What Treatments Are Available For Utis
The first line of treatment for many people who develop UTIs is a course of antibiotics. Often, this is the only treatment needed. Several different antibiotics can treat UTIs, and your provider will use results from a urine sample to determine which is right for you.
If the UTI is considered complicated , your doctor might prescribe a higher dose of antibiotics. If the infection is severe or in your kidneys, your physician may refer you to the hospital for high-dose antibiotics administered through an IV.
Urinary Problems In Parkinsons Disease
This 1-hour webinar is an interview with Dr. Janis Miyasaki, Dr. Jorges Juncos, and retired movement disorder specialist and young onset Parkinsons patient, Dr. Maria De Leon. They discuss the effect of Parkinsons disease on the autonomic nervous system, which regulates many body functions, including bladder control. Urinary problem diagnosis, symptom management and ongoing research on the topic wrap up the hour.
Recommended Reading: Similar To Parkinsons
Parkinson’s Disease And Voiding Dysfunction
In this 54-minute webinar, urologist Dr. Sidney Radomski explains how voiding function is affected by Parkinsons disease in both men and women. He discusses how an enlarged prostate contributes to voiding problems and management options of voiding dysfunction for those with Parkinsons disease and MSA.
Also Check: Can Parkinson’s Disease Cause Death
Management Of Sexual Dysfunction
Management of sexual dysfunction in patients with PD includes both behavioural and pharmacological options depending on the nature of the sexual dysfunction. Behavioural therapy may be used to treat SD, if considered as a learned maladaptive behaviour and may involve the use of psychodynamic psychotherapy and cognitive behavioural therapy . Pharmacological treatment of SD, on the other hand, requires either the reduction or elimination of drugs interfering with the sexual function or the introduction of drugs that improves sexual function . Ultimately, treatment options for SD may require multidisciplinary input from neurologists and psychologists for optimum results . Although phosphodiesterase 5 inhibitors are standard treatment option for erectile dysfunction , intracavernosal alprostadil 1.2510 g injections can be used.
The management of hypersexuality as part of an impulse control disorder includes reduction/stopping of dopamine receptor agonist and practical therapeutic strategies including psychological therapies but not limited to counselling, psychotherapy, sex, couple and behavioural therapies . Hormonal treatment specifically testosterone has been tried in PD .
What You Need To Know About Urinary Tract Infections And Parkinsons
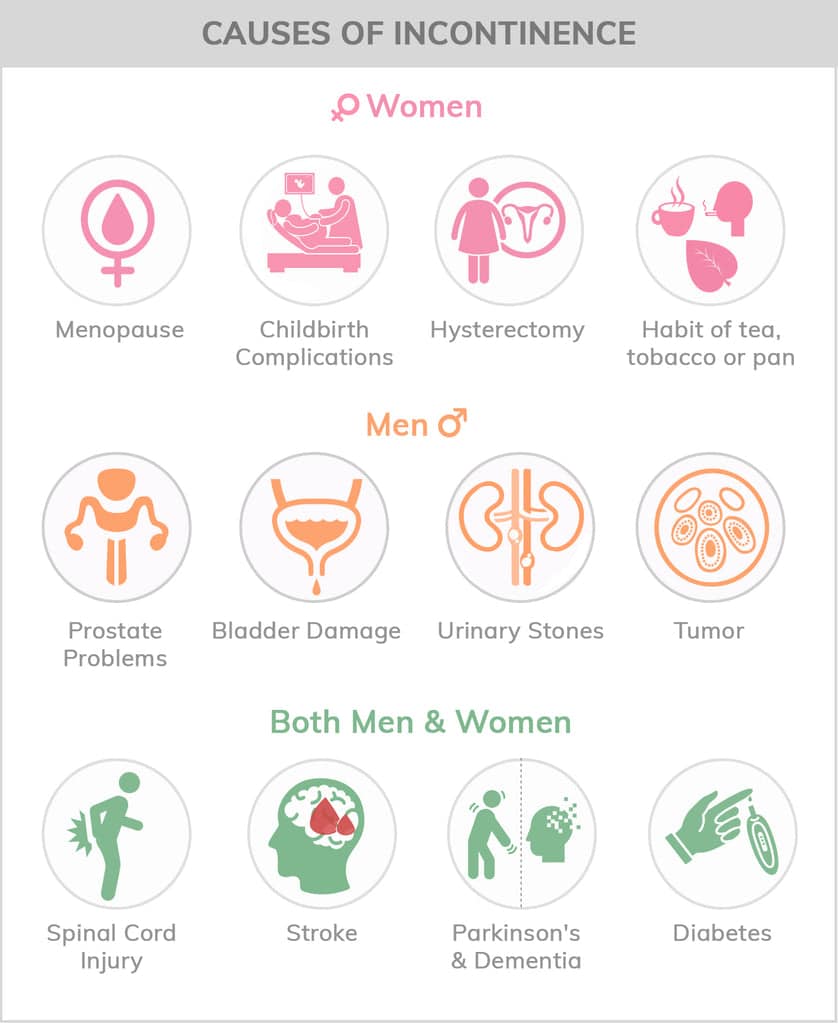
Your autonomic nervous system regulates your bodys automatic functions, such as controlling blood pressure, sweat and temperature, digestion, heart rate, and urination. In Parkinsons, these are referred to as non-motor symptoms. And of these, one of the more common ones people with Parkinsons face are those related to urination, such as urgency, frequency of urination, incontinence, and nocturia. Together, these symptoms put people with Parkinsons at greater risk of developing urinary tract infections .
