Other Relevant Information Pages
| cookielawinfo-checkbox-analytics | 11 months | This cookie is set by GDPR Cookie Consent plugin. The cookie is used to store the user consent for the cookies in the category “Analytics”. |
| cookielawinfo-checkbox-functional | 11 months | The cookie is set by GDPR cookie consent to record the user consent for the cookies in the category “Functional”. |
| cookielawinfo-checkbox-necessary | 11 months | This cookie is set by GDPR Cookie Consent plugin. The cookies is used to store the user consent for the cookies in the category “Necessary”. |
| cookielawinfo-checkbox-others | 11 months | This cookie is set by GDPR Cookie Consent plugin. The cookie is used to store the user consent for the cookies in the category “Other. |
| cookielawinfo-checkbox-performance | 11 months | This cookie is set by GDPR Cookie Consent plugin. The cookie is used to store the user consent for the cookies in the category “Performance”. |
| viewed_cookie_policy | 11 months | The cookie is set by the GDPR Cookie Consent plugin and is used to store whether or not user has consented to the use of cookies. It does not store any personal data. |
Freezing Of Gait In Parkinson’s Disease
This short webpage explains what freezing of gait is, why it occurs, and treatment. It also offers 10 tips to prevent freezing or get ‘unstuck.’ Finally, there is a discussion of walkers that can prevent injury due to falls when freezing episodes are severe and the future of treatments for freezing of gait.
Definition Of Parkinsons Disease:
Parkinsons is a chronic progressive degenerative disorder affecting mainly people above the age of 60. Males are more prone than females. Worldwide prevalence is 0.3 1 %. If we talk about India alone, Parkinsons disease is the second leading chronic degenerative disorder after Alzheimers, with a prevalence that is directly proportional to age. Between the age of 70-79 years, it could be as high as 280 for a Hundred thousand people.
Parkinsons disease is a disorder that impacts the brain and leads to difficulty with balancing, coordination and walking. Along with this, the patient also experiences shaking and stiffness.
You May Like: How Does Parkinson’s Disease Develop
Coping With Freezing In Parkinson’s Disease
Claudia Chaves, MD, is board-certified in cerebrovascular disease and neurology with a subspecialty certification in vascular neurology.
Around half of people who have Parkinson’s disease experience freezinga temporary inability to move that occurs suddenly and without warning. Such episodes are short-lived, lasting from a few seconds to up to several minutes.
Parkinson’s freezing can affect nearly any part of the body and disrupt nearly any activitychewing for example, or writing. However, it most often occurs when someone is walking, causing them to feel as if their feet are glued to the ground even though the upper part of their body is still mobile. This sometimes is referred to as freezing of gait and can have repercussions ranging from a brief disruption in stride to an increased risk of falling that can lead to broken bones and other injuries.
The exact physiological cause of freezing in Parkinson’s has yet to be determined. What is known is that it’s often associated with lulls in the effectiveness of medication, particularly among people who have mid-to-late stage disease. There also are a number of common triggers of freezing while walking, such as changing direction, approaching a doorway, or navigating a crowded area. Although Parkinson’s freezing can have a negative impact on a person’s quality of life, there are simple and effective ways to manage it.
