Getting Medication On Time
Parkinson’s patients who do not get the correct medicine at the right time when they are in hospital, sometimes cannot talk or walk. The health of a majority deteriorated due to unsatisfactory medication management when they are in hospital. Parkinson’s UK believes the NHS could save up to £10m a year and improve the care of Parkinson’s patients if mandatory training is introduced for all hospital staff.
Parkinson UK found:
- “Nearly two thirds of people who have Parkinsons dont always get their medication on time in hospital.”
- “More than three quarters of people with Parkinsons that we asked reported that their health deteriorated as a result of poor medication management in hospital.”
- “Only 21% of respondents told us they got their medication on time without having to remind hospital staff.”
Parkinsons Disease: Management And Guidance
An overview of Parkinsons disease management, including discussion of the updated National Institute for Health and Care Excellence guidelines.
Nervous system diseases
DR. MICHAEL SOUSSAN/ISM/SCIENCE PHOTO LIBRARY
Parkinsons disease is a chronic, progressive neurodegenerative condition resulting from the loss of the dopamine-containing cells of the substantia nigra, and its prevalence increases with age. Using primary care data from 2015, a Parkinsons UK report of the Clinical Practice Research Datalink found that the prevalence of PD is 45 per 100,000 people who are aged 3039 years, compared with 1,696 per 100,000 people who are aged 8084 years. Prevalence rates almost double at each five-year interval between the ages of 50 and 69 years for both men and women. The lifetime risk of being diagnosed with PD is 2.7% equating to 1 in every 37 people being diagnosed at some point in their lifetime. Owing to population growth and an increasing ageing population, the estimated prevalence of PD is expected to increase by 23.2% by 2025.
Caring For Patients With Parkinsons Disease In General Hospital Settings
Vicky Queen Parkinsons disease nurse specialist, Torbay Hospital, Torbay and South Devon NHS Foundation Trust, Torquay, England
Parkinsons disease is a common progressive neurological condition. There are 127,000 people with the disease in the UK, that is, one in every 500 of the population. In 2014-15 there were 14,000 hospital admissions of people with PD in England. However, PD is often not the primary cause of admission. Urinary tract infections and pneumonia, for example, are frequent causes of hospital admission for people with PD. Therefore, nurses on general medical and surgical wards will often care for people with PD. This article aims to provide an update on PD and explore the nurses role in assessment and provision of safe and effective care for patients with PD in acute hospital settings.
Nursing Older People.29, 5, 30-37. doi: 10.7748/nop.2017.e861
Correspondence
Recommended Reading: Parkinson’s Phase 3 Trials
General Approach To Management
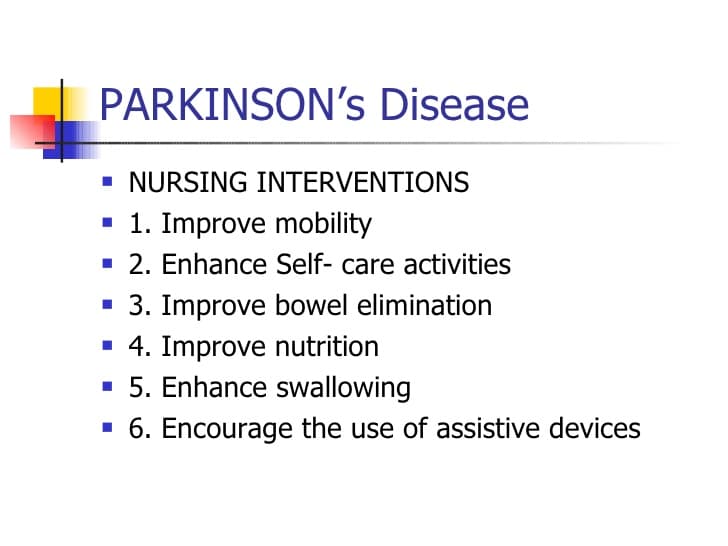
The primary goal in the management of PD is to treat the symptomatic motor and nonmotor features of the disorder, with the objective of improving the patients overall quality of life. Appropriate management requires an initial evaluation and diagnosis by a multidisciplinary team consisting of neurologists, primary care practitioners, nurses, physical therapists, social workers, and pharmacists., It is also important that the patient and his or her family have input into management decisions.
