the progression of Parkinson’s disease, restore lost functioning, and help prevent the disease from developing in the first place. You can find out if you or a loved one is right for one of hundreds of clinical trials for Parkinson’s Disease at the Fox Trial Finder.
Progression Of Motor Symptoms On Levodopa
In addition to previous considerations on the yearly decline in UPDRS-III OFF scores , we also report that, compared to 1-year follow-up, OFF state UPDRS-II and -III scores also worsened at 2 years , despite the increase in daily levodopa dosage, while the UPDRS-III in the ON state remained unchanged . The prevalence of subjects who developed motor fluctuations significantly increased. Nonetheless, OFF state motor performance and the ADL after 2 years were still significantly better than at baseline . At 4-year follow-up, UPDRS-III scores in the overnight OFF and in the ON state remained significantly lower than at baseline , despite the UPDRS-III worsening between the 1- and 4-year follow-up visits . At this time point, the UPDRS-II score, the non-dopaminergic score and the Hoehn and Yahr stage were similar to baseline .
Also Check: Diseases Similar To Parkinsons
Physical Exam For Parkinson’s
During a physical exam, the doctor examines the patients body for signs of disease. The doctor will include a visual inspection , palpation , ascultation , and percussion . The physical exam for PD is generally conducted by a neurologist and may also be called a neurological exam. It is recommended that a patient see a neurologist with special training in movement disorders as these specialists have the most knowledge about the symptoms and medications. During a neurological exam, the patient may be asked to sit, stand, walk, and extend their arms as the doctor evaluates balance and coordination. Most neurologists recommend a spouse or caregiver attend the exam with the patient to help with answering important questions.1,2
The Evolution Of Treatments
The history of Parkinson’s disease is tightly linked to therapeutic interventions, ranging from serendipitous observations to controlled clinical trials of specifically designed agents.
Parkinson devoted a chapter of his monograph to considerations respecting the means of cure . In humility and perhaps with a vision toward current concepts of neuroprotection, he hoped for the identification of a treatment by which the progress of the disease may be stopped . To this end, he advocated very early therapeutic intervention when signs were largely confined to the arms without balance and gait impairments. Reflecting therapeutic approaches of the early nineteenth century, Parkinson recommended venesection, specifically advocating bloodletting from the neck, followed by vesicatories to induce blistering and inflammation of the skin. Small pieces of cork were purposefully inserted into the blisters to cause a sufficient quantity of purulent discharge . All these efforts were designed to divert blood and inflammatory pressure away from the brain and spinal cord, and in this way, decompress the medulla that Parkinson considered the seat of neurological dysfunction.
Don’t Miss: Parkinson’s Double Vision
Providing Holistic Care In Pd
James Parkinson was a strong believer in the role of medicine to go beyond treating the disease and recognised the importance of holistic care. Given the constellation of symptoms seen in PD the condition has previously been referred to as a geriatric syndrome . It therefore follows that management of the condition may well be suited to an approach analogous to the Comprehensive Geriatric Assessment employed by geriatricians . The skill-set of a geriatrician, along with the wider multidisciplinary team, may be particularly valuable as PD reaches the complex phase, where the burden of neuropsychiatric and non-motor complications is high. Furthermore, geriatricians have expertise in end of life care. As PD progresses towards the palliative phase, geriatricians often have a central role in ensuring patients autonomy is preserved and that potentially difficult conversations about advanced care planning are undertaken at the appropriate stage in the condition.
Parkinson recognised the importance of carers in his original description of the disease and made reference to the need for support with activities of daily living.
The patient walks now with great difficulty, and unable any longer to support himself with his stick, he dares not venture on this exercise, unless assisted by an attendant, who walking backwards before him, prevents his falling forwards, by the pressure of his hands against the fore part of his shoulders.
How Do I Prevent Falls From Common Hazards
- Floors: Remove all loose wires, cords, and throw rugs. Minimize clutter. Make sure rugs are anchored and smooth. Keep furniture in its usual place.
- Bathroom: Install grab bars and non-skid tape in the tub or shower. Use non-skid bath mats on the floor or install wall-to-wall carpeting.
