Thanks For Signing Up
We are proud to have you as a part of our community. To ensure you receive the latest Parkinsons news, research updates and more, please check your email for a message from us. If you do not see our email, it may be in your spam folder. Just mark as not spam and you should receive our emails as expected.
Recommended Reading: Parkinsons Hallucinations Commercial
Stereotactic Dbs Vs Interventional Image
Stereotactic DBS surgery requires the patient to be off their medication. During the procedure, a frame stabilizes the head and provides coordinates to help the surgeons guide the lead to the correct location in the brain. The patient gets local anesthesia to keep them comfortable throughout each step along with a mild sedative to help them relax.
During image-guided DBS surgery, such as with interventional MRI or CT scan, the patient is often asleep under general anesthesia while the surgeon uses images of the brain to guide the lead to its target.
Some advanced centers offer both the stereotactic and iMRI-guided options for DBS surgery. In this case, the doctor and patient will discuss which procedure is better based on a number of factors.
For instance, the doctor may recommend an image-guided procedure for children, patients who have extreme symptoms, those who are especially anxious or fearful or those whose leads are going into certain parts of the brain.
Generally, DBS surgery follows this process:
What Is The Patient Selection For Dbs
Parkinsons disease:
- Confirmed diagnosis of Parkinsons disease for four years or more
- Responsiveness to levodopa medicine
Having one or more of the below:
- Motor fluctuations in which you have wearing-off periods when symptoms return because medicine isnt working well. These include tremor, stiffness and slowness of movement
- Prominent tremor
- Uncontrolled, involuntary movements known as dyskinesia
Ideal candidates with dystonia and tremor are those who have not responded well to medicine options or, in the case of dystonia, additional procedural options like Botox injections.
Read Also: Anesthesia Drugs To Avoid With Parkinson’s
When Should I Call My Healthcare Provider Or Go To The Hospital
Because DBS involves surgery especially the procedure on your brain there are some warning signs you shouldn’t ignore. You should call your healthcare provider immediately or go to the hospital outside of business hours if you have the following symptoms:
- Severe headache that happens suddenly or wont go away.
- Bleeding from your incisions.
What Are The Risks
No surgery is without risks. General complications of any surgery include bleeding, infection, blood clots, and reactions to anesthesia. Complications related to placement of the DBS lead include seizures, infection, and a 1% chance of bleeding in the brain.
Reasons for which you might need additional surgery include breakage of the extension wire in the neck parts may wear through the skin and removal of the device due to infection or mechanical failure. If you have a non-rechargeable DBS system, the battery will need to be replaced every 3 to 5 years. Rechargeable DBS systems have a battery that lasts 10 to 15 years.
DBS may also cause worsening of some symptoms such as speech and balance impairments. In some patients with Parkinson’s, DBS may cause or worsen depression. If you develop any side effects from a stimulation adjustment, you need to return to the office for further programming.
Also Check: Michael J Fox Cure For Parkinson’s
High Content Screening In Neuroscience
In neuroscience, HCS has been used in two major areas: neural regeneration and neuroprotection. There are also a series of primary neurons used in HCS, such as cerebellar granule neurons , dorsal root ganglion neurons, hippocampal neurons, cortical neurons, spinal cord neurons, retinal ganglion cells , and Drosophila neurons. Through quantitative analysis of complex cell phenotypes, it is helpful for the development of drugs against neurological diseases
Fig.1 Current trends in high-content analysis in biomedicine.
What Happens After Surgery
After surgery, you may take your regular dose of Parkinson’s medication immediately. You are kept overnight for monitoring and observation. Most patients are discharged home the next day.
During the recovery time after implanting the electrodes, you may feel better than normal. Brain swelling around the electrode tip causes a lesion effect that lasts a couple days to weeks. This temporary effect is a good predictor of your outcome once the stimulator is implanted and programmed.
About a week later, you will return to the hospital for outpatient surgery to implant the stimulator in the chest/abdomen. This surgery is performed under general anesthesia and takes about an hour. Patients go home the same day.
