Dietary Considerations With Medications
Treatments are only effective in moderating the symptoms of the disease, mainly with drugs including levodopa and dopamine agonists. Once too many dopamine producing cells have been lost however, the effects of L-DOPA become less effective. Once this occurs, a complication known as dyskenesia commonly occurs in which subjects undergo involuntary writhing movements despite the use of L-DOPA. The effects of dyskenesia vary between periods of high symptoms and low symptoms. In order to limit the onset of dyskenesia, typical L-DOPA dosages are kept as low as possible while still achieving desired results. Lastly, in cases in which drugs are ineffective, deep brain stimulation and surgery can be used to reduce symptoms.
Levodopa is taken orally and is absorbed through the small intestines into the blood, competing for access with natural proteins. Additionally, once the drug has entered the blood stream, L-DOPA utilizes the same pathways to cross the blood brain barrier as natural protein. Only about 5 10% of levodopa crosses the blood brain barrier, while the remaining is metabolized elsewhere in the body. The metabolism of medications elsewhere is known to cause side effects such as nausea, dsykinesias, and stiffness.
Icipating In Clinical Trials
Clinical trials and their participants have revolutionized Parkinsons treatment, and have changed the lives dramatically of those affected. They have helped make available many new treatments in addition to improving the delivery methods of medications and new deep brain stimulation techniques.
Clinical trials are essential to the future of Parkinsons research, and APDA is committed to this vital effort.
What Causes Parkinsons Disease
Parkinsons disease occurs when nerve cells in an area of the brain called the substantia nigra become impaired or die. These cells normally produce dopamine, a chemical that helps the cells of the brain communicate . When these nerve cells become impaired or die, they produce less dopamine. Dopamine is especially important for the operation of another area of the brain called the basal ganglia. This area of the brain is responsible for organizing the brains commands for body movement. The loss of dopamine causes the movement symptoms seen in people with Parkinsons disease.
People with Parkinsons disease also lose another neurotransmitter called norepinephrine. This chemical is needed for proper functioning of the sympathetic nervous system. This system controls some of the bodys autonomic functions such as digestion, heart rate, blood pressure and breathing. Loss of norepinephrine causes some of the non-movement-related symptoms of Parkinsons disease.
Scientists arent sure what causes the neurons that produce these neurotransmitter chemicals to die.
Also Check: Does Parkinson’s Cause Swelling
Strategies For The Treatment Of Parkinsons Disease: Beyond Dopamine
- 1Laboratorio de Neurobiología, Facultad de Ciencias de la Salud, Universidad San Sebastián, Concepción, Chile
- 2Department of Biological Sciences, University of Limerick, Limerick, Ireland
- 3Health Research Institute, University of Limerick, Limerick, Ireland
- 4Department of Psychology and Neuroscience, Center for Neuroscience, University of Colorado, Boulder, CO, United States
- 5Research & Development Service, Bay Pines VA Healthcare System, Bay Pines, FL, United States
Parkinsons disease is the second-leading cause of dementia and is characterized by a progressive loss of dopaminergic neurons in the substantia nigra alongside the presence of intraneuronal -synuclein-positive inclusions. Therapies to date have been directed to the restoration of the dopaminergic system, and the prevention of dopaminergic neuronal cell death in the midbrain. This review discusses the physiological mechanisms involved in PD as well as new and prospective therapies for the disease. The current data suggest that prevention or early treatment of PD may be the most effective therapeutic strategy. New advances in the understanding of the underlying mechanisms of PD predict the development of more personalized and integral therapies in the years to come. Thus, the development of more reliable biomarkers at asymptomatic stages of the disease, and the use of genetic profiling of patients will surely permit a more effective treatment of PD.
Getting Medication On Time

Parkinson’s patients who do not get the correct medicine at the right time when they are in hospital, sometimes cannot talk or walk. The health of a majority deteriorated due to unsatisfactory medication management when they are in hospital. Parkinson’s UK believes the NHS could save up to £10m a year and improve the care of Parkinson’s patients if mandatory training is introduced for all hospital staff.
Parkinson UK found:
- “Nearly two thirds of people who have Parkinsons dont always get their medication on time in hospital.”
- “More than three quarters of people with Parkinsons that we asked reported that their health deteriorated as a result of poor medication management in hospital.”
- “Only 21% of respondents told us they got their medication on time without having to remind hospital staff.”
