Overview Of Therapeutic Drugs
Several studies have reported the therapeutic effects of antidementia and antipsychotic drugs on VH. There are two types of globally used antidementia drugs, cholinesterase inhibitors and NMDA receptor antagonists. We reviewed key previous studies on these drugs.
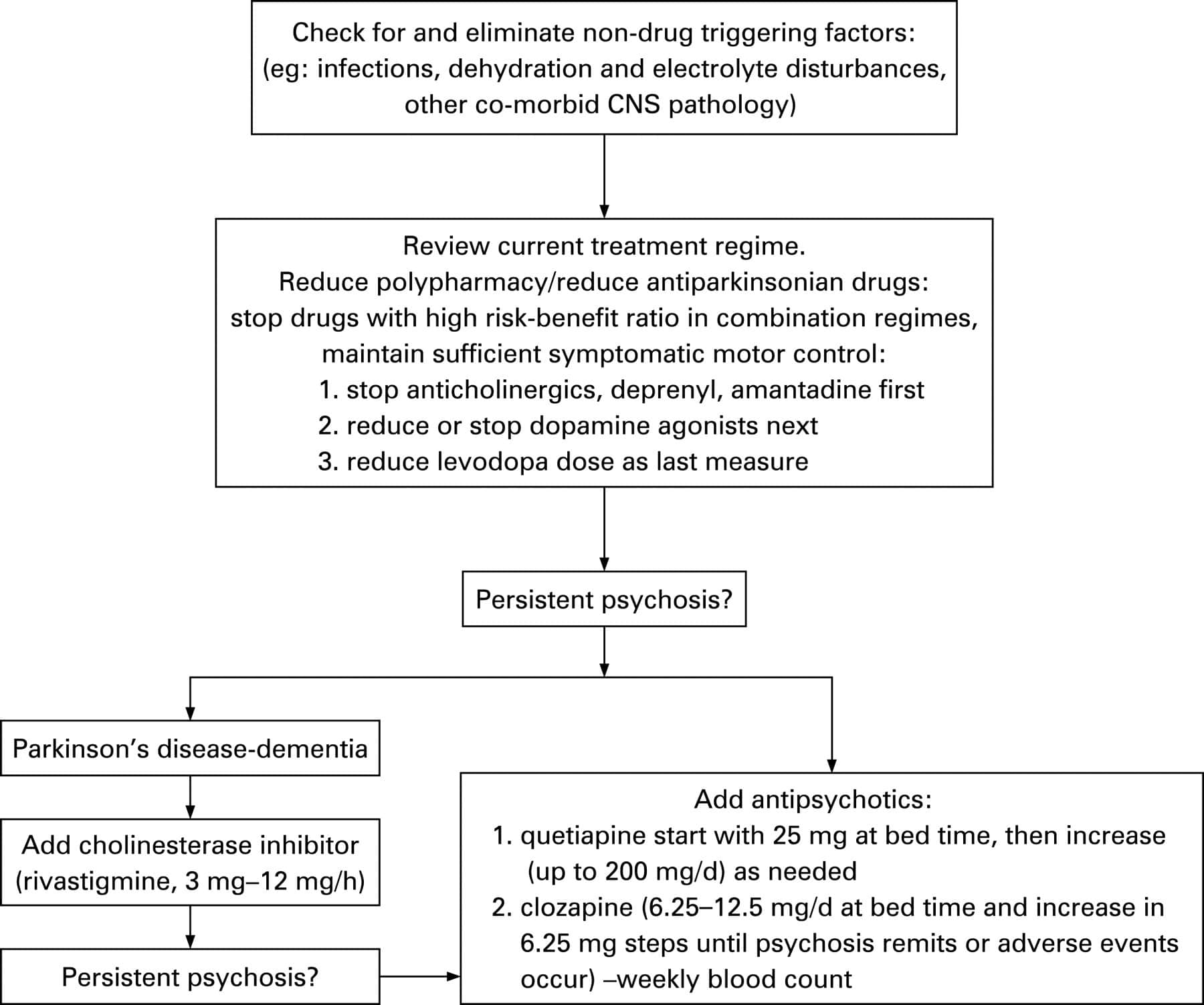
Cholinesterase inhibitors reduce VH and mostly do not worsen parkinsonism . They can be used as first-line drugs. Although there is no study showing that memantine ameliorates VH sufficiently, it may improve cognitive function . It can be used as an additional drug. Antipsychotic drugs should be used in a minimal dose due to high risks of mortality and adverse events . However, some of them reduce VH without causing intolerable adverse events . They should be used for cases that are difficult to control.