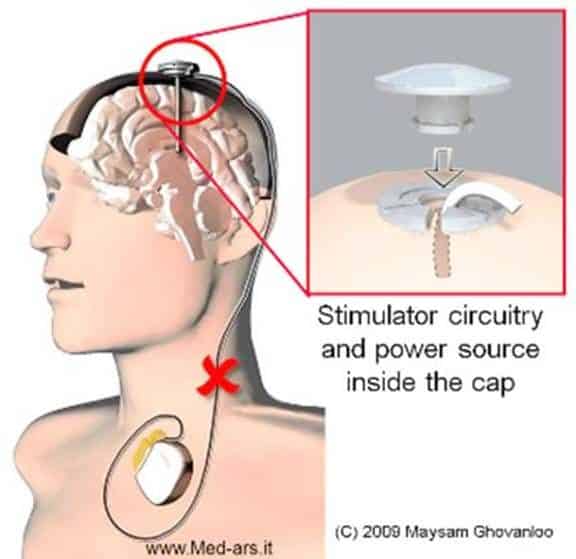
Step 7: implant the stimulator You will be taken to the OR and put to sleep with general anesthesia. A portion of the scalp incision is reopened to access the leads. A small incision is made near the collarbone and the neurostimulator is implanted under the skin. The lead is attached to an extension wire that is passed under the skin of the scalp, down the neck, to the stimulator/battery in the chest or abdomen. The device will be visible as a small bulge under the skin, but it is usually not seen under clothes.
You will have lifting and activity restrictions for 6-8 weeks while the incisions heal. Follow all discharge instructions and the neck exercises provided. Incision pain can be managed with medication.
Read Also: Lifestyle Changes For Parkinson’s Disease
Placement Of The Neurostimulator
This procedure takes place under general anesthesia so that the person is asleep. The surgical team inserts the neurostimulator under the outer layers of skin, usually just under the collarbone, but sometimes in the chest or abdomen. The extension wire from the lead is attached to the neurostimulator.
Who Can Get Dbs
Deep brain stimulation is a relatively new treatment for epilepsy, but it’s been used for some time to treat Parkinson’s disease and other conditions. If you have epilepsy and other treatments have failed to reduce seizure activity, you may be considered for DBS therapy.
Whether you are a candidate for this treatment depends on your specific type of seizure activity, your overall health, and whether you meet other criteria your surgeon may require.
You May Like: Stage 2 Parkinson’s Disease
Overview Of Parkinson’s Disease
James Parkinson revealed a detailed description of six patients with shaking palsy in 1817 and after his death, the mentioned description known as Parkinson’s disease , which is now the most common neurodegenerative disorder after Alzheimer’s disease. The pathological hallmark of PD is the degeneration of dopaminergic neurons of the substantia nigra pars compacta . The loss of this neuronal population results in functional imbalances in the nigrostriatal pathway, leading to lowering the level of dopamine in the striatum. This leads to motor dysfunction and the development of the classical symptoms of PD. Motor symptoms including resting tremor, bradykinesia, and rigidity of skeletal muscle, postural instability, stooped posture, and freezing of gait are clinical symptoms in PD. Furthermore, non-motor symptoms such as cognitive and behavioral problems, besides sensory impairments are seen in the patients. The prevalence of PD is approximately 0.3 % in the general population in developed countries and affects about 1% of those older than 60 and it is unusual to occur before the age of 50. Notably, men are at higher risk than women.
Fig.1 The dopaminergic neuron and the nigrostriatal pathway.
Testing Before Deep Brain Stimulation
For patients with Parkinsons disease, the doctor must confirm that the PD is levodopa-responsive and determine which symptoms are most likely to respond to DBS and discuss these with the patient.
To accomplish these two objectives, the movement disorders neurologist will examine the patient in the absence of his or her PD medications, then again after having taken them. Seeing the effect of PD medications on the movement and non-motor symptoms helps the physician and patient identify good target symptoms for DBS.
A cognitive assessment can help determine a persons ability to participate in the procedure, which involves providing feedback to the doctor during surgery and throughout the neurostimulator adjustment process. This assessment also informs the team of the risk of having worsened confusion or cognitive problems following the procedure.
Some hospitals also perform an occupational therapy review or speech, language and swallowing assessment. A psychiatrist may examine the person to determine if a condition such as depression or anxiety requires treatment before the DBS procedure.
Recommended Reading: Does Vitamin B12 Help Parkinsons
Also Check: Social Security Blue Book Parkinson’s
Deep Brain Stimulation For Epilepsy
Deep brain stimulation is a therapy that may help reduce seizure activity in those with certain types of epilepsy. This treatment is usually reserved for people whose seizures haven’t responded to other medications or therapies. DBS is a relatively new tool for epilepsy, and further studies may reveal additional uses.
This article discusses how deep brain stimulation is used, what the DBS device does inside your brain, how it’s implanted, and what to expect after starting treatment.
Westend61 / Getty Images
Deep Brain Stimulation For Movement Disorders
Deep brain stimulation has been approved for the treatment of movement disorders since the 1990s. Numerous studies have proven this surgerys superiority to medical therapy alone. The time to consider DBS surgery is when the quality of life is no longer acceptable on optimal medical therapy as administered by a movement disorder specialist. DBS surgery is very safe and recent advancements in device technology have improved patient outcomes as well.