Effective management should include a combination of nonpharmacological and pharmacological strategies to maximize clinical outcomes. To date, therapies that slow the progression of PD or provide a neuroprotective effect have not been identified., Current research has focused on identifying biomarkers that may be useful in the diagnosis of early disease and on developing future disease-modifying interventions.,
Pathogenesis Of Parkinsons Disease
A number of mechanisms have been implicated in PD pathogenesis, with -synuclein aggregation central to the development of the disease. Multiple other processes are thought to be involved, with several studies suggesting that abnormal protein clearance, mitochondrial dysfunction, and neuroinflammation play a role in the onset and progression of PD. However, the relationship between these pathways remains unclear.
Recommended Reading: Stabilizing Spoon For Parkinson’s
Nursing Assessment And Interventions
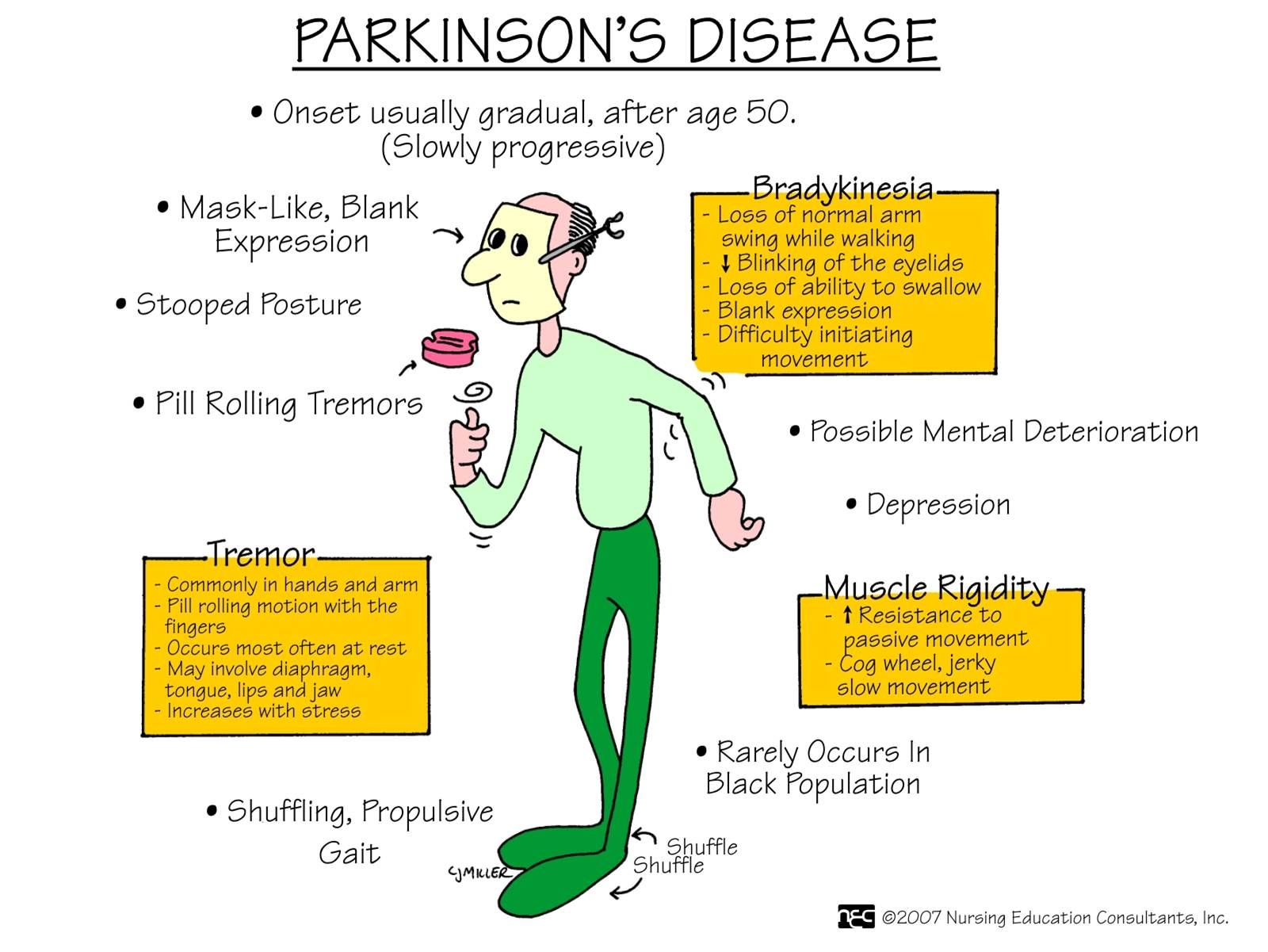
Managing Parkinson’s disease is a collaborative effort involving the patient, the patient’s family or caregiver, and the health care team. On the health care team, the role of the nurse is to provide education about PD, to help monitor medication management, and to help the patient maintain optimal functioning with as much independence as possible. PD is a complex multisystem disease. Symptoms vary from one person to the next. For each individual, symptoms change over time as the disease progresses. The nursing assessment is an ongoing process to monitor the symptoms of the disease and the effectiveness of treatment in managing these symptoms. Assessment includes: history of symptoms physical assessment and specific review of medication effectiveness or side effects.
