Sleep Disturbances And Subtypes Of Pain
The frequency of sleep disturbances was 20% for patients without pain and 38% for patients with pain . In comparison with patients without pain, the frequency of sleep disturbances was significantly higher for patients with central parkinsonian pain , but not for musculoskeletal pain , dystonia-related pain , or radicular/neuropathic pain .
Among patients with pain, a simple logistic regression revealed that the odds of having sleep disturbances were higher among patients with central parkinsonian pain . No significant association was found with musculoskeletal pain, dystonia-related pain, or radicular/neuropathic pain . When adjusted for severity of motor symptoms in off , presence of motor fluctuations, pain intensity , anxiety, and depression , the odds of having sleep disturbances remained higher in patients with central parkinsonian pain .
|
Table 2 Odds of patients with pain having PDSS-2 total score 18 according to pain subtypes |
Beating The Lockdown Blues
Did you knowBodily functions are heavily influenced by biological clocks which are distributed throughout your body . Your clocks primary role is timing and orchestrating your bodys everyday vital functions and aligning these to geophysical and social schedules. Disruptions to your daily routine derail your clock which reflects negatively on your mood, energy, sleep, digestion, heart and immune system, just to name a few!
With COVID-19-related lockdowns causing unanticipated disruptions to our routine, Researchers at the University of Queensland have developed some guidelines to stay on a schedule to improve sleep and support your health and wellbeing.
Meds That Improve Some Symptoms Can Exacerbate Others
SAN ANTONIO — Roughly three out of four people living with Parkinson’s disease also have sleep disorders, and there is growing recognition that sleep problems are greatly complicated by the disease, its symptoms, and the many medications used to treat it.
“Sleep disorders are among the most common non-motor symptoms in PD, and sleep is something clinicians have to continually monitor when considering medication dosing,” Scott Kutscher, MD, of Stanford School of Medicine in California, told MedPage Today.
“Sleep issues can appear years before the classic motor symptoms of Parkinson’s, but it has only been relatively recently that sleep has become part of the diagnostic workup of the disorder,” he added.
Insomnia, excessive daytime sleepiness, sleep fragmentation, circadian rhythm disorders, restless leg syndrome, and rapid eye movement behavior disorder are all common in patients with Parkinson’s disease.
Although there is some debate about whether having PD increases the risk for obstructive sleep apnea , a recent review of the literature found an increased frequency of OSA and other sleep-disordered breathing conditions associated with the neurodegenerative disorder.
One mechanism suggested for this association is that upper airway musculature may be affected by involuntary movements characteristic of the disease, resulting in abnormal spirometry and upper airway obstruction.
Also Check: Huntington’s Disease Vs Parkinson’s Disease
Develop A Bedtime Routine
Your bedtime routine should help you prepare for bed. So be sure to follow it every evening. Essential tasks that every bedtime routine must have include:
- Having a Light Snack: Eat only light snacks if you get hungry before bed. Heavy meals before going to bed are unhealthy and can result in weight gain. Also, avoid snacks that might contain stimulant ingredients like alcohol and caffeine.
- Taking a Warm Bath: Bathing in warm water before bed may improve sleep quality. However, be sure not to spend too much time in the bath as it may wake up your body.
- Go to the Toilet: Be sure to finish your business in the bathroom before bed. Minimize your liquid intake at least three hours before bedtime to help avoid nocturia.
- Brush Your Teeth: Brushing your teeth right before bed helps prevent dental problems, including cavities and decay. Although it is indirectly related to better sleep, having this step in a bedtime routine is helpful.
Hallucinations And Rem Sleep Disorders In Parkinson’s Disease

At timestamp 1:58 in this recording of Thrive: HAPS 2020 Caregiver Conference, you will find a one hour talk by neurologist Joohi Jimenez-Shahed, MD. In it she delves into what REM sleep behavior disorder is and is not, and the distinctions between hallucinations, delusions, and delirium. Managment options for RBD and hallucinations are included.
Also Check: How To Calm Parkinson’s Tremors
Characteristics Of The Sample
Of the 229 PD patients examined, 122 were men, mean age was 69 years , mean age at disease onset was 60 years , and mean duration of the disease was 9 years . Ninety-six were taking dopamine agonist and the mean levodopa equivalent dose was 900 mg/day . The mean ropinirole dose was 10 . Mean scores in motor scales were: 32 in UPDRSS-III off and 22 in on 2.7 in H& Y off and 2.3 in on. One hundred and thirty-one had motor fluctuations. Mean in the functional independence scale S& E were 75 in off and 87 in on. At the time of the assessment, 162 patients reported pain. Of those with pain, 99 had musculoskeletal pain, 43 had dystonia-related pain, 38 had central parkinsonian pain, and 19 had radicular or neuropathic pain. No patient reported akathitic discomfort. The frequencies of HADS 8 on anxiety and depression subscales were, respectively, 102 and 111 . Mean SF-36 summary scores for physical and mental health were, respectively, 40 and 46 .
