Parkinsons Is A Condition Which Produces Three Major Symptoms:
- Tremor
- Rigidity
- Akinesia
In addition, because of postural instability, poor balance can be a feature. These symptoms are also associated with disturbance of gait , particularly as Parkinsons progresses.
The symptoms may occur alone or in combination. They usually start on one side of the body and after a period of several years will then involve the other side of the body.
Behavioral And Clinical Data
Each patients overall motor impairment was indexed using the total score of the Unified Parkinsons Disease Rating Scale part III, where higher scores indicate more severe overall motor symptoms. While some previous studies have examined motor subtypes by classifying patients into AR or tremor-dominant groups, we chose to examine individual differences in these two domains of motor symptoms. Each individuals AR score was calculated as a sum of UPDRS III ratings on rigidity, finger tapping, hand movements, arising from chair, posture, gait, and body bradykinesia, and the tremor scores as a sum of ratings on resting tremor of the arms and legs and action tremor of the arms . To determine if motor impairments became more severe over time we evaluated motor domain scores in 274 patients who had behavioral data collected at all four time points. Baseline demographic information regarding these participants can be found in Table .
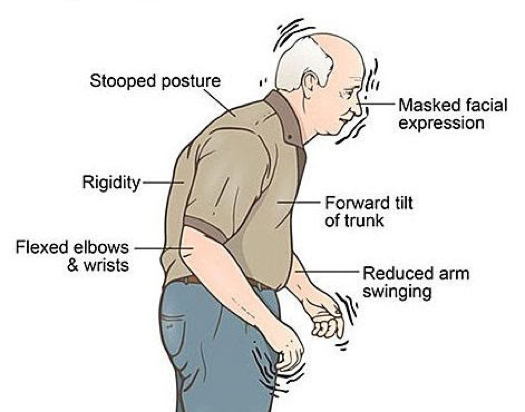
Muscle Rigidity: Lead Pipe And Cogwheel Rigidity
Muscle rigidity due to Parkinsonâs disease can be misdiagnosed as arthritis or general tightness from aging. Rigidity can affect your legs, arms, torso, and face. â
What rigidity feels like. Your muscles may feel tight and difficult to move. They may also stiffen involuntarily like a muscle spasm. This stiffness can also cause joint and muscle pain.
Rigidity and everyday life. This type of stiffness can start impacting your normal functions. Simple tasks like cleaning, exercise, and fulfilling hobbies can become difficult because of rigidity. You may also experience:
- Stiffness in your facial muscles that make it difficult to express yourself
- Stiffness while sleeping that make it difficult to get comfortable and sleep well
- Constant tension in your muscles that leads to muscle fatigue and a lack of energy
- Difficulty with certain motor skills, like writing or getting dressed
- Stiffness in your arms that make it harder to maintain balance while walking
Lead pipe rigidity. This type of stiffness is characterized by a feeling of frozen muscles. The muscles feel stuck and unable to move. â
Attempts to move those limbs are met with resistance throughout the motion. They feel stiff and heavy like a âlead pipeâ for sustained periods of time.
Cogwheel rigidity. This type of rigidity is similar to muscle spasms. The limbs experiencing the stiffness can move in small jerking motions, like a ratchet. You may even feel small clicking sensations when moving your arm. â
Recommended Reading: Parkinson’s Coughing At Night
Description Of The Included Studies
3.2.1. Methods Evaluating the Mechanical or Neurophysiological Properties of the Muscle
Eleven studies were included, which are summarized in . Of these, five used electromyography , three used myotonometry , and three used elastography . The study design chosen in all cases was casecontrol, except for the study by Hayashi et al., who used a prepost design. The sample size was quite low for all the studies . Five out of 11 studies did not reach 20 participants, whilst only 3 of 11 papers had a sample size 30 participants.