Parkinsons Disease Stem Cell Treatment
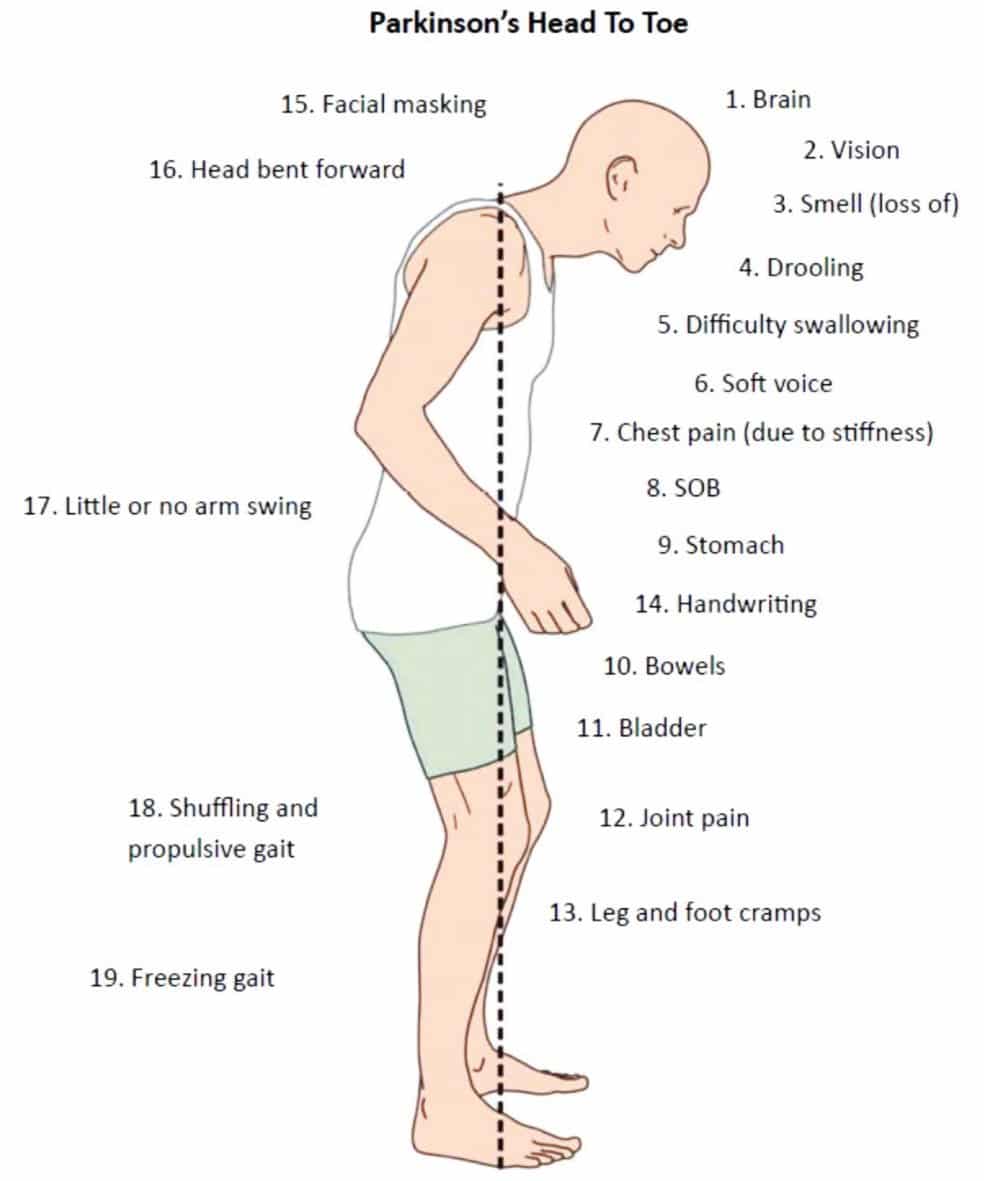
Parkinsons disease happens when there is a problem with certain nerve cells in the brain. This disease affects the way you move because of the inadequate production of dopamine, which is an important chemical that sends signals to the part of the brain that controls movement. Parkinsons is a progressive disease whose symptoms take a few years to surface.
Parkinsons is an illness that affects the central nervous system with a direct blow on the brain and spinal cord and usually only affects adults. More specifically, this disease damages a group of nerve cells in the deepest part of the brain called the Basal Ganglia. There are quite a few reasons leading to Parkinsons disease, including aging and poisons in the environment. To cure Parkinsons disease, stem cell treatment is highly popular.
These nerve cells make and use a brain chemical called dopamine to send messages to other parts of the brain to coordinate body movements. When someone suffers from Parkinsons disease, the dopamine levels are low. So, the body doesnt get the right messages required to move normally.
About 1 million people in the United States alone have Parkinsons, and both men and women can be affected by it. It usually affects the elderly population, someone older than 50, and it becomes common as people get older.
- Problems with balance or walking
Tremor, which essentially means shaking or trembling. Tremors may affect your hands, arms, or legs.
You May Like: Pharmacological Treatment Of Parkinson’s Disease
Techniques To Overcome Freezing
Physical therapy and occupational therapy can be helpful to reduce or overcome freezing episodes. Physical therapy focuses on the physical rehabilitation of people recovering from injuries or disease with the goal of restoring mobility, as well as educating patients on managing their condition to maintain long-term benefits. Occupational therapy also deals with rehabilitation and motion but is focused more on enabling the person to engage in daily activities as seamlessly as possible. Occupational therapists also suggest adaptations and modifications to the persons environment.3
There are several techniques that can help people with PD overcome freezing, including:
As with any symptom, patients who experience freezing episodes should mention this to their neurologist who is managing their care. The neurologist may make changes to medication or provide a referral to a physical or occupational therapist.