Sleep And Circadian Rhythm Disturbance Resulting From Pd
A study conducted on familial PD models indicated that dysfunction of the ER could also be a contributing factor to defects in sleep patterns and circadian rhythm . Further research has demonstrated that impaired neuropeptide distribution in specific neurons is responsible for disrupted circadian rhythm and sleep patterns in PD mutant Drosophila and has mapped these defects to specific neuronal clusters, including ventral lateral neurons and insulin-producing cells . The LNvs are analogous to neurons in the human hypothalamus , and secrete the vasoactive intestinal peptide -like neuropeptide pigment dispersing factor , which is involved in regulating the circadian cycle . Further investigations have revealed that the excessive ERmitochondrial contact involved in phosphatidylserine transport interfere with the production of PDF-loaded dense core vesicles via effects on lipid membrane composition, resulting in a defect in the release of PDF and subsequent sleep pattern defects in flies . Notably, supplementation with PtdSer was shown to rescue sleep defects in PD models, indicating that the disturbed sleep and circadian rhythmicity can be attributed to neuronal dysfunction rather than neurodegeneration, and may therefore be reversible.
Read Also: Classic Signs Of Parkinson’s Disease
Lessons From Other Fields: The Role Of Sleep Deprivation
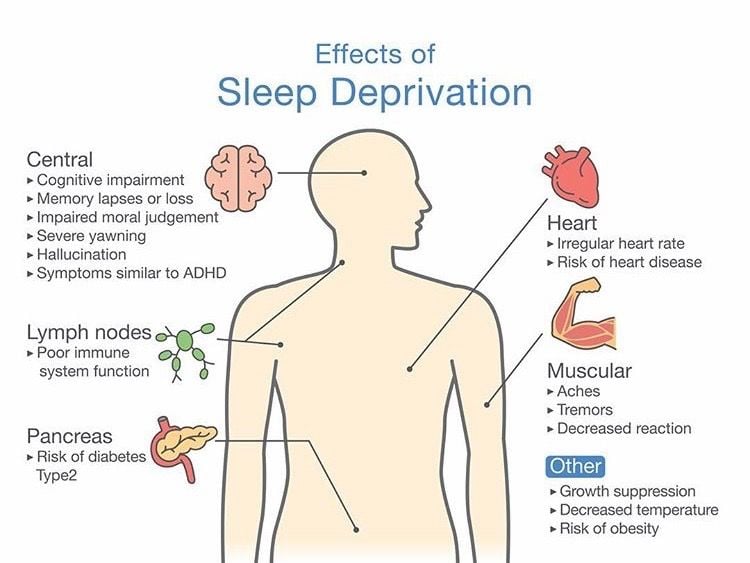
Mounting evidence points to short- or long-term sleep deprivation as a cause to structural and pathological changes in the brain. A number of animal studies document the sensitivity of the hippocampus to chronic sleep deprivation and an imaging study reported increased neuronal loss in the hippocampus of patients with chronic insomnia . In mice, sleep deprivation promotes astrocytic phagocytosis and microglial activation , likely leading to exacerbated phagocytosis of synaptic elements.
Several studies also show that sleep is the most important diurnal phase for clearance of neuronal metabolites such as A42 . In addition, the reduction of slow wave sleep increase the level of brain A prior to amyloid deposition, the hallmark of Alzheimer’s disease , which is also observed in patients with dementia with Lewy bodies and PD , indicating that interventions targeting sleep that reduce amyloid burden could be of significance in the prevention or treatment of both AD and -synucleinopathies.
Why Do Parkinsons Patients Have Trouble Sleeping
Despite having daytime tremors, Parkinsons patients do not shake in their sleep. However, both Parkinsons disease itself and the medications used to treat it can give rise to a number of sleep problems that lead to insomnia and excessive daytime sleepiness.
Patients with motor symptoms may have trouble adjusting sleeping positions to get comfortable. Others may experience distressing nocturnal hallucinations when trying to fall asleep. These may be a result of medications or cognitive impairment.
In turn, excessive daytime sleepiness may occur as a consequence of sleeping poorly at night. It may also be triggered by medications. Parkinsons patients who suffer from EDS may be at a higher risk of accidents and unable to safely carry out activities such as operating a motor vehicle.