What Are The Non
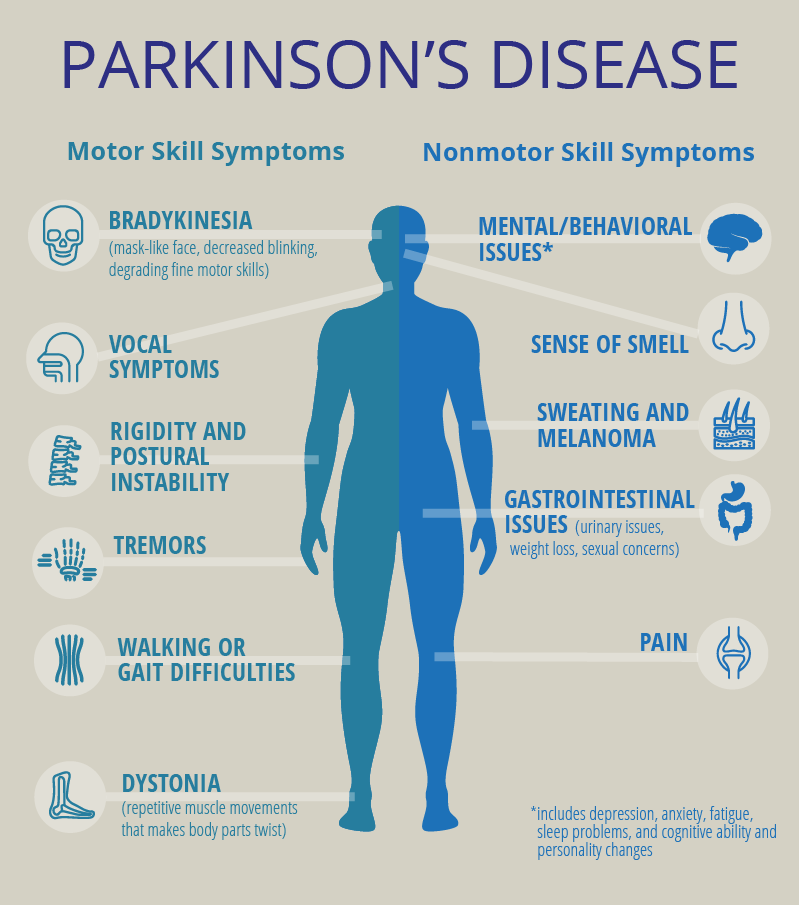
While Parkinson’s disease is often associated with movement changes, there are a variety of non-motor symptoms, as well. Non-motor symptoms refer to the many other changes to a person’s health and wellbeing that can happen from Parkinson’s.
These symptoms can sometimes have an even greater impact on a person’s life than tremor, rigidity, and slow movement, so it’s important to keep an eye out for them in someone with the disorder. Here are some of the non-motor symptoms of Parkinson’s disease to look out for:
Read Also: Can A Blood Test Detect Parkinson’s
How Is Parkinson’s Disease Diagnosed
A person doesn’t need to have all the signs and symptoms of Parkinson’s disease to be diagnosed with it.
“In general, people have a combination of the motor symptoms and the non-motor symptoms,” says Dr. Nwabuobi. “Some people have more non-motor symptoms than motor and vice versa, but in order to have a diagnosis of Parkinson’s, you definitely need the motor symptoms. We’re looking for specific things , including a rest tremor, bradykinesia, rigidity, and poor balance.”
According to the Parkinson’s Foundation, a person needs to have two of the four main motor symptoms of Parkinson’s over a period of time to be diagnosed with the disease.
Examining Muscle Weakness And Rigidity In Parkinsons Disease
The sun peeks over the horizon, and before long Dad is up and at it. Its a boxing day, and he wants to time his medications to optimize control over his Parkinsons symptoms.
The other part of his routine revolves around his morning stretches. Muscle rigidity is the first obstacle that he faces when he wakes, and he chooses to confront it with a stretching practice.
Parkinsons disease claims multiple functions as it progresses. Understanding how the disease affects the patient may help to inform treatment decisions. Im a curious person, and Dads stretching routine makes me wonder if Parkinsons disease directly affects the way muscles work. I think about how muscle rigidity and weakness are linked and how others handle these symptoms.
Recommended Reading: Parkinson’s Donations In Memory Of
Thanks For Signing Up
We are proud to have you as a part of our community. To ensure you receive the latest Parkinsons news, research updates and more, please check your email for a message from us. If you do not see our email, it may be in your spam folder. Just mark as not spam and you should receive our emails as expected.