New Drug To Treat Parkinsons Disease To Be Introduced In India
Apomorphine, which is derived from the water lily plant, has been found to control several neurodegenerative symptoms of Parkinsons and aid in improvement of the condition in many cases.
The blue water lily was used by ancient Egyptians as a sedative and intoxicant. Centuries later, scientists have now discovered that a derivative of the plant has a significant role to play in the treatment of Parkinsons disease. Apomorphine, which comes from the plant, has been found to control several neurodegenerative symptoms of Parkinsons and aids in improvement of the condition in many cases. This drug is now set to be available for the first time in India to treat those suffering from Parkinsons disease.
Around 300 to 400 people for every 100,000 population are diagnosed with Parkinsons in India, states Dr Shivam Om Mittal, Parkinsons Specialist from Bengaluru. It is expected to more than double by the year 2030 and will be a major non-communicable degenerative disorder among the people in the country. Speaking to the media on Thursday at an event held at Vikram Hospital in the city, introducing the drug to the Indian market, he along with several other experts talked about the impact of introducing the drug in India.
What is Parkinsons disease?
It is not as though the drug is not without its drawbacks.
Apomorphine pens
Recommended Reading: How Long Will A Person Live With Parkinsons Disease
Don’t Miss: How Many Forms Of Parkinson’s Are There
How Can I Help Myself
Freezing in public places can be upsetting, embarrassing and even frightening. You may feel tempted to avoid situations that are more likely to make you freeze crowded rooms, narrow entrances etc but this may not always be practical. Social activities are important to quality of life and overall wellbeing so it is important to find out what strategies work best for you to prevent or overcome freezing. This will mean that you can continue to do things you enjoy.
The first thing to remember if you think you are about to freeze is to stop moving so that you have time to think about your balance. Stay calm and dont rush. You can then think about your next movement and plan how to carry it out before you actually move. Following these simple steps will allow you to put in place the strategies you have learned to overcome freezing and will reduce the risk of falling.
If you experience frequent freezing your doctor may suggest that you keep a medication or wearing off diary to help establish what might be causing these episodes. By keeping a diary, you can record the timing, duration and frequency of freezing episodes, as well as the timing and dosage of each medication, which can help your doctor in adjusting medication to try to overcome freezing problems. For a sample diary and information on keeping one, see Keeping a diary.
If you find that you freeze in busy places such as shops or public places you may find the following strategy helpful:
Balance And The Brain
Difficulties with balance and walking are linked to the brain changes that take place with PD. For people who dont have PD, balance is automatic, a reflex. But Parkinsons affects the basal ganglia . To compensate, the brain assigns another brain area an area used for thinking to take over. The thinking part of the brain, mainly the frontal cortex, cant control balance automatically. The result: for many people with PD, balance becomes less automatic.
This means that when people experience freezing and fall, they cant adjust their balance automatically. Taking small steps to try and regain balance can make things worse, because it involves shifting weight with each step. The brain changes from PD inhibit their ability to take a big step to catch their balance and avoid a fall. For some, the drug levodopa can help prevent freezing, but does not improve balance.
A person whose balance is less automatic must pay more attention while walking. For everyone, walking slows down when were talking and thinking slows down when were walking. This is called the dual-task cost and its higher in people with PD. That tells us that people with PD are using more attention and more cognitive control for balance and gait.
Don’t Miss: Treatment Of Parkinson’s Disease In Elderly
What Causes Freezing Of Gait In Parkinsons
There are significant differences between people with Parkinsons who experience freezing of gait and those who dont. However, there are some commonalities that may help to explain why some people with Parkinsons disease develop this symptom while others dont.
One theory is that freezing of gait occurs when certain brain areas are unable to properly process information from the body regarding movement. This can be due to damage to the parts of the brain that control movement, or it may be due to changes in the way that information is transmitted between the different parts of the brain.
Another theory is that freezing of gait may be a result of an imbalance in the neurotransmitters in the brain. Neurotransmitters are chemicals that help to transmit signals between the different parts of the brain. If there is an imbalance in the neurotransmitters, it can lead to problems with movement.