Although UTIs are common, especially in women, people with Parkinsons have a higher risk of these infections than people without Parkinsons. UTIs can also significantly impact your Parkinsons symptoms and increase your risks of falls, cognitive decline, and hospitalization. For this reason, you must understand the risk factors, symptoms, prevention strategies, and treatment options available. The good news is that there are numerous ways you can decrease your risk of developing a UTI and treat the infection if one occurs. In this post, we share information about the causes and symptoms of UTIs and how Parkinsons increases your risk of developing one so you can recognize symptoms, get proper treatment, and prevent UTIs from developing in the first place.
Recommended Reading: Very Early Signs Of Parkinson’s Disease
Urinary Retention And Stasis
As previously mentioned, advanced PD may predispose to urinary retention through a variety of mechanisms. One Korean study of 197 PD patients found that 8.9% had increased post-void residual volumes over 100cc, a well-established risk factor for UTI . Another potential mechanism involves motor dysfunction itself, as patients with advanced PD may have severe rigidity/akinesia preventing access to toileting. Additionally, as PD patients may be at higher risk for urinary incontinence, they may be prescribed anticholinergics, which may independently contribute to an increased risk of UTI . Caution should be taken when titrating antimuscarinic agents on patients with advanced PD and PD dementia to avoid the risk of drug-induced urinary retention. PD patients with cognitive impairment and spastic bladder may benefit from timed or prompted voiding to prevent episodes of urinary incontinence and avoid the need for antimuscarinic therapy, as discussed in further detail below under Management strategies to prevent UTI in PD.
Parkinsons Drugs And Their Side Effects On Kidneys
Parkinsons drugs have also been researched for kidney damage. Although it can be seen as a side effect of many Parkinsons drugs, There is no solid evidence, and many studies are underway. In a research, a 90-year-old parkinsonian woman treated with
Levodopa-Benserazide and Bornaprine developed rhabdomyolysis and were found unconscious on the floor.
Although there is little evidence, some clinical cases have been observed.
Don’t Miss: Housing For Parkinson’s Patients
How Can A Neurodegenerative Disease Cause A Kidney Problem Can Parkinsons Cause Kidney Problems
Some studies have shown a relationship between chronic kidney disease and Parkinsons disease. Chronic kidney disease and Parkinsons disease both share many common risk factors, such as:
Although, its not common to come across patients with Parkinsons disease and chronic kidney disease with its associations.
Parkinsons disease has been shown to affect the kidney by causing chronic kidney disease or end-stagerenal disease. This can result in several metabolic derangements, hypoxia, toxins, and acidosis, which cause brain edema, particularly basal ganglia. This will lead to permanent Parkinsons disease due to cytotoxic derangements by damaged kidneys.