Functional Imaging Studies Of The Effect Of Surgery And Deep Brain Stimulation On Bradykinesia
Many imaging studies have been driven by the model of basal ganglia function outlined in the early 1990s. Overactivity of the inhibitory output projections from the basal ganglia to the thalamus in Parkinson’s disease was supposed to remove facilitatory thalamocortical drive, particularly to midline cortical motor areas . PET and fMRI activation studies had shown that these areas were less activated during movement in patients, and therefore pallidotomy was expected to improve activation by restoring normal levels of basal ganglia output .
Most studies on movement-related changes in metabolic activity have reported similar findings both after pallidotomy and during subthalamic nucleus stimulation . In tasks in which a free-choice joystick movement is used, increased activation of preSMA and anterior cingulate cortex is usually accompanied by increased activation of the dorsolateral prefrontal cortex. Although most reports of activation-induced metabolism suggest that there is no change in the primary motor cortex, there are some suggestions that stimulation of the subthalamic nucleus may reduce activity in the resting state . Whether this is related to a general reduction in rigidity or other involuntary muscle activity or to reduced input to the cortex via pathways direct from the subthalamic nucleus is not known.
Recommended Reading: Leg Weakness Parkinson’s Disease
How Can I Help Myself
Try to keep active in spite of rigidity as this will help you maintain flexibility, mobility and independence. Regular exercise can also help to strengthen muscles and alleviate the pain and aches that often accompany rigidity.
The following suggestions may help:
- Continue your normal routine and daily activities as long as you are able.
- Follow a simple exercise programme to keep your muscles flexible and strong.
- Adjust your routine so that you do things that might tire your muscles when you feel least stiff .
- Remove or firmly secure loose rugs that you can trip over, and rearrange furniture to make it easier to move around at home.
- Maintain a positive attitude this can help with all sorts of difficulties.
Many people have discovered and developed activities and exercises that help with rigidity and mobility their own personal coping strategies. Although these wont work for everyone, watching some of the video clips on Coping Strategies – Tips & Tricks may help you discover and develop strategies of your own, for example juggling to avoid stiffness.
- Bouncing a ball to reduce stiffness – watch our video
- Juggling to reduce stiffness – watch our video
Muscle Weakness And Rigidity
As his Parkinsons progresses, Dad complains that his stiffness is slowing him down. The frequency and intensity with which it occurs seem to be increasing. To better understand the disease and how it relates to the body, I decided to explore the research.
In an abstract of a literature review published by the American Journal of Physical Medicine & Rehabilitation, the authors stated that isokinetic muscle strength was decreased in patients with Parkinsons disease and that muscle weakness was not specifically related to tremor or rigidity.
Recommended Reading: What’s The Difference Between Parkinson’s And Ms
Treatment And Management Options
There are several treatment options available to alleviate the motor symptoms associated with Parkinsons disease. Most of them also help Parkinsons patients overcome issues related to rigidity. These include:
- Medications such as levodopa , dopamine agonists, anticholinergics, catechol-O-methyl transferase inhibitors, and monoamine oxidase-B inhibitors. One treatment or a combination of treatments is commonly prescribed to Parkinsons disease patients to improve motor problems, including rigidity, that occur due to dysfunction in dopaminergic neurons.
- Physiotherapy to improve mobility and the range of movement in muscles and joints, and to alleviate the muscle cramps common in Parkinsons disease patients. An occupational therapist or physiotherapist can advise on daily routines, exercises, and the use of assistive devices, such as walkers or canes, to help the patient stay as mobile and independent as possible. Occupational therapy is generally needed for patients to perform daily activities more effectively, such as rolling in bed or getting up from a chair, for example. Regular exercise and stretching can strengthen muscles and maintain flexibility.
- Speech therapy that teaches facial exercises to help with speech and communication.
- Deep brain stimulation for Parkinsons disease patients whose symptoms are not adequately controlled with medications and/or exercise.
Pathophysiology Of Rigidity And Akinesia In Parkinsons Disease
Log in to MyKarger to check if you already have access to this content.
Buy a Karger Article Bundle and profit from a discount!
If you would like to redeem your KAB credit, please log in.
Save over 20%
- Rent for 48h to view
- Buy Cloud Access for unlimited viewing via different devices
- Synchronizing in the ReadCube Cloud
- Printing and saving restrictions apply
USD 8.50
- Access to all articles of the subscribed year guaranteed for 5 years
- Unlimited re-access via Subscriber Login or MyKarger
- Unrestricted printing, no saving restrictions for personal use
The final prices may differ from the prices shown due to specifics of VAT rules.