Hereafter, we will explain the studies on and detailed characteristics of these drugs and propose a treatment strategy.
How Hallucinations May Affect You
Hallucinations can be mild, or they can be quite frightening, especially when you dont realise that the things you see or hear arent real. Some people will be aware that they are hallucinating, and some wont be. Some people might prefer to tolerate a relatively harmless hallucination, rather than reduce their medication and possibly have an increase in their physical symptoms.
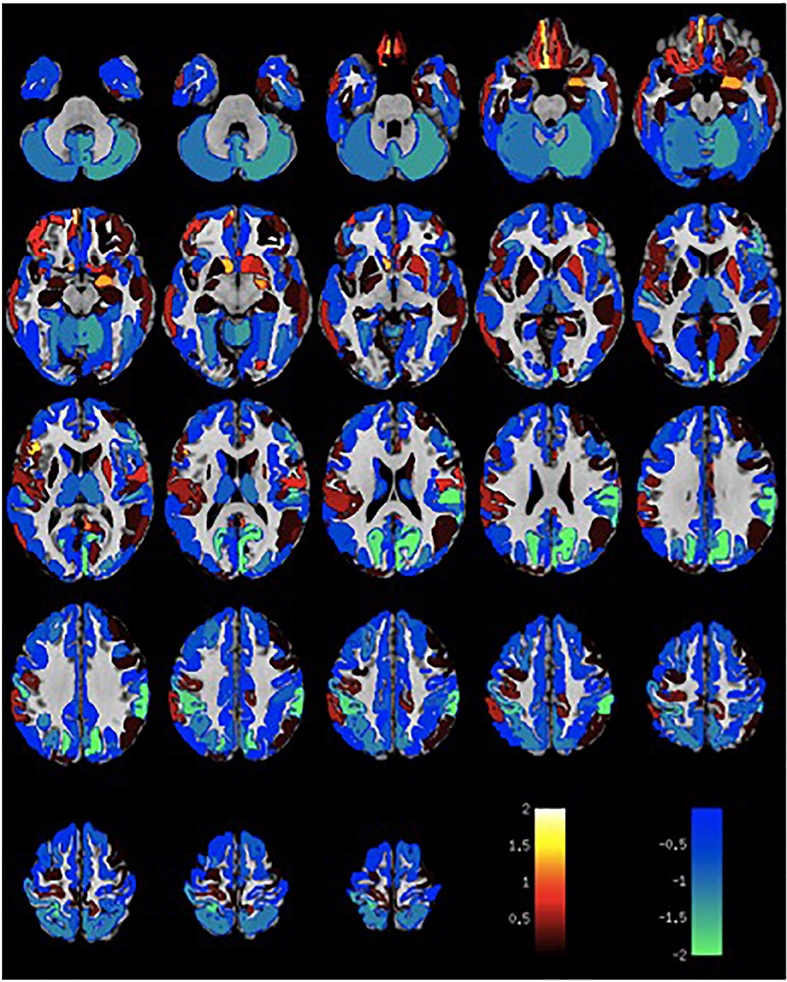
Visual Integrity And Visual Perceptual Scores
Cataracts were reported by 20% of the recruited participants while 19% of the participants had cataracts removed . Other ophthalmological history reported include glaucoma by two participants , macular degeneration by one participant , and laser treatment .
Visual acuity and perceptual scores are summarized in Table 1. There was a pattern of overall decline in visual integrity within the PDD patients relative to the control group, characterized by a significant reduction in LOGMAR measurements of visual acuity. As expected, PDD-CVH patients showed a characteristic significant increase in the number of false perceptions reported during the pareidolia task compared to PDD-NCVH patients. Interocular latency differences were significantly higher in PDD-CVH compared to the PDD-NCVH group.
Also Check: How Long Does It Take To Diagnose Parkinson’s
What Should I Do Once The Hallucination Passes
After the hallucination passes, you can try to talk through the experience together. If the person has insight, it may be easier for them to understand and talk about what just happened.
Write down what happened during the hallucination. Note the time of day and what the person was doing when it started.
Taking notes each time it happens can help you identify the triggers. It could be related to the timing of medication, and your loved one might feel a sense of relief and control in knowing that pattern.
Ask what you can do to stop it from happening again. This might include adjusting their medication dosage or adding an atypical antipsychotic drug to their medication regimen.