A kidney transplant can be a way out of the vicious cycle thought to be created between Parkinsons disease and kidney damage.
Along with the transplant, the immunosuppressants given in the process can act as a preventive measure for the permanent development of Parkinsons disease. This happens by interfering with the pathophysiology and reducing inflammations.
Another cause is triggered acute renal failure, mainly due to rhabdomyolysis. Parkinsons disease can be further more complicated due to rhabdomyolysis. This can lead to a sudden renal shutdown, i.e., Acute renal failure.
There can be two types of cases with rhabdomyolysis, one complicated by oligo-anuric renal failure, and this usually occurs in patients with Parkinsons disease.
Identifying And Reporting Uti In Pd
Cognitively intact patients with urinary symptoms should have testing with a urinary dipstick as an initial measure to evaluate for the presence of nitrite or leukocyte esterase or, alternatively, a urinalysis to detect pyuria. Although urinary culture is not required in all cases of uncomplicated UTI, it is preferred to document speciation and susceptibility to antibiotics . In cognitively impaired patients in whom self-reporting of urinary symptoms may be limited, an acute change in mental status, with or without localizable genitourinary symptoms, such as dysuria, urgency, or suprapubic pain, should prompt diagnostic testing for UTI . Heightened suspicion for UTI is appropriate when these symptoms occur in combination, as demonstrated in a study of nursing home residents that showed that the combination of dysuria with either a change in the character of the patients urine or mental status predicted the presence of bacteriuria plus pyuria in 63% of cases . In the future, new technologies may evolve to allow for serial monitoring or automated detection of UTI, perhaps with the use of smart-diapers with built in urinalysis capability .
You May Like: What Fruits Are Good For Parkinson’s
Bladder And Constipation Problems
Parkinsons commonly leads to problems with constipation and bladder control, including urinary urgency, frequency, retention and nocturia.
These problems add to the challenge of living with Parkinsons and can have a negative effect on a persons quality of life. It is important to seek help in managing these problems, as both issues can be effectively managed.
Increased Risk Of Overactive Bladder In Patients With Idiopathic Parkinsons Disease: Insight From A Nationwide Population
-
Roles Conceptualization, Investigation, Methodology, Writing original draft
Affiliation Department of Neurology, China Medical University Hospital, China Medical University School of Medicine, Taichung, Taiwan
-
Affiliation Department of Neurology, China Medical University Hospital, China Medical University School of Medicine, Taichung, Taiwan
- Cheng-Li Lin,
Roles Data curation, Formal analysis, Project administration
Affiliations College of Medicine, China Medical University, Taichung, Taiwan, Management Office for Health Data, China Medical University Hospital, Taichung, Taiwan
-
* E-mail:
Affiliations National Institute of Environmental Health Sciences, National Health Research Institutes, Miaoli, Taiwan, Institute of Occupational Medicine and Industrial Hygiene, College of Public Health, National Taiwan University, Taipei, Taiwan, Ph.D. Program in Environmental and Occupational Medicine, Kaohsiung Medical University, Kaohsiung, Taiwan
Read Also: Focused Ultrasound Therapy For Parkinson’s
How Does Parkinsons Impact The Risk Of Getting Utis
In Parkinsons, the brains control of the urinary sphincter can become disrupted, leading to difficulty holding urine. As a result, people with Parkinsons may experience storage symptoms, which can increase the frequency and/or urgency of urination and lead to nocturia when you wake up multiple times at night to go to the bathroom. Another set of urinary symptoms, called voiding symptoms, can cause urination hesitancy, straining, interrupted stream, and double voiding . You may experience symptoms in both sets, which puts you at a higher risk of developing a UTI.
Voiding symptoms often go unnoticed for longer than storage symptoms do, and they can play a significant role in the development of UTIs. For example, if they keep you from fully emptying your bladder each time you urinate or keep you from urinating as often as you should, bacteria can grow and spread in the remaining urine, leading to UTIs.