History ofsymptoms : mobility problems, fatigue, sleep problems, eating/swallowing problems, weight gain or loss, falls, episodes of fainting or feeling light-headed, pain, muscle cramps, constipation, urinary problems, sexual dysfunction, excessive sweating, skin problems, restless leg syndrome, depression or other mood changes, hallucination or delusions, and behavior changes.
A nursing physical assessment includes: evaluation of overall appearance, weight, affect, facial expression, drooling, tremor , muscle rigidity, posture, gait, coordination, speech, skin, scalp, mental status.
Associated Clinical Features Of Probable Pdd
Associated clinical features are defined along four primary cognitive domains and a spectrum of behavioural disorders . The MDS Task Force recommended a number of tests from which the clinician could choose to assess the four primary cognitive domains and suggested that the four-item Neuropsychiatric Inventory, which covers hallucinations, depression, delusions and apathy, might be useful in assessing behavioural symptoms associated with PDD . A diagnosis of probable PDD is made on the basis of a typical profile of cognitive deficits . If dementia exists in the presence of established PD, yet the associated clinical features are not considered typical , only possible PDD should be diagnosed.
Read Also: Parkinson’s Disease Mental Health
Parkinsons Disease: Symptoms Treatment Options And Nursing Care
Phil Cotterell Parkinsons disease nurse specialist, Community Neurological Rehabilitation Team, Sussex Community NHS Foundation Trust, Worthing, England
Why you should read this article:
-
» To understand your role in supporting and improving the quality of life of patients with Parkinsons disease and their family and carers
-
» To recognise motor and non-motor symptoms of Parkinsons disease and potential treatment options
-
» To ensure the care you provide to patients is holistic and considers not only the physical effect of Parkinsons disease, but also the psychological and emotional effects that individuals may experience
Idiopathic Parkinsons disease is a progressive neurodegenerative condition that causes various motor and non-motor symptoms and will often have life-changing effects for those with the condition, as well as for their family and carers. Nurses can make a significant difference to the lives of those affected by Parkinsons disease, whether in the acute setting, community setting or in care homes. This article explores the causes and progressive clinical pathway of IPD using an evidence-based approach. It emphasises the valuable role of the multidisciplinary team and of the nurse, in particular, in monitoring and improving the quality of life of those with the condition and their family and carers.
Nursing Standard. doi: 10.7748/ns.2018.e11207
Citation
Pharmacological Treatment Of Parkinson’s Disease
There is currently no proven disease-modifying or neuroprotective therapy for PD. A summary of previous neuroprotection trials is given in a recent review article. Current evidence-based treatment for PD is symptomatic and mainly based around dopaminergic replacement or modulation . The evidence base is summarised in recent guidelines from the National Institute for Health and Care Excellence and the International Parkinson and Movement Disorder Society. Levodopa, dopamine agonists and monoamine oxidase B inhibitors are all licensed for use as initial therapy in PD. Anticholinergics are no longer routinely used due to the risk of cognitive decompensation.
Pharmacological therapies currently used for initial and adjunctive treatment of motor symptoms in Parkinson’s disease
Recommended Reading: How Do You Treat Parkinson’s Disease Naturally
Monoamine Oxidase B Inhibitors
- Selegiline hydrochloride
- Rasagiline mesylate
The enzyme monoamine oxidase B breaks down dopamine in the brain. MAO-B inhibitors prevent this breakdown, thus increasing the amount of dopamine in the brain and reducing the motor symptoms of Parkinson’s disease.
MAO-B inhibitors to treat the symptoms of PD can either be used alone or with levodopa. In early PD, they can delay the need for starting levodopa. Later in the disease, they can be given with levodopa, to enhance and prolong the effects to levodopa, thus reducing the “wearing off” phenomenon. When taken in combination with levodopa, it may allow the dose of levodopa to be reduced.