What Is Parkinsons Disease Psychosis
Parkinsons disease psychosis is a non-motor symptom of Parkinsons disease that causes patients to experience hallucinations and/or delusions.More than half of all patients with Parkinsons disease eventually develop symptoms over the course of their disease.1
Diagnosing and treating this condition can be complex. The condition relates to both neurology and psychiatry . For this reason, Parkinsons disease psychosis is considered a neuropsychiatric condition, since it deals with mental health symptoms caused by a disease of the nervous system .
Introducing an easier way to track your symptoms and manage your care.
Dont want to download the app? Use the non-mobile version here.
Recommended Reading: Parkinsons Double Vision
You May Like: Can Parkinson’s Disease Be Treated
Dr Zoe Says Walking Can Reduce Risk Of Dementia
We use your sign-up to provide content in ways you’ve consented to and to improve our understanding of you. This may include adverts from us and 3rd parties based on our understanding. You can unsubscribe at any time. More info
Dementia is a syndrome related to the continuous decline of the brain. For this reason it is often associated with memory loss and difficulties with language. Currently more than 850,000 people in the UK are living with dementia, with this expected to rise due to an ageing population.
Phenomenology Of The Hallucinations
Minor hallucinations/illusions
We grouped together in this category three types of phenomena. The most frequent type was presence hallucinations . The patient had the vivid sensation of the presence of somebody either somewhere in the room or, less often, behind him or her. In all cases, the presence was that of a person, and in one case it was also occasionally the presence of an animal . In seven cases, the presence was that of a relative . In all the other cases the presence was unidentified. The presence hallucinations were commonly as vivid as a hallucinated scene and were described as a `perception. For instance, one patient said: `the image is behind me, a second said: `I see someone arriving I turn back but nobody is there, a third said: `I take a look I dont see anything, but it is engraved in my mind, and another said: `I have the impression that my mother is always there, that she is about to come into sight. The passage hallucinations consisted of brief visions of a person or an animal passing sideways. If an animal was seen, the species was almost invariably specified , and in two instances it was a dog previously owned by the patient. Illusions occurred in nine patients . In five cases the illusion consisted of the transformation of an object into an animal .
Case 1 .
Case 4
You May Like: Herbal Tea For Parkinson’s
Treatment Of Parkinsons Disease Psychosis
Andrew Schleisman, PharmD Candidate 2017
Mikayla Spangler, PharmD, BCPSAssociate Professor of Pharmacy Practice
Emily Knezevich, PharmD, BCPS, CDEAssociate Professor of Pharmacy PracticeCreighton University School of Pharmacy and Health ProfessionsOmaha, Nebraska
US Pharm. 2016 41:HS20-HS26.
ABSTRACT: Delusions and hallucinations in patients with Parkinsons disease, a condition known as Parkinsons disease psychosis , have historically been treated with clozapine and quetiapine because of their relatively low likelihood of worsening motor symptoms. Although clozapine is considered the drug of choice, it is underused in this population because of the need for frequent monitoring. Quetiapine, on the other hand, is generally first-line treatment despite its questionable efficacy. Consequently, in 2006, the American Academy of Neurology identified a need for the development of a novel antipsychotic with evidence of both safety and efficacy in patients with PDP. Pimavanserin, which has shown promise in clinical trials, recently became the first agent to receive FDA approval for the treatment of PDP.
Some Examples Of Delusions And Their Impact In Pd Include:
- Belief: Your partner is being unfaithful.
- Behavior: Paranoia, agitation, suspiciousness, aggression
Read Also: Challenges Of Living With Parkinson’s Disease
Age And Duration Of Illness
Increased age has been associated with the presence of hallucinations. This might be explained by accerelated sensory loss or age related side effects of medication. One of the main confounders with age is duration of illness when the non-independence of these variables was controlled, Fénelon et alfound that duration of illness was the crucial factor. Grahamet al identified two subgroups of patients with Parkinsons disease experiencing hallucinosis: in those with disease duration of 5 years or less, visual hallucinations were associated with rapid progression of the motor but not the cognitive component of the disease. In the remainder with longer histories, visual hallucinations were associated with postural instability, global cognitive impairment, and the lack of depression. Goetz et al contrasted patients with Parkinsons disease who experienced hallucinations within 3 months of levodopa therapy with those who experienced hallucinations after 1 year of treatment. Diagnoses in the early onset group more often changed to Lewy body or Alzheimers disease. Lewy bodies are present to a greater or lesser degree in all cases of Parkinsons disease and are known to be associated with visual hallucinations.
How Can Caregivers Support Their Loved Ones
Caring for someone who sees, hears, or believes things that arent real can be very difficult. Try to be as patient and calm as you can.
Avoid arguing with the person. If they still have insight, gently explain that what theyre seeing isnt real. Tell anyone who cares for or visits your loved one what to expect, and how to respond.