Parkinsons motor symptoms can also impact your ability to urinate as frequently. Slowness and stiffness can make it difficult to get to the bathroom. In addition, if you experience significant balance issues, you may not travel to the bathroom as often as you need to for fear of falling.
Evaluating And Treating Urinary Issues In Parkinsons Disease Multiple System Atrophy And The Other Atypical Parkinsonism Disorders
In this hour-long webinar, neuro-urologist Ekene Enemchukwu, MD focuses on urinary incontinence, overactive bladder, urinary retention, and other urinary issues in PD, MSA, and the atypical parkinsonism disorders. Following the presentation, moderator Candy Welch, Brain Support Networks MSA caregiver support group leader, asks Dr. Enemchukwu many questions submitted by webinar participants.
Also Check: How Long Does It Take For Parkinson Medication To Work
Clean Intermittent Self Catheterization
The finding of a high post-void residue is unusual in patients with PD. If the PVR volume is consistently more than 100 mL, clean intermittent catheterization has been advocated. Specific issues related to dexterity in PD may make this challenging. Experienced health-care professionals, such as a continence adviser, should be involved in teaching the technique and exploring possible barriers to successful catheterization. Complications include UTI and trauma .
Dont Miss: What Happens If Parkinsons Is Left Untreated
Introduction Of Bacteria Via Catheterization
Indwelling urinary catheterization provides a direct pathway for pathogenic bacteria to ascend from the external environment to the lower urinary tract. There are three possible mechanisms by which catheterization may lead to bacterial colonization of the lower urinary tract and subsequent infection . First, bacteria may be introduced directly during catheter insertion if aseptic technique is not observed. Secondly, bacteria may travel along the outside of the catheter, between the urethral mucosa and the exterior of the catheter. Lastly, bacteria may ascend directly along the interior lumen of the catheter. Overall, extraluminal tracking of bacteria seems to be the predominant pathophysiologic mechanism of catheter-associated UTI , with biofilm formation playing a role in some cases . Bacteriuria is virtually guaranteed with indwelling urinary catheterization and is more likely with prolonged duration of catheterization.
Don’t Miss: Parkinson’s Disease Journal Articles
Bladder Problems In Parkinsons
The primary function of the bladder is twofold to store urine as it is made and then to empty the urine. With Parkinsons, problems can emerge in both areas.
Recent studies suggest that 30-40% of people with Parkinsons have urinary difficulties. Despite the frequency of urinary dysfunction, actual urinary incontinence is relatively uncommon. Troublesome incontinence develops in only about 15% of people with Parkinsons.
The most common urinary symptoms experienced by people with Parkinsons are:
- The need to urinate frequently
- Trouble delaying urination once the need is perceived, creating a sense of urinary urgency
These symptoms usually mean you have an irritable or overactive bladder. Your bladder is signaling the brain that it is full and needs to empty when, in fact, it is not. This can happen at any time, so you might have to get up multiple times during the night to go to the bathroom.
Impairment of bladder emptying is a less frequent but still troublesome feature of urinary dysfunction in Parkinsons. This may be caused by delay or difficulty in relaxation of the urethral sphincter muscles. These muscles must relax for the bladder to empty. This can result in hesitancy in initiating urination, difficulty in generating a stream and incomplete emptying of the bladder. Dystonia involuntary muscle contractions of the urethral sphincter has also been described.
Symptoms Of Urinary Retention
The symptoms of urinary retention are not always obvious but may include
- Hesitancy really having to strain to pass urine
- Strong feelings of urgency and frequency and when passing urine only a small amount comes out
- A urinary stream that is very weak and intermittent
Whilst your bladder is not emptying properly there is a risk that the residual urine in the bladder will become infected. This could cause further complications and problems if it isnt removed regularly. It is important to seek help if you experience any of the above symptoms.
It is a good idea to keep a record of your bladder activity in a bladder diary for a few days before your appointment with your doctor or nurse.