Side effects of MAO-B inhibitors include nausea, dizziness, headache, confusion, postural hypotension, hallucinations and insomnia. Confusion and hallucinations are more common in the elderly.
MAO-B inhibitors should not be used with meperidine or other opioids because of potential life-threatening drug interactions at high doses. MAO-B inhibitors at high doses could also potentially precipitate a hypertensive crisis if very large amounts of tyramine containing foods are eaten. Serious drug interactions have been reported with MAO-B inhibitors and some antidepressants.
Selegiline and rasagiline are available as standard oral tablets. An oral disintegrating selegiline tablet is also available for people who have difficulty swallowing tablets.
Training And Coaching Of Parkinsons Disease Nurse Specialists
Before the start of the study, we will organize a single training session with all participating PDNSs . The goal of this meeting is to acquire commitment to the study and uniformity in workflow by reviewing the Nursing care in Parkinsons disease guideline to explain the study specifics and to discuss practical issues related to the study intervention. In addition, PDNSs will be closely coached in order to optimize the intervention and adherence to the guideline. Every month, an experienced PD nurse from Radboudumc will have an individual intervention session with each PDNS, mainly to discuss difficult cases and to optimize the intervention and its uniformity. Finally, we will organize a video meeting every 3 months with all PDNSs to maintain their commitment, support each other, discuss difficulties related to the study, and give each other advice .
Importantly, for the purpose of this study, we will implement an increase in nursing staff capacity for participating nurses. This will allow us to study the real impact of current usual care, which would not be achieved by adding a new set of specifically trained research nurses to the existing PDNS staff. The PDNSs are all graduated nurses with a certificate in Parkinsons nursing. Furthermore, they have achieved a standard of competence as described in the Nursing care in Parkinsons disease guideline .
Don’t Miss: Parkinson’s Staring Into Space
Knowledge Deficit Related To Anti
When a medication is prescribed for treating the symptoms of Parkinson’s disease, assess the patient’s and caregiver’s knowledge of the medication. Review the purpose, the dose and schedule for taking the medication, the side effects and any special considerations regarding the specific medication. See Treatments section, Medications for a review of medications used in PD.
Diagnosis Of Parkinsons Disease
There is no specific diagnostic procedure to diagnose PD. However, the following are helpful to come up with the diagnosis:
- Medical History Taking
- Physical Examination
- Single Photon Emission CT scan -this form of imaging shows the blood flow to tissues and organs
- Dopamine transporter scan this imaging is often used to confirm the diagnosis of PD. It is not typically requested as medical history and physical examination are often conclusive.
Don’t Miss: On Off Phenomenon In Parkinson’s Disease
Data Collection And Management
Patients will be given a unique personal identification code not containing any information that refers back to the individual. The key file connecting personal identification codes to the individual patient will be stored on a secure Radboudumc data server. Only the research team has access to this key. The key file will be stored on a different server from the one with acquired study data for 5 years, allowing the research team to contact patients after they have finished the study. After 5 years, the key file will be destroyed.
Data from all paper-based case report forms completed by the researcher will be entered manually into an online certified data management system . Online CRFs will automatically be recorded in Castor EDC. When patients or caregivers are not able to complete questionnaires online, they also have the opportunity to do this on paper. We will send out the questionnaires by post, and patients can return the completed questionnaires using a self-addressed envelope. These questionnaires will be entered manually into Castor EDC. Both online and paper-based CRFs only contain the personal identification code.
Clinical notes taken by the PDNS in the online study report will also not contain any information that refers back to the individual. PDNSs are instructed to make notes according to a predefined structured format without mentioning personal information that traces back to an individual patient. The study report will be completed in Castor EDC.
Ltc Nursing Assistant Trainer December 7 2005
CNAs play a very important role in the life of Parkinson’s residents. They can assist in the following areas to help residents remain functional for many years:
Tremors-Many people with Parkinson’s disease feel embarrassed by their tremors. Suggest that they hold a book or put their hands in their pockets to try to reduce the tremor.
Walking-Encourage people with Parkinson’s to concentrate on their walking. Don’t talk or ask questions while they are walking because the distraction may bring them to a sudden stop. When Parkinson’s residents become frozen in place, sugget that they rock slightly from side to side and count out loud to get themselves moving again. Stand nearby and offer support to help them balance.
Exercise-Keep the person as mobile as possible with active or passive range-of-motion exercises. In the later stages of the disease, regular exercise helps prevent contractures.