Recommended Reading: Can Head Injury Cause Parkinson’s
Full Financial Disclosures For The Last 12 Months
Alessandra Fanciulli: Dr. Fanciulli reports royalties from Springer Nature Publishing Group, speaker fees and honoraria from the Austrian Autonomic Society, Austrian Parkinson Society, Ordensklinikum Linz, International Parkinson Disease and Movement Disorders Society and Theravance Biopharma and research grants from the Stichting ParkinsonFond and the Österreichischer Austausch Dienst, outside of the submitted work.
Fabian Leys: Dr. Leys reports no disclosures.
Cristian Falup-Pecurariu: Dr. Falup-Pecurariu reports royalties from Springer Nature Publishing Group, speaker fees and honoraria from the International Parkinson and Movement Disorders Society, outside of the submitted work.
Roland Thijs: Dr. Thijs reports speaker fees from Novartis, consultancy fees from Theravance Biopharma and research support from the Dutch Epilepsy Foundation Dutch, the Netherlands Organization for Health Research and Development and De Christelijke Vereniging voor de Verpleging van Lijders aan Epilepsie, outside of the submitted work.
Gregor K. Wenning: Dr. Wenning reports consultancy fees from Biogen, Biohaven, Lundbeck, Minoryx, Takeda, Theravance and research support from the Austrian Science Fund, International Parkinson Disease and Movement Disorders Society and the Medical University Innsbruck, outside of the submitted work.
Adjuvant Therapy For More Advanced Parkinson’s Disease
- A choice of dopamine agonists, MAO-BIs or COMT inhibitors should be offered as an adjunct to levodopa for people with Parkinson’s disease who have developed dyskinesia or motor fluctuations despite optimal levodopa therapy.
- COMT inhibitors:
- Reversibly inhibit the peripheral breakdown of levodopa by the COMT enzyme, increasing the amount available for conversion to dopamine in the brain and reducing fluctuations in plasma levels.
- Produce clinical benefits in people with levodopa motor fluctuations and in those with stable responses to levodopa.
- Entacapone should ideally be offered as a combination drug because of poor patient compliance. One study found that early addition of entacapone to combined therapy produced more benefit than if it were introduced at a later stage . Tolcapone should only be used if entacapone fails .
Also Check: Foods To Help With Parkinson’s Disease
Advanced Therapies For Parkinson’s Disease
When significant off-time or dyskinesia persists despite optimised oral treatment, advanced therapies should be considered. Apomorphine, a potent dopamine agonist given by continuous subcutaneous infusion, is the least invasive and most straightforward of these. Following on from extensive clinical experience, the recent double-blind TOLEDO study confirmed a significant reduction in off-time and improved on-time with apomorphine versus placebo.
Deep-brain stimulation involves surgical placement of electrodes into brain regions such as the subthalamic nucleus to improve motor fluctuations or refractory tremor. DBS is typically considered in patients without significant axial or neuropsychiatric problems. It improves motor function, off-time and QoL in patients with PD, and provides significant benefits over medical therapy even in patients with an average disease duration of 7 years. The benefits of DBS on motor function, fluctuations and activities of daily living have been demonstrated up to 10 years postoperatively, although axial features continue to progress. Infusion of levodopacarbidopa intestinal gel via jejunostomy has also been shown to improve off-time compared to oral levodopa, and is commissioned in specialist centres where other advanced therapies are ineffective or contraindicated. Further information on the decision-making process for advanced therapies is summarised in a dedicated review.
Mitochondrial Dysfunction: A Pivotal Pathological Mechanism Of Parkinsons Disease
Mitochondria are complex cytosolic organelles of eukaryotic cells whose primary function is the generation of cellular energy in the form of ATP by oxidative phosphorylation. Mammalian mitochondria contain between 2 and 10 mitochondrial DNA molecules encoding 22 transfer RNAs, two ribosomal RNAs, and 13 polypeptides, each of which is part of the respiratory chain and the oxidative phosphorylation system . The mitochondrial respiratory chain contains four protein complexes that form the site of oxidative phosphorylation. This site is responsible for NADH and FADH2 oxidation, co-occurring with the movement of protons from the matrix into the intermembrane space. This movement produces an electrochemical gradient denoted as mitochondrial membrane potential . This gradient stimulates the ATP synthase to reduce molecular oxygen and synthesize ATP. This step is fundamental in aerobic metabolism and constitutes the primary provider of ATP at the final stage of cellular respiration . Nevertheless, the biological function of mitochondria goes far beyond energy production and includes the metabolism of lipids and amino acids and the support of intermediate metabolic pathways, such as the Krebs cycle.