Since insomnia frequently goes hand-in-hand with anxiety and depression, it may be a contributing factor to sleep problems in people with Parkinsons disease. For that reason, doctors often look for mental health disorders in people with Parkinsons disease who have sleep problems.
Also Check: Seizures Associated With Parkinson’s Disease
Tips For Better Sleep
- Keep a regular sleep schedule go to bed at the same time and get up at the same time.
- Choose your bedtime based on when you want to get up. Plan to spend seven to eight hours a night in bed.
- Make a bedtime routine for example, snack, bath, tooth-brushing, toileting and follow it every evening.
- Spend time outdoors and exercise every day, in the morning if possible. Avoid exercise after 8:00 p.m.
- If you cant get outdoors, consider light therapy sitting or working near a light therapy box, available at drug stores and department stores.
- If you nap, try to do so at the same time every day, for no more than an hour, and not after 3:00 p.m.
- Sleep in a cool dark place and use the bed only for sleeping and sexual activity.
- Do not read or watch television in bed.
- Use satin sheets and pajamas to make moving in bed easier.
- Minimize drinking liquids for three hours before bedtime to avoid frequent nighttime urination.
- Go to the bathroom immediately before retiring.
- Place a commode next to the bed, to minimize the effort, and light to get up during the night.
- Avoid:
- Alcohol, caffeine and other stimulants such as nicotine
- Heavy late-night meals
- Heavy exercise within six hours of bedtime
- Thoughts or discussions before bedtime about topics that cause anxiety, anger or frustration
- Clock watching
- Screen time television, phones, tablets one or two hours before bed.
Good Night: Sleep And Parkinsons Disease
Lack of good sleep can worsen Parkinsons symptoms. In this 45-minute lecture, Dr. Rafael Zuzuárregui addresses causes of sleep loss and the latest treatments for: insomnia, restless leg syndrome, REM sleep behavior disorder, nocturnal urination, hallucinations, wearing off of medication, dystonia and sleep apnea.
Recommended Reading: What Drugs Cause Parkinson Like Symptoms
Whats The Relationship Between Parkinsons And Sleep
Parkinsons disease and sleep are connected in complex ways that not even scientists completely understand quite yet.
Sometimes, Parkinsons disease directly causes sleep problems. According to one study, sleep-related symptoms may be one of the earliest signs of Parkinsons disease. These signs may include things like thrashing while youre asleep.
Other factors can also play a role. One thing is clear: For many people with Parkinsons disease, a restful nights sleep can be hard to find.
Nighttime Tips For Better Sleep

For more insights on this topic, listen to our podcast episodeParkinsons Disease and Sleep.
*Please note that not all content is available in both languages. If you are interested in receiving Spanish communications, we recommend selecting both” to stay best informed on the Foundation’s work and the latest in PD news.
Read Also: What Diseases Are Similar To Parkinson’s
What Didnt Work For Me But Might Work For Others
My Parkinsons Nurse first tried swapping out the sleeping drug that the doctor would no longer prescribe for pharmaceutical melatonin. This didnt work for me and made my insomnia even worse. However, I was anxious about it, because there are contra-indications for long term use in PD. Some theories of PD even assert that it is not just a shortage of dopamine which is the issue, but the resulting imbalance between dopamine and melatonin .
Whenever we look at other hormones and neurotransmitters in people with PD , the balances with dopamine are always off. It appears that it is more the relative levels between various biochemicals which are causal, rather than the absolute levels of any one individual chemical. The old-fashioned dopamine producing cell death narrative was naïve.
Indeed, a light therapy protocol developed by a clinic in Australia for PD, which has demonstrated real life long term symptom reduction , works by attacking melatonin when it is at its peak value, thus bringing balance back to dopamine and melatonin levels.
Furthermore, Dr Andrew Huberman also expresses qualms about melatonin as a long term solution, as it reduces levels of sex hormones.
Indeed, I discovered something interesting along the way. Taking the passion flower tincture reduced my pain and rigidity! I later found out that passion flower is a weak MAO inhibitor, and hence slows the break down of dopamine, works like the PD drug Rasagiline.
Sleep Disorders Related To Parkinsons Disease
Poor sleep quality can decrease a persons overall quality of life. For those diagnosed with Parkinsons disease , cognitive decline may contribute to sleep disturbances, which affect alertness in the morning and the ability to fall asleep.
Whether you or your loved one has PD and trouble sleeping, lets learn about the relationship between the two in this article.