Stay in close contact with the persons doctor. If their symptoms dont improve, ask whether they need a medication adjustment.
Check whether the person needs hearing aids or glasses. Poor hearing or vision can sometimes lead to hallucinations. It can also help to turn on bright lights at night, to prevent the shadows that may trigger visual illusions.
Secure any dangerous objects, and keep pathways in the home clear to prevent falls and injuries. If you ever feel like the person is a risk to themselves or others, call their doctor.
Read Also: Restless Leg Syndrome And Parkinson’s Disease
How Common Is Parkinsons Disease Psychosis
Between 20-40% of people with Parkinsons report the experience of hallucinations or delusions. When followed as the disease progresses over the years, this number increases. The increase does not mean that the hallucinations are persistent across the majority of patients. However, it is important to note that these statistics sometimes include delirium, in which the symptoms are temporary due to medication that needs to be adjusted or infection that needs to be treated, and isolated minor symptoms or minor hallucinations, including illusions, where instead of seeing things that are not there , people misinterpret things that are really there. These are the most common types of psychosis in people with PD, with different studies placing the occurrence between 25-70% of people with Parkinsons. Typically, if the person with PD only has these minor hallucinations, their doctor will not prescribe an antipsychotic medication, though more significant psychosis that requires medication may develop over time. In one study, 10% of those with minor hallucinations had their symptoms resolved within a few years, while 52% saw their symptoms remain the same and 38% saw their psychosis symptoms get worse.
We recommend that people with Parkinsons not use a single percentage to represent the prevalence of hallucinations and PDP. Parkinsons is a complex disease and as it progresses the percentages and risk of symptoms will change.
Also Check: Pfnca Wellness Programs
Examples Of Delusions In Pd
- Belief: Your partner is being unfaithful.
- Behavior: Paranoia, agitation, suspiciousness, aggression.
You May Like: On-off Phenomenon
Read Also: Parkinson’s Disease Fact Sheet
Data Collection And Outcome Measures
Information on patient age, sex, onset age and duration of PD, and medications was collected by neurologists caring for the patients. We asked the patients and their caregivers to use the original screening questionnaire for the presence of hallucinations, the timing of the hallucinations , the type of hallucinations , and the content of the hallucinations. After obtaining answers to the questionnaire, we conducted semistructured interviews with the patients and their caregivers, and the collected information included examples of hallucinations. Hallucinations were defined as feelings or perceptions without existence or physical stimuli that could involve any sensory modality .
Minor-type hallucinations included visual illusion and presence sense. Based on previous studies, visual illusions were defined as brief misperceptions of objects that differ from objective reality, and presence hallucinations were defined as vivid sensations that someone was present nearby in the absence of sensory clues .
For comparison, we performed the same screening questionnaire and interviewed healthy adults without neuropsychiatric manifestations and sleep disorders. Among healthy individuals, the term hallucination was also used for their abnormal perceptions without actual physical stimuli, based on the guidelines of previous publications .
Pdps Impact On Caregivers
As Susans story demonstrates, PDP is difficult for both the patient and their caregivers, particularly because it is impossible to convince someone that their delusions are not real. Logic does not penetrate. In fact, accusations of spousal infidelity are often the last straw when caregivers find caring for their loved one too overwhelming. One of the major problems in dealing with PDP is that the patient and the family often try to hide the problem the patient for fear of being thought crazy and the caregiver due to embarrassment. The reality is that when a Parkinsons Disease patient has psychotic symptoms, his or her mental abilities will be otherwise normal. The patient may not be disoriented, can still balance their checkbook and recall everything theyre supposed to know. When hallucinations or delusions occur, the treating doctor should be notified. No irreversible harm will occur if treatment is delayed, but it is unlikely the problem will go away on its own.
You May Like: Parkinson’s Disease And Nausea
Mickan Against Parkinsons Gala Dinner 2019
At The Mickan against Parkinsons Adelaide, SA. Congratulations to Ms.Nassaris and the team at Adelaide Oval for putting this together .Thanks for inviting Mr Girish Nair as a speaker for the event to speak about his involvement in Mr. Mickans care as a treating Neurosurgeon
Thanks for having Neuroaxis at this event celebrating a true Champion in footy and in the fight against Parkinsons. We are proud to be part of Marks Parkinson journey.
Recommended Reading: Parkinsons Hallucinations Commercial
Showing Up As Your Best Self
Caring for someone with a progressive condition like Parkinsons disease can be challenging. Hallucinations only add to the stress of caregiving, especially if the person youre caring for doesnt have insight into what theyre experiencing.