Don’t Miss: What Are The Initial Symptoms Of Parkinson’s Disease
Treatment Of Dyskinesia And Dystonia
Troublesome peak-dose dyskinesia can be managed by reducing the dose of levodopa or adjunctive dopaminergic agents if possible. Dopamine agonists are less likely to cause dyskinesia, so in patients with brittle symptom control, adding or increasing the dopamine agonist may allow levodopa to be reduced. Amantadine, an NMDA antagonist, has been shown to reduce dyskinesia in some studies., However, its short-lasting efficacy and anticholinergic adverse effects, including delirium and hallucinations, limit its use in older people.
To manage dystonia, levodopa dosage and administration should be adjusted, as outlined for motor fluctuations. Anticholinergic agents such as benztropine and trihexyphenidyl may be useful, however, the risk of adverse effects such as delirium, hallucinations and falls in older people usually outweigh the benefits. In patients with cognitive impairment they should be avoided. Baclofen or botulinum toxin injections into dystonic muscles can occasionally help in intractable cases.
Anticholinergics For Early On
The first pharmacological agents used in PD therapy were anticholinergic drugs. They reduce the activity of acetylcholine by acting as antagonists at choline receptors, hoping to restore the balance between dopamine and acetylcholine levels that was disturbed by PD. These drugs have largely been replaced by L-DOPA and other centrally acting dopaminergic agonists, but they still remain available for use in the treatment of PD. Benztropine, biperiden, diphenhydramine, ethopropazine, orphenadrine, procyclidine, and trihexyphenidyl are included in this therapeutic class of drugs, though there is little pharmacokinetic information available on them because of their low plasma drug concentrations. Typically, anticholinergic drugs have a greater role in tremor-predominant PD and can be a monotherapy in early stages, but are usually done in adjunct with L-DOPA or other prescribed medications.
You May Like: Parkinson’s Disease Exercise Program
Medications For People With Parkinsons Disease
Symptoms of Parkinsons disease result from the progressive degeneration of nerve cells in the brain and other organs such as the gut, which produce a neurotransmitter called dopamine. This causes a deficiency in the availability of dopamine, which is necessary for smooth and controlled movements. Medication therapy focuses on maximising the availability of dopamine in the brain. Medication regimes are individually tailored to your specific need. Parkinsons medications fit into one of the following broad categories:
- levodopa dopamine replacement therapy
- dopamine agonists mimic the action of dopamine
- COMT inhibitors used along with levodopa. This medication blocks an enzyme known as COMT to prevent levodopa breaking down in the intestine, allowing more of it to reach the brain
- anticholinergics block the effect of another brain chemical to rebalance its levels with dopamine
- amantadine has anticholinergic properties and improves dopamine transmission
- MAO type B inhibitors prevent the metabolism of dopamine within the brain.
What Lifestyle Changes Can I Make To Ease Parkinsons Symptoms
Exercise: Exercise helps improve muscle strength, balance, coordination, flexibility, and tremor. It is also strongly believed to improve memory, thinking and reduce the risk of falls and decrease anxiety and depression. One study in persons with Parkinsons disease showed that 2.5 hours of exercise per week resulted in improved ability to move and a slower decline in quality of life compared to those who didnt exercise or didnt start until later in the course of their disease. Some exercises to consider include strengthening or resistance training, stretching exercises or aerobics . All types of exercise are helpful.
Eat a healthy, balanced diet: This is not only good for your general health but can ease some of the non-movement related symptoms of Parkinsons, such as constipation. Eating foods high in fiber in particular can relieve constipation. The Mediterranean diet is one example of a healthy diet.
Preventing falls and maintaining balance: Falls are a frequent complication of Parkinson’s. While you can do many things to reduce your risk of falling, the two most important are: 1) to work with your doctor to ensure that your treatments whether medicines or deep brain stimulation are optimal and 2) to consult with a physical therapist who can assess your walking and balance. The physical therapist is the expert when it comes to recommending assistive devices or exercise to improve safety and preventing falls.
You May Like: Parkinson’s Donations In Memory Of
Medication Guidelines For Parkinson’s Disease
There is no one best mix of Parkinsonâs medicines. You and your doctor will have to try a few treatment approaches to figure out the best one for you.
But there are some general guidelines for taking your medication. Be sure to ask your doctor or pharmacist for any specific tips for your treatment.