Yet, another theory involves the contribution that step length has to FOG.
Freezing of gait has been identified as one of the main contributors to gait disturbances in Parkinsons disease. While the pathophysiology remains enigmatic, several factors such as step length and the sequence effect may lead to the occurrence of FOG.
Understanding Phenomenology And Pathophysiology
Despite an abundance of clinical experience from direct observations, there are still a significant number of fundamental gaps in our understanding of FOG despite the proposal of several pathophysiological models . These range from the very basic grasp we have on phenomenology through to the more nuanced appreciation of its underlying neurobiology that manifests clinically.
Read Also: Drugs That Can Mimic Parkinsons Disease
You May Like: Gift Ideas For Parkinson Patients
Is Freezing Related To The Intake Of Dopaminergic Medication
Some people with Parkinsons have on and off periods, when they switch from being able to move when their medication level is higher to being unable to move without difficulty when their medication level is low . Many people notice that freezing is worse when their medication level is low, when they are off. But freezing is not the same as being on or off.
Noninvasive Vagus Nerve Stimulation
Recently, it has been reported that VNS administered for 10days improved locomotion in a rodent model of PD . Thus, an observational, open-label, pilot study explored the effect of single-dose, noninvasive VNS on gait pattern and FOG in 12 patients with FOG. A total of 2 VNS treatments were applied to the left vagus nerve in left side of the neck below the mandibular angle, medial to the sternocleidomastoid muscle and lateral to the larynx, with an interval of 15min between 2 VNS treatments. Each VNS treatment consisted of 120s of stimulation. Assessments were performed just before and 15min after the application of VNS. Video analysis showed that VNS significantly improved the number of steps taken while turning . The mechanism was still unknown. One possibility is that locus coeruleus noradrenergic neurons degenerate prior to substantia nigra dopaminergic neurons in PD, and VNS may activate locus coeruleus neurons . A multicenter, double-blind, placebo/sham-controlled randomized trial of noninvasive VNS in patients with PD are needed.
Recommended Reading: Early Symptoms Of Parkinsons Disease
Music Exercise Therapy Group
In addition to routine rehabilitation treatment, we will provide music exercise therapy, in which patients will perform scheduled exercises according to the rhythm of music. This will be performed 5 times a week for 4weeks, with 1h each time.
Music selection
Music therapists will screen musical tracks and rhythms according to the actual situation and music preferences of patients with Parkinsons disease. Thereafter, the therapists will create a personalized music playlist for each subject, because the lyrics in the music may distract attention of the PD patients, hence selection of music with lyrics will be avoided. Each playlist will be loaded into a personal music player, and subjects are allowed to choose earplugs or headphones for maximum comfort. The mode setting of the music player will be sequential play, and not random play. Moreover, music will be played by a designated music therapist, and subjects will be also told that they can request changes to their playlists at any stage during intervention.
Exercise therapy
While listening to music using earphones, the patients will be subjected to conduct flat start walking, turn around, and stop trainings, as well as narrow space walking and stair step training according to the beat in the music. The patients will be expected to simultaneously complete a cycle of exercise relative to completion of the music playlist.
Points for attention
How To Deal With Freezing
The management of this symptom is based on physical therapy with rehabilitation oriented towards gait disorders. The use of sensory cues can be used to support this management and to limit freezing of gait.
It is recommended to practice regular physical activity, and to favor activities involving the mobilization of motor and rhythmic abilities .
Here are some tips recommended by the American Parkinson Disease Association for returning to walking during a freezing episode :
-
Try to do another movement before moving on. For example, raise one arm, touch your head, point to the ceiling, then try to move again.
-
Change direction, or move to the side before moving again.
-
Visualize an object on the floor in front of you and try to walk on it.
-
Take a step backward and then forward.
-
Walk on the spot and then move forward.
-
Point with your arm in the desired direction and move forward, insisting on swinging your arms.
-
Tap the leg you want to move forward before starting the movement.
-
Count 1, 2, 3 and move forward.
-
Use a rhythmic sound to focus on the rhythm to restart and maintain a steady walk.
Technological solutions are being developed to offer rhythmic auditory stimulation at home. This technique can be useful to resume walking after a freezing and to limit its appearance in order to improve ones overall gait.