Your Doctor or Healthcare Professional may recommend the following tests:
Recommended Reading: Cialis And Parkinsons Disease
Read Also: What Causes Parkinson’s Symptoms
Prevalence Of Nocturia In Pd
Questionnaire based studies generally report a high prevalence of nocturia, with figures ranging between 76% and 86%,, though one study reported a prevalence of only 34.6%. In a study of 115 PD patients using a questionnaire on pelvic organ functions, Sakakibara et al. reported nocturia in 53% of men and 63% of women with PD.
Nocturia has been reported in 34.6% of PD patients using a semistructured interview in 1,072 consecutive patients with PD in the large, multicentric PRIAMO study.
This apparent variability in prevalence between studies could be put down to several factors, including differences in the demographic features of the cohort of patients being studied, and the occurrence of medical comorbidities. LUT symptoms are more prevalent with advancing disease and were most frequent in patients at H & Y stage 4 to 5 with a reported prevalence of around 90%. Moreover, the term nocturia has been applied differently in studies and the prevalence varies according to the definition being used. The International Continence Society made an attempt to standardize the definition of nocturia in 2002 and, based on a consensual approach, put forward the complaint that the individual has to wake at night one or more times to void.
Parkinsons Disease And The Bladder
In this 30-minute video lecture Dr. Donna Deng explains the cause of bladder dysfunction and quality of life consequences. Treatment options include behavioral modification, pharmacologic, nerve stimulation , Implantable Impulse Generator, and Botox injections. Last line of treatment for older men with Parkinsons should be prostate surgical procedures.
Recommended Reading: Medications For Parkinson’s Disease And Side Effects
What You Can Do To Help
- Discuss bladder problems with your family doctor or neurologist, who may perform some tests to rule out urinary tract infection or other problems.
- Speak with your family doctor or neurologist about a referral to a urologist . The urologist will be able to look into any bladder symptoms and provide treatment plans.
- Be aware that bladder difficulties can be a sign of wearing off. Wearing off is where some of the symptoms of Parkinsons occur or worsen between doses of medication and are related to the level of medication becoming too low. Taking your medication on time every time helps reduce fluctuations and that will help reduce bladder difficulties.
- Managing constipation and making sure that you have regular bowel movements will also assist in minimising bladder problems.
Treatment For Over Active Bladder In Parkinsons
Overactive bladder affects up to 27% of men and 43% of women of the global population. Now, add a neurological condition and the problem becomes more challenging. First, there is a list of medications which make the problem worse, so should be avoided. Then, a thorough evaluation and physical exam. Treatment depends on the cause, but evaluating all medications and an adjustment of dopamine medication is often necessary. If you are still having problems, five further treatment options are included.
Recommended Reading: Parkinson’s Disease Constipation Treatment
Increasing Your Fibre Intake
Eating the right amount of fibre and drinking enough fluids can help if you have constipation.
To get more fibre in your diet:
- choose a breakfast cereal containing wheat, wheat bran or oats, such as Weetabix, porridge or bran flakes.
- eat more vegetables, especially peas, beans and lentils.
- eat more fruit fresh, stewed, tinned or dried. High fibre fruits include prunes or oranges.
- drink plenty of fluids throughout the day to avoid dehydration. Lots of fluids are suitable, including water, fruit juice,
- milk, tea and squashes. Cut out caffeine to avoid overstimulation of your bladder.
If you find it difficult chewing high-fibre food, you can get some types which dissolve in water. You can also get drinks which are high in fibre.
Try to increase how much fibre you get gradually to avoid bloating or flatulence .
A dietitian can give you further advice. Ask your GP, specialist or Parkinsons nurse for a referral.
Addressing Practical Aspects Of Eating And Drinking
Some people with Parkinsons have problems chewing and swallowing. This can make it difficult to eat a diet with plenty of fibre. A speech and language therapist can give advice about this. Ask your GP, specialist or Parkinsons nurse for a referral. If it takes a long time to eat and your meal goes cold, eat smaller portions and go back for seconds that have been kept warm. You can also get special plates that keep your meals hot the Disabled Living Foundation has more information.
An occupational therapist will also be able to give you some tips and practical advice.
Read Also: Ear Acupuncture And Parkinson’s