Diagnosis Of Parkinson’s Disease
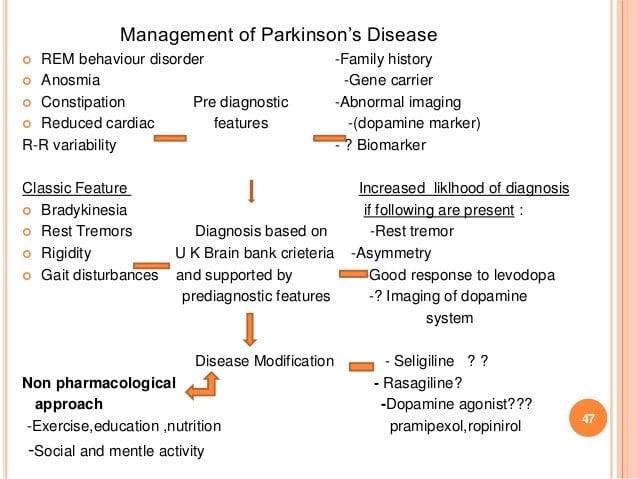
The diagnosis of PD is clinical and requires bradykinesia, defined as slowness of movement and decrement in amplitude or speed, usually assessed using finger tapping, foot tapping or pronationsupination hand movements. In addition, rest tremor or rigidity is required to confirm a parkinsonian syndrome. Tremor was absent at presentation in 30% in one series of pathologically proven PD. Patients with suspected PD should be referred quickly and untreated to a specialist in movement disorders for evaluation. Key points for discussion at diagnosis include the need to inform vehicle licensing agencies and insurers, signposting to written or web-based information on newly diagnosed PD, and provision of contact details for the local PD nurse specialist .
Current International Parkinson and Movement Disorder Society diagnostic criteria for Parkinson’s disease adapted from Postuma RB, Berg D, Stern M et al. MDS clinical diagnostic criteria for Parkinson’s disease. Mov Disord 2015 30:1591601. At least two supportive criteria and no red flags required for a diagnosis of clinically established Parkinson’s disease. Conditions in italics should be considered if the corresponding exclusion criteria or red flags are present.
You May Like: Does Parkinson’s Cause Weight Gain
Symptoms Of Parkinsons Disease
The type, number, severity and progression of Parkinsons disease symptoms vary greatly. Every person is affected differently they may not get every symptom.
Some of the more common symptoms are:
- resting tremor
- rigidity
- blood pressure fluctuation
- constipation.
People living with Parkinsons for some time may experience hallucinations , paranoia and delusions . These symptoms are able to be treated so have a talk with your doctor.
Associated Clinical Features Of Probable Pdd
Associated clinical features are defined along four primary cognitive domains and a spectrum of behavioural disorders . The MDS Task Force recommended a number of tests from which the clinician could choose to assess the four primary cognitive domains and suggested that the four-item Neuropsychiatric Inventory, which covers hallucinations, depression, delusions and apathy, might be useful in assessing behavioural symptoms associated with PDD . A diagnosis of probable PDD is made on the basis of a typical profile of cognitive deficits . If dementia exists in the presence of established PD, yet the associated clinical features are not considered typical , only possible PDD should be diagnosed.
Don’t Miss: Young Onset Parkinson’s Symptoms
Dietary Management Of Parkinson’s Disease
| Find sources: “Dietary management of Parkinson’s disease” news ·newspapers ·books ·scholar ·JSTOR |
Parkinson’s disease is the 2nd most prevalent neurological disorder within the United States and Europe, affecting around 1% of the population over the age of 60. While the link connecting the onset of Parkinson’s disease to environmental factors is known, the link between dietary patterns and the disease is just beginning to be researched more fully. Additionally, other research has sought to examine the symptoms of the disease and propose methods on how to alleviate these symptoms through changes in diet. Current medications that work to alleviate the symptoms of Parkinson’s disease can also be made more effective through changes in diet.
What Is Parkinsons Disease
Parkinsons disease is a nervous system disease that affects your ability to control movement. The disease usually starts out slowly and worsens over time. If you have Parkinsons disease, you may shake, have muscle stiffness, and have trouble walking and maintaining your balance and coordination. As the disease worsens, you may have trouble talking, sleeping, have mental and memory problems, experience behavioral changes and have other symptoms.
Recommended Reading: Parkinson’s And Bad Taste In Mouth
Progression Of Parkinson’s Disease
The disease progression of PD from diagnosis has been conceptualised into four stages . It is also important to recognise a prodromal phase in which non-motor symptoms, such as anosmia, constipation and rapid-eye-movement sleep behaviour disorder may predict the development of motor PD. Motor complications are more common as PD progresses, and typify transition to the complex phase. Many so-called axial symptoms of later stage PD, such as dysphagia, gait disturbance and falls, do not respond to levodopa, but may be helped by multidisciplinary team input. Dementia occurs in up to 80% of people with PD after 20 years disease duration. The rate of PD progression is heterogeneous and is generally more rapid in those with older age and more severe motor impairment at onset.
Stages of Parkinson’s disease. RBD = rapid eye movement sleep behaviour disorder.