Don’t Miss: Sleep Medications For Parkinson’s Patients
Experience Fewer Symptoms With Deep Brainstimulation
For patients with movement disorders, such as Parkinson’s disease and essential tremor, an effective treatment is available to help significantly reduce their symptoms and make performing daily activities easier.
For appointments
Deep brain stimulation is a therapy used to treat multiple disorders. The most common disorders include Parkinsons disease and essential tremor. It can be used to improve a patients:
- Abnormal muscle activation
It is also being studied in a few psychiatric conditions such as obsessive-compulsive disorder, Tourettes syndrome, depression and addiction.
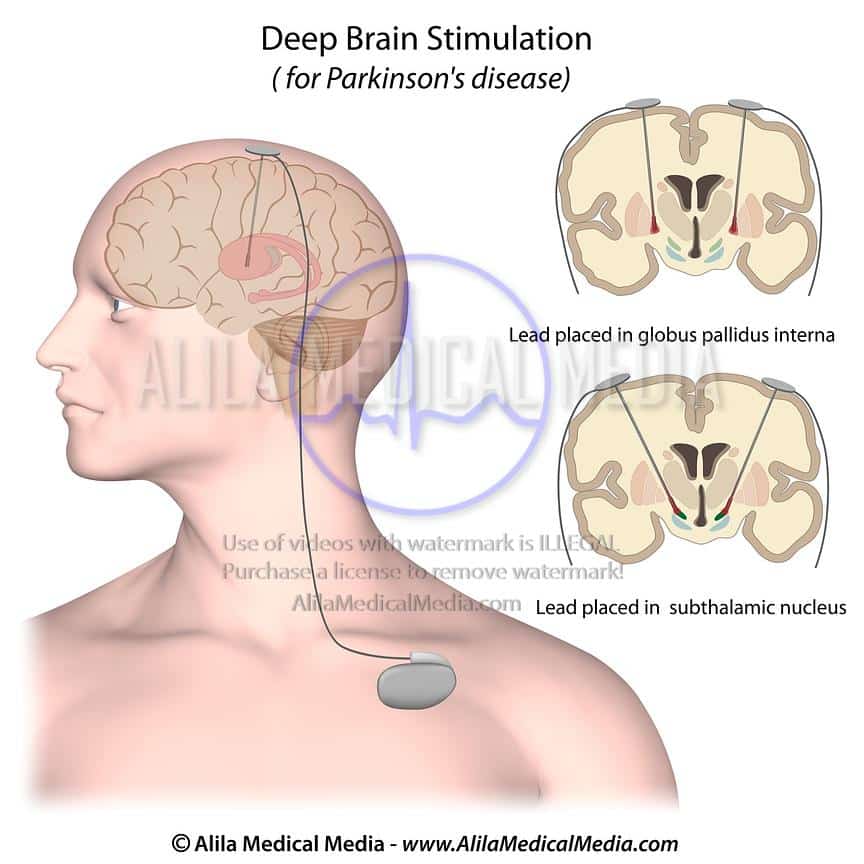
About DBS surgery
The procedure involves placement of an electrode or lead into a deep structure of the brain typically, one on each side of the brain. These electrodes are secured in place with a plastic cap and connected to extension wires that are tunneled underneath the skin to an implanted generator placed under the skin just below the collar bone, similar to a pacemaker.
The generators last for 3-15 years depending on type implanted and patient use. They are replaced with a simple outpatient surgery. The overall risk of the operation is very low but not zero. In depth discussion with your neurologist and surgeon is needed to determine if you are an appropriate candidate and your risk of the operation.
For above images: ©2021 Medtronic. All rights reserved. Used with the permission of Medtronic.
How Is The Surgery Performed
UPMC was one of the first centers to use ROSA robotic assistance for the placement of DBS electrodes. ROSA is similar to a GPS device for the brain. It provides the surgeon with a roadmap to reach the intended brain targets. The patient is sedated for the beginning of the surgery while we make a small opening in the skin and bone at the surgical site. The patient will not feel or remember this part of the surgery, but once these steps are complete, he is awoken for the remainder of the surgery.
Brain MappingWe use neurophysiology recordings from very thin electrodes inserted into the brain to map activity in the intended target and confirm the best spot for the DBS electrode. It is important for the patient to be awake during this part of the surgery so we can obtain the best recordings possible, which will aid in the most accurate placement of the DBS electrode. The brain mapping is not painful and the surgical team will be available to provide reassurance and feedback the entire time.