The WALK medical device is based on this technique and it is possible to try this innovation at home.
To learn more, visit our website
RESILIENT INNOVATION
Read Also: Immunotherapy For Parkinson’s Disease
Risk Factors For Developing Fog
This review included the prospective studies that followed early-stage PD patients over time and the retrospective studies that clearly recorded the clinical manifestation prior to FOG onset. Many studies identified FOG related motor and non-motor symptoms by utilizing cross-section data to compare the clinical symptoms between freezers and non-freezers. Those studies were excluded as they cannot differentiate the symptoms prior to FOG from the accompanying symptoms of FOG. A total of 11 longitudinal follow-up studies were reviewed and summarized . For these studies, cox proportional-hazards regression analyses or logistic regression analysis were performed to identify the factors predictive of FOG except one study that used generalized estimating equations . Here, we elaborated the risk factors including demographic information, motor symptoms, non-motor symptoms, neuroimaging, fluid parameters, and medication use. Current limitations and recommendations for future researches will also be discussed. A list of the evidence supporting and refuting the following variables as risk factors of FOG was provided in Table .
Table 1 A detail summary of risk factors for FOG development in Parkinsons disease
What Does It Look Like
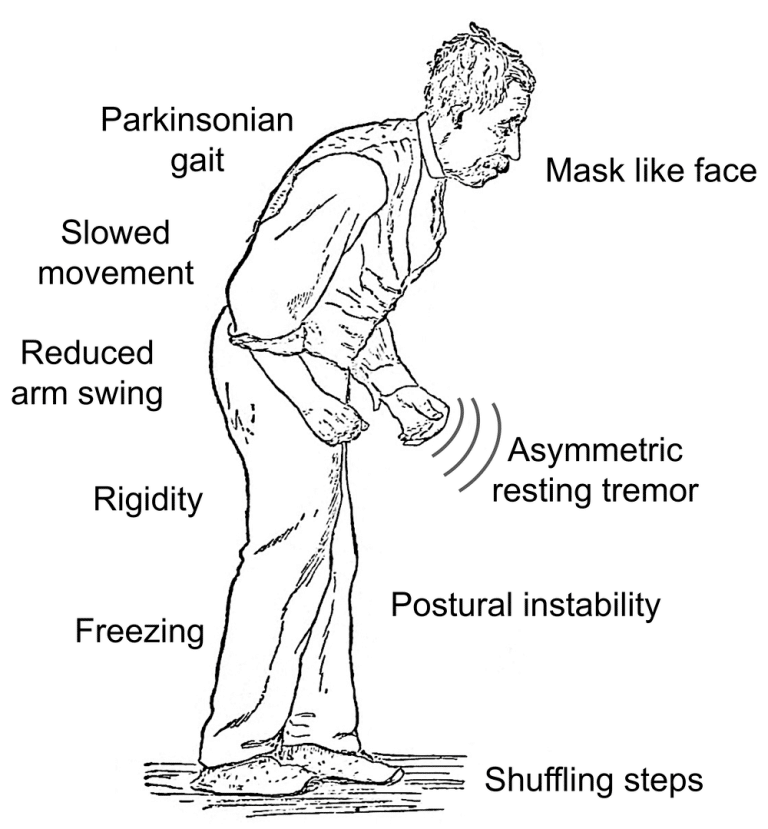
Parkinsonian gait is one of several motor symptoms that are the hallmarks of Parkinsons disease, including slowness of movement and tremors. Motor symptoms in Parkinsons disease come from a lack of control over movements and difficulty initiating muscle movements.
The exact features of Parkinsonian gait can differ from person to person, but there are some very common features that most people have. These include:
- taking small, shuffling steps
- moving more slowly than expected for your age
- festinating, or when your strides become quicker and shorter than normal, which can make it look like youre hurrying
- taking jerky steps
- moving your arms less when walking
- falling frequently
- freezing of gait
People with Parkinsons disease can sometimes lose the ability to pick up their feet, which makes them stuck in place. Freezing of gait can be triggered by environmental factors, such as walking through a narrow doorway, changing directions, or walking through a crowd. It can also be triggered by emotions, especially anxiety or feeling rushed.
Freezing of gait can happen anytime. However, it often occurs when you stand up. You might find that youre unable to pick up your feet and start moving.
Don’t Miss: How Long Does A Parkinson’s Patient Live