Don’t Miss: Best Parkinson’s Doctors In Usa
How Does Parkinsons Disease Cause Sleep Problems
Researchers have yet to uncover every nuance of the Parkinsons and sleep connection. So far, medical experts believe several causes may contribute:
- Chemical changes in the brain: Ongoing research shows that Parkinsons disease may disrupt sleep-wake cycles. Changes to certain brain chemicals may cause people with Parkinsons to get less sleep.
- Medication: Some drugs that treat Parkinsons disease may make it harder to fall or stay asleep. A medication may also disrupt your sleep patterns by making you drowsy during the day .
- Mental health challenges: People with Parkinsons commonly deal with mood disorders, such as anxiety or depression. Any mood disorder may keep you up at night or make you sleep less soundly.
- Parkinsons symptoms: Pain, waking up at night to pee or other Parkinsons symptoms can make restful sleep harder to come by. Sleep apnea can also disrupt sleep.
Aging Sleep Pattern And Sleep Stages
General statements about sleep can only be made regarding sleep in the normal young adult without sleep complaints, living on a conventional sleep-wake cycle. This is because in elderly people, there is a profound increase in inter-individual sleep variability that precludes any generalizations other than those in young adults . Aging is accompanied by a reduction in sleep quality and quantity, with a progressive reduction in sleep slow wave activity from the age of thirty years. Increasing evidence suggests that slow wave activity reflects synaptic density or the strength of cortical synapses, and reduced SWS in the elderly is associated with grey matter medial prefrontal atrophy as well as an age-related decline in memory performance. With aging, time spent in bed reduces due to earlier wake-up times compared to younger adults. The circadian rhythm change with increasing age is characterized by a phase advance of around 1 hour, with earlier bed times and wake up times. Aging is also associated with a weakening of circadian regulation, with the elderly having reduced 24 hour melatonin secretion and circadian modulation of REM sleep.
During REM sleep in contrast, posture control is lost, autonomic activity is highly unstable with centrally driven surges in heart rate and blood pressure, breathing is irregular and thermoregulation is suspended. REM sleep is defined by rapid desynchronized, low amplitude EEG activity, muscle atonia and episodic bursts of rapid eye movements.
Read Also: Gifts For Parkinson’s Patients
Limit Lights In Your Room
Minimize your exposure to artificial lights when preparing for bed. Sleep in a cool, dark place. Avoid bright lights when sleeping. You could keep dim night lights if sleeping in complete darkness is uncomfortable.
Avoid watching television and using mobile devices before bed or lying in bed. These devices emit blue lights that could affect your sleeping habits.
Why Does Pd Lead To Sleep Problems
When it comes to sleep and Parkinsons disease, it can be complicated. Chemical changes in the brain from PD can disrupt sleep. However, sleep disruptions are usually complex and many factors come into play. For example, drugs that treat PD as well as other conditions could contribute to poor sleep. Lifestyle habits, pain, and muscle stiffness can all add to the problem.1,2
Don’t Miss: Parkinson’s Disease And Movement Disorders Center Of Boca Raton
Sleep Problems In Pd Patients
The overall mean total PDSS score was 102.8 , and 17% of the patients had a total PDSS score under 82. A more detailed examination of the PDSS sub-scales and proportion of patients scoring below 5 are shown in Table ). In total, 70% had a total score under 5 on one or more items of the PDSS. There were no significant differences in Hoehn and Yahr stage 12 vs 34 for any of the PDSS items.
Table 1 Sleep problems, by PDSS items, for 176 patients with Parkinsons disease
Drugs Used To Treat Parkinsons Disease
The common Parkinsons disease medication of carbidopa and levodopa can contribute to insomnia for some people, says Horvat. Thats because its replacing the dopamine that youve lost in Parkinsons disease, she says. Research has shown that dopamine receptors play a role in wakefulness.
Sometimes when people are first started on this medication, they will take a dose right before bed rather than closer to their dinner, says Horvat. Then theyre not able to get to sleep because the dopamine affects the reward center in the brain and gives people a high, she says.
Besides timing the medication further from bedtime, your doctor may suggest taking an extended-release capsule of carbidopa and levodopa, says Horvat. That has a lower peak dose effect, so the stimulation is milder, and it lasts a little longer. It can allow patients to have more of a baseline rather than a peak at night, which can cause the insomnia, she says.
If you suspect your medication is making sleep difficult, tell your doctor dont stop taking the medicine as prescribed, says Horvat. Sometimes we can time the medication in a different way or in some cases we do change the medication but this is not something to try to figure out on your own.
Don’t Miss: What Is Signs Of Parkinson’s Disease