Don’t Miss: How Can You Test For Parkinson’s Disease
How Is Parkinsons Disease Treated
There is no cure for Parkinsons disease. However, medications and other treatments can help relieve some of your symptoms. Exercise can help your Parkinsons symptoms significantly. In addition, physical therapy, occupational therapy and speech-language therapy can help with walking and balance problems, eating and swallowing challenges and speech problems. Surgery is an option for some patients.
Managing Depression In Parkinsons Disease
People with Parkinsons, family members and caregivers may not always recognize the signs of depression and anxiety. If you are experiencing depression as a symptom of Parkinsons, it is important to know it can be treated.
Here are some suggestions:
- For information and support on living well with Parkinsons disease, contact our Information and Referral line.
- As much as possible, remain socially engaged and physically active. Resist the urge to isolate yourself.
- You may want to consult a psychologist and there are medications that help relieve depression in people with Parkinsons, including nortriptyline and citalopram .
Read Also: Tai Chi For Parkinson’s
Correlation Of Clinical Rigidity Scores And Damping Ratio
The damping ratios of PD subjects had a linear relationship with clinical rigidity scores .3). No other model parameters significantly correlated with rigidity, including natural frequency and peak time.
There is a linear relationship between clinical rigidity scores and damping ratio . This relationship could be utilized to predict rigidity scores, which significantly correlate with actual recorded rigidity scores.
Functional Image Data Preprocessing
Standard image preprocessing was performed using Statistical Parametric Mapping . For each individual, functional images were corrected for slice timing and then realigned to the first image to correct for head motion between scans, while structural image was coregistered to the mean functional image. The structural image was then segmented and normalized to a template based on a sample of individuals with PD using affine registration followed by nonlinear transformation,. The resulting parameters were then applied to all functional images. Finally, the functional images were spatially smoothed with a Gaussian kernel of 6mm at full width at half maximum.
You May Like: Parkinson’s Disease And Driving
How Is Cogwheeling Treated
You can help treat cogwheel rigidity by treating the underlying condition. The most common and effective treatment for Parkinsons disease is levodopa . It can help all symptoms, not just cogwheel rigidity. Its often combined with carbidopa, which helps lessen side effects.
Dopamine agonists and MAO-B inhibitors are other medications that treat Parkinsons disease.
If no other medication has worked, some people with advanced Parkinsons disease are candidates for deep brain stimulation. In this procedure, electrodes are positioned in the basal ganglia, where they send small electrical signals into the brain. This can help lessen cogwheel rigidity.
There are also things you can do at home to help manage your cogwheel rigidity. These include:
- Bouncing a ball like dribbling a basketball to keep your arms moving.
- Exercising. This can help strengthen your muscles and relieve pain. Aerobic exercise where you do large movements is best for reducing rigidity. Just be sure not to push yourself beyond your physical limitations.
- Stretching, to keep your muscles flexible.
- Practicing tai chi or yoga.
- Reducing stress. While stress doesnt cause Parkinsons disease, it can make your symptoms worse.
When you do any type of exercise, make sure you cool down properly. This helps keep your muscles from getting stiff again. A physical therapist can help you find the best exercise and stretching routine for you.
What Lifestyle Changes Can I Make To Ease Parkinsons Symptoms
Exercise: Exercise helps improve muscle strength, balance, coordination, flexibility, and tremor. It is also strongly believed to improve memory, thinking and reduce the risk of falls and decrease anxiety and depression. One study in persons with Parkinsons disease showed that 2.5 hours of exercise per week resulted in improved ability to move and a slower decline in quality of life compared to those who didnt exercise or didnt start until later in the course of their disease. Some exercises to consider include strengthening or resistance training, stretching exercises or aerobics . All types of exercise are helpful.
Eat a healthy, balanced diet: This is not only good for your general health but can ease some of the non-movement related symptoms of Parkinsons, such as constipation. Eating foods high in fiber in particular can relieve constipation. The Mediterranean diet is one example of a healthy diet.
Preventing falls and maintaining balance: Falls are a frequent complication of Parkinson’s. While you can do many things to reduce your risk of falling, the two most important are: 1) to work with your doctor to ensure that your treatments whether medicines or deep brain stimulation are optimal and 2) to consult with a physical therapist who can assess your walking and balance. The physical therapist is the expert when it comes to recommending assistive devices or exercise to improve safety and preventing falls.