Intra-Operative Stimulation TestingWhen the best site is identified from the brain mapping, the DBS electrode is inserted and tested. We monitor the patient for improvement in his symptoms, for example tremor, and also ask him to report any new sensations he experiences. Again, this part of the procedure is not painful, but provides valuable feedback to the surgical team.
Recommended Reading: Tce Exposure And Parkinson’s
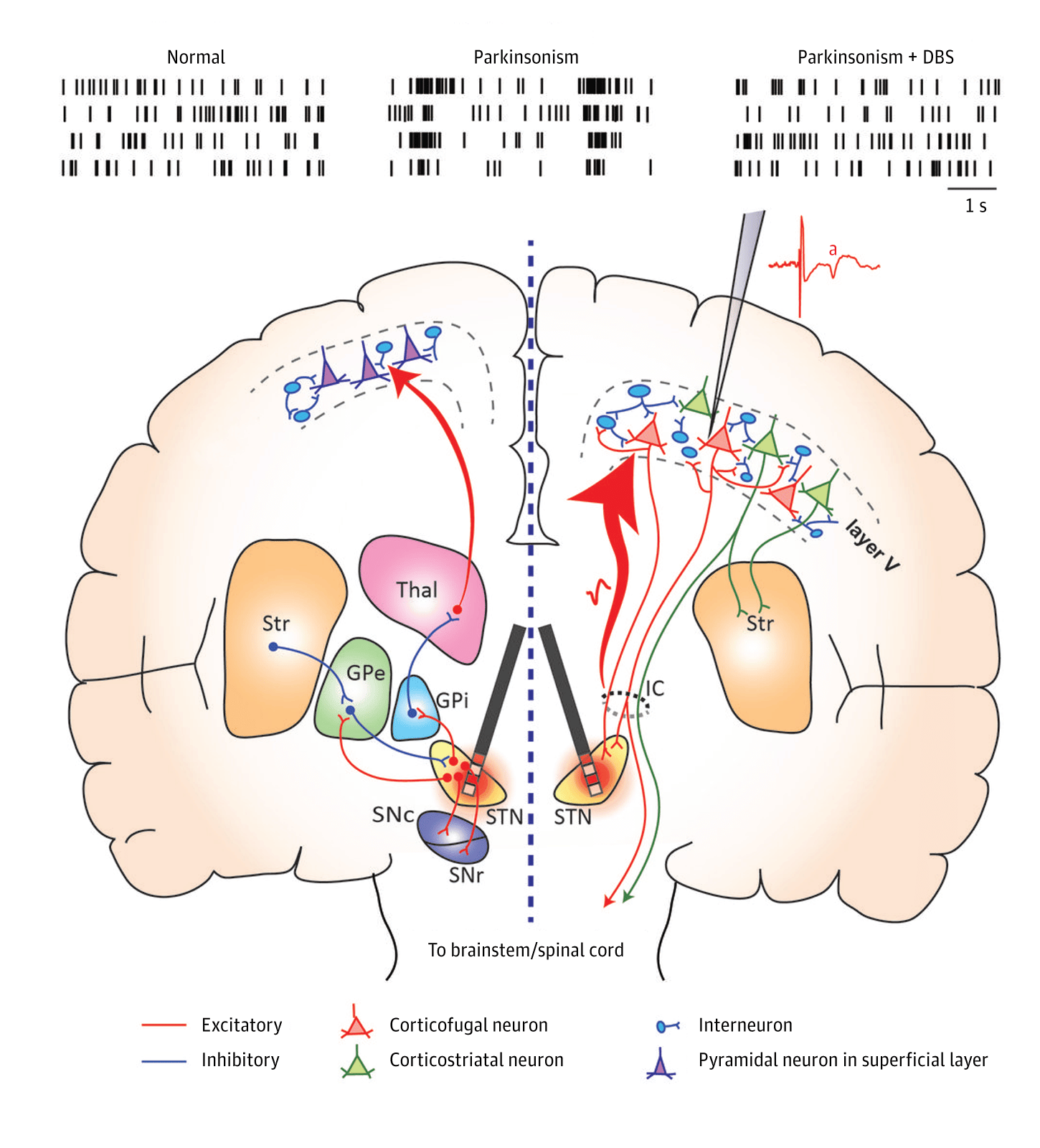
Pallidal Stimulation Versus Subthalamic Stimulation
As mentioned, there are two main anatomic targets for using DBS to treat PD the STN and the GPi. There have been several large randomized studies comparing STN and GPi DBS in PD. It is suggested that both STN DBS and GPi DBS overall equally and successfully improve motor symptom, and are similar in cost-effectiveness. However, although no differences were observed in the on phase between STN DBS and GPi DBS, significant differences were seen in the off phase STN DBS was more effective in terms of motor function improvement in the off phase. There are different opinions in terms of effects of STN DBS and GPi DBS on quality of life. Some authors have found no significant difference between the STN and GPi targets. However, others agree with that greater improvements in quality-of-life measures are achieved in patients with GPi DBS.