Elimination-Fill out intake and output sheets on Parkinson’s residents to watch for constipation, which can cause fecal impaction and urinary tract infections. Both are common in residents with this disease.
Nutrition-Chewing and swallowing becomes a problem as the disease progresses. Substitute three large meals a day for six small meals a day for residents. Keep the person upright for at least 30 minutes after eating to avoid aspiration of food into the lungs.
Read Also: Interventions For Parkinson’s Disease
Encouragingthe Use Of Assistive Devices
An electric warming tray keeps food hot and permits thepatient to rest during the prolonged time that it takes to eat. Specialuten-sils also assist at mealtime. A plate that is stabilized, a nonspill cup,and eating utensils with built-up handles are useful self-help devices. Theoccupational therapist can assist in identifying appropriate adaptive devices.
Nursing Education To Improve Hospital Care For Parkinsons
A new educational program for nurses prepares them to improve hospital care for people with Parkinsons disease . The program, developed by and with nurses and tools affiliated with the Parkinsons Foundation, is described in the online March 3 edition of the Journal of Gerontological Nursing.
People with PD visit the hospital for a host of reasons, such as a disease-related fall or a urinary tract infection or for reasons unrelated to PD, such as heart problems or back surgery. Unfortunately, many people with Parkinsons find that during hospital stays, their symptoms worsen. Not only that, they tend to be hospitalized more often than their peers without PD, and hospital stay is often longer.
One reason is that hospital staff may have little experience with PD. Staff may be unaware of the complexities of Parkinsons and its symptoms. For example, its essential for people with PD to get their medications on time at the hospital. But studies have shown that, during a hospital stay, people with PD often receive their medications late, or even skip doses, and may be given other medications for pain, nausea, depression or psychosis that interfere with PD medications.
Results:
The program included the following:
What Does It Mean?
Reference
DiBartolo MC. . Enhancing Care for Hospitalized Patients With Parkinsons Disease: Development of a Formal Educational Program for Nursing Staff. Journal of Gerontological Nursing doi:10.3928/00989134-20170223-02
You May Like: How Does Occupational Therapy Help Parkinson Disease
Differences In Home Health Nursing Care For Patients With Parkinsons Disease By Stage Of Progress: Patients In Hoehn And Yahr Stages Iii Iv And V
Yumi Iwasa
1Department of Nursing, Graduate School of Health Sciences, Kobe University, Tomogaoka, Suma-ku, Kobe, Hyogo 654-0142, Japan
2Akebi Home-Visit Nursing Station, Hosoe, Shikama-ku, Himeji, Hyogo 672-8064, Japan
Abstract
1. Introduction
Parkinsons disease is a neurodegenerative disease with no radical cure. In Japan, patients above stage III on the Hoehn and Yahr scale are eligible for public medical expense subsidies. When calculated using the Japanese population, the adjusted prevalence of the disease is 166.8 per 100,000 individuals .
It is important for patients with PD in long-term medical treatment to receive physical therapy to maintain bodily functions and pharmacotherapy, centering primarily on L-Dopa, to achieve symptomatic relief both of these efforts require effective care protocols. When provided by nurses, programs that involve counseling, medication information, and collaboration with local organizations during hospitalization and discharge are known to be effective for supporting patients with PD. In the West, PD nurse specialists perform these roles and, in recent years, efforts to improve these nursing activities have resulted in studies and surveys leading to the creation of nursing practice guidelines . Due to the need to enhance the effectiveness of nursing care provided to patients with PD, the movement to maintain and further improve the quality of care is increasing globally.
2. Methods
2.1. Participants and Collected Data
3. Results
Inpatient Management Of Parkinson’s Disease
Patients with PD are often admitted to hospital for other reasons, but the unique challenges of the condition mean that outcomes related to PD are often suboptimal. Many hospitals have an alert system to inform members of the PD team of admission to allow proactive in-reach consultations. It is essential that antiparkinsonian medications are given on time and in correct dosage, as sudden reduction or withdrawal of medication can lead to severe morbidity or even mortality due to parkinsonismhyperpyrexia syndrome. Dopamine blocking drugs must not be given. When patients with PD cannot take their usual oral medications, we recommend that an equivalent dosage be given via nasogastric tube. If this is not possible, or enteral medication is contraindicated, cautious use of rotigotine patch can be helpful.
Recommended Reading: Are There Service Dogs For Parkinson’s Patients