Read Also: Is Parkinson’s A Form Of Cancer
What Causes Rigidity In Parkinsons Disease
The exact cause of rigidity in people suffering from Parkinson is not precisely known. It is believed that the reduction in dopamine , also called as a neurotransmitter relays the message to some areas of the brain for producing smooth and purposeful movement. These some areas of the brain are put together in a circuit called basal ganglia. When Parkinson damages these dopamine producing neurons, the communication between them is disrupted and rigidity is caused.
Is Parkinsons Disease Inherited
Scientists have discovered gene mutations that are associated with Parkinsons disease.
There is some belief that some cases of early-onset Parkinsons disease disease starting before age 50 may be inherited. Scientists identified a gene mutation in people with Parkinsons disease whose brains contain Lewy bodies, which are clumps of the protein alpha-synuclein. Scientists are trying to understand the function of this protein and its relationship to genetic mutations that are sometimes seen in Parkinsons disease and in people with a type of dementia called Lewy body dementia.
Several other gene mutations have been found to play a role in Parkinsons disease. Mutations in these genes cause abnormal cell functioning, which affects the nerve cells ability to release dopamine and causes nerve cell death. Researchers are still trying to discover what causes these genes to mutate in order to understand how gene mutations influence the development of Parkinsons disease.
Scientists think that about 10% to 15% of persons with Parkinsons disease may have a genetic mutation that predisposes them to development of the disease. There are also environmental factors involved that are not fully understood.
Also Check: Does Parkinson’s Cause Swelling
Pathophysiology Of Motor Dysfunction In Parkinsons Disease As The Rationale For Drug Treatment And Rehabilitation
Stefano Tamburin
1Department of Neurosciences, Biomedicine and Movement Sciences, University of Verona, Piazzale Scuro 10, 37134 Verona, Italy
2Neuromotor and Cognitive Rehabilitation Research Centre, University of Verona, Piazzale Scuro 10, 37134 Verona, Italy
3Rehabilitation Unit, Pederzoli Hospital, Via Monte Baldo 24, 37019 Peschiera del Garda, Italy
4Neurology Unit, Pederzoli Hospital, Via Monte Baldo 24, 37019 Peschiera del Garda, Italy
Abstract
1. Introduction
Parkinsons disease is the second most common neurodegenerative disorder after Alzheimers disease , with an overall prevalence of 300 per 100,000 that rises from 41 in the 4049 years age range to 1903 in people older than age of 80 years .
This review will summarize the evidence on the pathophysiology of PD motor symptoms and signs and give some insight into their neuropathological and neuropharmacological bases. These pieces of information may help the clinicians to better understand the rationale of current pharmacological and rehabilitation strategies for PD and encompass the large areas of uncertainty that should represent the focus for further studies.
2. The Functional Anatomy and Pathophysiology of the Basal Ganglia and the Role of the Cerebellum
3. The Neuropathology of PD
4. The Neuropharmacology of PD
| Neurotransmitter |
5. Pathophysiology of Bradykinesia in PD
6. Pathophysiology of Tremor in PD
7. Pathophysiology of Rigidity in PD
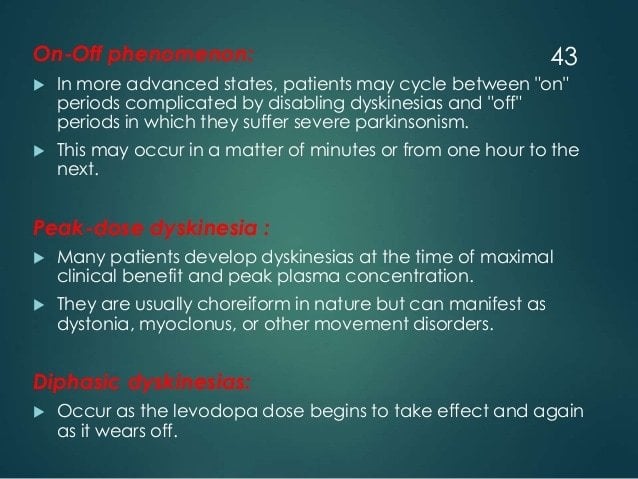
8. Pathophysiology of Motor Fluctuations and Dyskinesia