GPi DBS can be used for patients with more axial symptoms, gait issues, dyskinesias, depression, and word fluency problems. STN DBS is often favored in reducing medication post surgery, and for patients with greater tremor. STN-DBS has also demonstrated an improvement in the quality of sleep for patients.
Dont Miss: Does Sam Waterston Have Parkinsons
Importance Of In Vitro Models In Pd
Animal models are useful for investigating PD progression as they are amenable to behavioral tests. However, as humans are the only species that develop neurodegenerative disorders, it is necessary to induce dopaminergic damage and/or LB pathology in these models. To date, no model has recreated the full spectrum of PD, which makes it difficult to evaluate molecular mechanisms and translate these findings to humans. In vitro models present a controlled environment that facilitates investigations of molecular and cellular pathophysiological mechanisms of dopaminergic degeneration in PD and the screening of potential therapeutics.
Fig. 2 In vitro models of Parkinson’s disease.
You May Like: How Does Parkinson’s Affect The Nervous System
Efficacy Of Local Versus General Anesthesia Techniques
A meta-analysis of 145 studies of DBS in PD showed that the mean target error was not significantly different between LA and GA however the mean number of DBS lead passes were significantly less with GA as compared to LA .62 Post DBS complications were significantly lower with GA . The two techniques did not differ significantly in UPDRS II scores off medication, UPDRS III scores off and on medication or LED. UPDRS IV off medication score decreased more significantly in awake DBS versus sleep DBS cohorts .62 Hence, most DBS procedures should ideally be carried out under LA due to the lower side effect profile.
Conflict Of Interest Statement
PH is the director of the Duke University Parkinson Disease and Movement Disorders fellowship, which receives grant support from Medtronic. MS works for Duke University, and has received consultancy fees from Eli Lilly, Merz, Osmotica, Pfizer, SK Life Sciences, Allergan, Avid, Best Doctors, Biotie, Lundbeck, Neuronova, Novartis Pharma , Saraepta Therapeutics, and Sunovion Pharmaceutics, Inc. Dr. MS has also received grants from the Michael J. Fox Foundation, the NIH, the Parkinson Study Group, and Pharma 2B, royalties from Informa Press for the Handbook of Dystonia and Duke University for the Wearing Off Questionnaire. He has also received payment for development of educational presentations from the University of Kansas, the University of Miami, and the University of Rochester. Dr. MS also received paid travel accommodations from the Cleveland Clinic Neurological Institute, the Movement Disorder Society, and the National Parkinson Foundation.
Recommended Reading: Ed Begley Jr Parkinson’s
How Does Deep Brain Stimulation For Parkinsons Work
Deep brain stimulation works by modifying abnormal electrical activity in the brain. It was first approved for Parkinsons tremors in 1997 and has become an established treatment to control additional motor symptoms of Parkinsons disease.
DBS involves three main components:
- Leads: Leads are implanted in the brain in a region responsible for motor activity.
- Implantable pulse generator : A separate procedure is performed to implant a battery-operated device in the chest or in the abdomen. An IPG is similar to a pacemaker for the heart and has been coined by some as a pacemaker for the brain.
- Extension: A thin, insulated wire is passed beneath the skin between the leads and implantable pulse generator to deliver the electrical stimulation from the pulse generator to the leads.
The target area in the brain is first identified by magnetic resonance imaging or computed tomography . Then, the leads are placed via small holes that a surgeon drills in the skull.
This is considered a minimally invasive surgery that is done in the operating room with local anesthesia. It usually requires an overnight stay.
The IPG is inserted in a separate surgical procedure in the operating room roughly a week later.
After a few weeks, a neurologist begins to program the unit. This process can take several additional weeks to months. When this is completed, people are able to manage the device with a handheld remote control.
Services At Creative Biolabs
As an industry leading CRO, Creative Biolabs has thrown a great deal of manpower, material, and financial resources into in vitro CNS diseases modeling platform. After years of hard work, our platform has finally been completely optimized and opened to customers around the world. We are now capable of offering a variety of custom ex vivo CNS diseases model services, including Parkinson’s disease model.
If you are interested in our custom disease model services, or any other custom CNS diseases modeling services on our websites, please don’t hesitate to contact us for more information.
Reference
For Research Use Only. Not For Clinical Use.
Read Also: How To Stop The Progression Of Parkinson’s Disease