- Lighting: Make sure halls, stairways, and entrances are well-lit. Install a night light in your bathroom or hallway and staircase. Turn lights on if you get up in the middle of the night. Make sure lamps or light switches are within reach of the bed if you have to get up during the night.
- Kitchen: Install non-skid rubber mats near the sink and stove. Clean spills immediately.
- Stairs: Make sure treads, rails, and rugs are secure. Install a rail on both sides of the stairs. If stairs are a threat, it might be helpful to arrange most of your activities on the lower level to reduce the number of times you must climb the stairs.
- Entrances and doorways: Install metal handles on the walls adjacent to the doorknobs of all doors to make it more secure as you travel through the doorway.
You May Like: Parkinson’s Hallucinations Commercial
The History Of Parkinson’s Disease Treatment
For many decades, doctors couldn’t treat Parkinson’s disease effectively, and thought it was a terminal illness. The drugs used to treat the symptoms of tremor in the late 1800s included arsenic, morphine, hemlock, and cannabis, according to Chrisopher Goetz’s review published in September 2011 in Cold Spring Harbor Perspectives in Medicine.
Sidebar: Advances In Circuitry Research
The brain contains numerous connections among neurons known as neural circuits.
Research on such connections and networks within the brain have advanced rapidly in the past few years. A wide spectrum of tools and techniques can now map connections between neural circuits. Using animal models, scientists have shown how circuits in the brain can be turned on and off. For example, researchers can see correlations between the firing patterns of neurons in a zebrafishs brain and precise behavioral responses such as seeking and capturing food.
Potential opportunities to influence the brains circuitry are starting to emerge. Optogenetics is an experimental technique that involves the delivery of light-sensitive proteins to specific populations of brain cells. Once in place, these light-sensitive proteins can be inhibited or stimulated by exposure to light delivered via fiber optics. Optogenetics has never been used in people, however the success of the approach in animal models demonstrates a proof of principal: A neural network can be precisely targeted.
Thanks in part to the BRAIN Initiative, research on neural circuitry is gaining momentum. The Brain Research through Advancing Innovative Neurotechnologies Initiative is accelerating the development and application of new technologies that enable researchers to produce dynamic pictures of the brain that show how individual brain cells and complex neural circuits interact at the speed of thought.
NIH Publication No. 15-5595
Read Also: Yopd Life Expectancy
What Is The Outlook For Persons With Parkinsons Disease
Although there is no cure or absolute evidence of ways to prevent Parkinsons disease, scientists are working hard to learn more about the disease and find innovative ways to better manage it, prevent it from progressing and ultimately curing it.
Currently, you and your healthcare teams efforts are focused on medical management of your symptoms along with general health and lifestyle improvement recommendations . By identifying individual symptoms and adjusting the course of action based on changes in symptoms, most people with Parkinsons disease can live fulfilling lives.
The future is hopeful. Some of the research underway includes:
- Using stem cells to produce new neurons, which would produce dopamine.
- Producing a dopamine-producing enzyme that is delivered to a gene in the brain that controls movement.
- Using a naturally occurring human protein glial cell-line derived neurotrophic factor, GDNF to protect dopamine-releasing nerve cells.
Many other investigations are underway too. Much has been learned, much progress has been made and additional discoveries are likely to come.
Living Well With Parkinson’s

While medication and DBS surgery are the most effective treatments for PD, individuals often choose to delay these treatments because of their adverse side effects. Until a therapy is developed that can halt the progression of PD, there is a significant need for strategies that provide symptom relief without causing negative side effects.
Diet, Exercise, and Stress Reduction
Findings from several studies suggest that exercise has the potential to provide relief from certain PD symptoms. Anecdotally, people with Parkinsons disease who exercise typically do better. However, many questions remain. Among them is whether exercise provides a conditioning effect by strengthening muscles and improving flexibility or whether it has a direct effect on the brain.
In an NINDS-funded trial comparing the benefits of tai chi, resistance training, and stretching, tai chi was found to reduce balance impairments in people with mild-to-moderate PD. People in the tai chi group also experienced significantly fewer falls and greater improvements in their functional capacity.
Technologies that Improve Quality of Life
Also Check: On And Off Phenomenon