The more you understand about your loved ones condition, the easier itll be to care for them. Talk to their doctor and read up on Parkinsons disease so youre better equipped to respond when hallucinations occur.
Dont forget to take care of yourself as well. Take regular breaks from caregiving to relax and do the things you enjoy. By tending to your own needs, youll have more energy to devote to your loved one.
Also Check: Voice Amplifiers For Parkinson’s Patients
Whats The Treatment For Parkinsons Disease Psychosis
The single most important thing to do when it comes to Parkinsons disease psychosis is to tell your care providers and partners the minute you notice changes in your vision, hearing, thinking and behavior. The earlier they know whats going on, the sooner they can begin interventions to help you feel better.
Once you bring your concerns up to your doctor, they will typically do a clinical evaluation, review your medications and dosage, assess your lifestyle and determine the severity of your symptoms. Depending upon what they find, they may refer you to counseling or therapy, adjust your medication, change your medication, eliminate medication or do all of the above. If none of those strategies work, they may try antipsychotic drug therapy to see if they can adjust chemical levels in the brain. This can bring with it an entirely different set of problems so its important to be invested every step along the way and be sure youre well-informed before you move in that direction.
Dont Miss: Judy Woodruff Parkinsons
Practical Tips For Caregivers Of People With Parkinson’s Psychosis
This 2-page tip sheet has bullet point suggestions for what to do if the person you care for experiences hallucination, delusions or confusion, or becomes agitated or aggressive. In addition, there are tips for how to best be prepared for a doctors appointment when you bring this behavior to the attention of your medical team.
Also Check: Tea For Parkinson’s Disease
Hallucinations In Parkinsons Disease: Approach And Management
Babak Tousi, MD, and Thayagaran Subramanian, MD
Risk Factors
Risk factors that have been reported include dementia, duration of therapy with dopaminergic medications, duration of disease, age of patients,10,11 anticholinergic medications, and sleep disorders.12-15 The mnemonic SADDAD can be used to recall these risk factors for hallucinations in PD:
Sleep disorders Anticholinergic medications Duration of disease
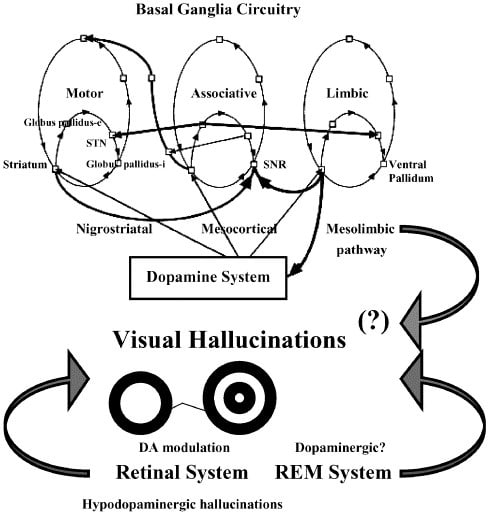
Severe cognitive impairment or dementia is a major and independent predictive factor for visual hallucinations.4,9,16 In one study, the prevalence of visual hallucinations was reported as 70% in patients with PD who have dementia.9 It is not clear whether cognitive impairment and hallucinations occur independently as the natural progression of disease or if they have causative links. Studies using positron emission tomography have shown marked occipital hypometabolism in patients with PD who have dementia.17 This suggests that degenerative process in the visual cortex can be a cause for visual hallucinations.
Auditory and Tactile Hallucinations
Treatment
Summary
AcknowledgmentThe authors acknowledge the help of Dr. Robert Palmer, Chief of Geriatric Section, Cleveland Clinic Foundation, in the preparation of this paper.
Treatment And Management Of Hallucinations
You should discuss any hallucinations or delusions with your doctor, or Parkinsons nurse if you have one, so that all treatment options can be considered.
In mild cases no specific action may be required and simple reassurance that the images, sensations or sounds are harmless may be all that is needed.
Read Also: Sam Waterston Tremor
Also Check: How To Pray For Someone With Parkinson’s
Support Your Loved One And Yourself
PDP is also associated with increased caregiver stress and burden, nursing home placement and increased morbidity and mortality. But, your loved one is certainly not alone in living with PDP, and an effective management plan can improve the complications. Seek out the support that he or she needs, but also make sure that you are getting the emotional care you personally need in order to be an effective advocate for your loved one.
Sensorimotor Hallucinations In Parkinsons Disease
- For correspondence:
You May Like: World Parkinson’s Day 2022 Theme