When To See A Doctor
You should see a doctor about Parkinsons symptoms when you first notice symptoms, says Dr. Maurer. While these symptoms may initially be discussed with a primary care provider, its important to be seen by a neurologist to receive a thorough neurological examination and a diagnosis.
Sometimes, a loved one may be the first to notice early symptoms of Parkinsons, such as changes in facial expressions, gait or handwriting. If you suspect a loved one is developing any symptoms associated with Parkinsons disease, make an appointment with a neurologist for proper testing and diagnosis.
Find Care For The Ones You Love
Conveniently search for local senior caregivers and senior living communities on Care.com.
Stage Four Of Parkinsons Disease
In stage four, PD has progressed to a severely disabling disease. Patients with stage four PD may be able to walk and stand unassisted, but they are noticeably incapacitated. Many use a walker to help them.
At this stage, the patient is unable to live an independent life and needs assistance with some activities of daily living. The necessity for help with daily living defines this stage. If the patient is still able to live alone, it is still defined as stage three.
Recommended Reading: Parkinsons Disease Stages Dementia
What Challenges Can People With Parkinsons Experience Later In Life
As Parkinsons disease is a progressive condition with variable motor and non-motor symptoms, patients may face considerable problems in late stages. Impairment of functions that are difficult to manage may bring limitations in daily activities and increase dependence.
The problems in later stages of Parkinsons disease include worsening walking disorders, with postural impairment and falls speech and swallowing disorders and progressive functional disability in the hands. They can also include non-motor issues, which may have a negative impact on quality of life including fatigue and sleep problems with restless legs or REM sleep disorder, bladder problems and constipation, drooling and orthostatic episodes, mood and behavioural disorders, hallucinations and cognitive impairment.
Recommended Reading: Sole Support For Parkinson’s
Signs Of Dying In The Elderly With Dementia
Dementia is a general term for a chronic or persistent decline in mental processes including memory loss, impaired reasoning, and personality changes. Alzheimers disease is the most common form of dementia, accounting for 60-80% of all cases of dementia. It is also the 6th leading cause of death in the United States, and over 5 million Americans are currently living with Alzheimers disease.
Alzheimers disease and most progressive dementias do not have a cure. While the disease inevitably worsens over time, that timeline can vary greatly from one patient to the next.
Caring for a loved one can be challenging and stressful, as the individuals personality changes and cognitive function declines. They may even stop recognizing their nearest and dearest friends and relatives. As dementia progresses, the individual will require more and more care. As a family caregiver, its important to be able to recognize the signs of dying in elderly with dementia. Hospice can help by offering care wherever the individual resides, providing physical, emotional and spiritual care to the patient and support their family.
How Is Parkinsons Disease Diagnosed
Its important to see a doctor about Parkinsons symptoms when you first notice them.Non-genetic cases of Parkinsons cant be diagnosed through blood or laboratory tests. Instead, a neurologist specializing in movement disorders can make the diagnosis by performing a neurological examination.
While symptoms may initially be discussed with a primary care provider, its important to be seen by a neurologist to receive a thorough neurological examination and a diagnosis, says Dr. Maurer.People with Parkinsons disease benefit from seeing a neurologist with specialty training in movement disorders, she adds. Movement disorders neurologists have completed extra training in Parkinsons disease, and typically a large fraction of their practice revolves around seeing patients with Parkinsons disease.
You May Like: Claiming Pip For Parkinsons Disease
Recommended Reading: Can Head Injury Cause Parkinson’s
A Guide To Understanding End
Crossroads Hospice & Palliative Care created guidelines to help family caregivers better understand the physical changes of the end-of-life process, as well as the emotional and spiritual end-of-life changes taking place.
The following describes the physical symptoms you may observe. Here are end-of-life signs and helpful tips:
What Are The Risks Of Not Receiving Any Dopaminergic Medication
There is the possibility of neuroleptic malignant-like syndrome , a life-threatening and distressing condition resulting in rigidity and fever, from withdrawal of therapy.31 This can also occur with sudden cessation of Deep Brain Stimulation .32,33,34 To reduce the risk of this, dopaminergic therapy at the end of life should be continued.27 It should also be noted that in a patient dying of another condition, whose PD is still responsive to dopaminergic medication, the cessation of this also risks aspiration pneumonia.35 Transdermal rotigotine can be used in patients in whom a NG tube may cause excessive distress or is not possible. The dose should be calculated with an accepted converter.36
You May Like: My Mom Has Parkinson’s Will I Get It
How To Get Palliative Care
If you or a loved one is facing Parkinsons disease, ask your doctor for a referral to palliative carethe earlier the better.
Although living with Parkinsons disease is difficult, your burden may be easier when palliative care is involved. You can receive palliative care in the hospital, at an outpatient clinic and sometimes at home.
Be informed about your condition, its treatment and what you can expect. And if you have received a Parkinsons diagnosis, or if the burden of illness is growing, dont hesitate to ask for a palliative care referral to help you make sense of the situation. With the support of palliative care, you can help ensure that you achieve and sustain the highest quality of life possible.
For more information, visit GetPalliativeCare.org. Take our quiz to find out if palliative care is right for you. And find providers in your area by visiting our Palliative Care Provider Directory.
Stage : Mild Dementia
At this stage, individuals may start to become socially withdrawn and show changes in personality and mood. Denial of symptoms as a defense mechanism is commonly seen in stage 4. Behaviors to look for include:
- Difficulty remembering things about ones personal history
- Difficulty recognizing faces and people
In stage 4 dementia, individuals have no trouble recognizing familiar faces or traveling to familiar locations. However, patients in this stage will often avoid challenging situations in order to hide symptoms or prevent stress or anxiety.
You May Like: Is Thumb Twitching A Sign Of Parkinsons
You May Like: What Benefits Am I Entitled To If I Have Parkinson’s
Parkinsons Progression Palliative And End Of Life Issues
This 38-minute webinar provides an overview of Parkinsons symptoms, and treatment challenges due to disease progression. 18-minutes in the topic turns to planning a good death, the euphemisms even doctors use to avoid discussing death, the most common cause of death in those with PD, putting your end-of-life preferences in writing. Palliative care can help families face these end-of-life issues.
What Is The Definition Of Palliative Care
The word palliative derives from the Latin pallium, meaning cloak or covering. It is reflected in the Middle Eastern blessing: May you be wrapped in tenderness, you my brother, as if in a cloak.
We could use the word cloak to symbolise the holistic care we aim for, which encompasses the physical, psychological, social and spiritual aspects of care, and is highlighted in the following definition of palliative care:
Palliative care is an approach that improves the quality of life of patients and their families who are facing problems associated with life-threatening illness. It prevents and relieves suffering through the early identification, correct assessment and treatment of pain and other problems, whether physical, psychosocial or spiritual.
The early development of the palliative care ethos was synonymous with cancer care, but as research in palliative care developed it became recognised that people living with life limiting, non-malignant illness had as many complex care needs as those suffering with cancer. The recognised definition of palliative care devised by the World Health Organization was therefore revised to incorporate the care of those with life limiting illnesses.
Further reading
The trajectory of Parkinsons is variable and complex, making it essential that each person is assessed regularly by the multidisciplinary team and their changing needs are managed on an individual basis.
2.2.1 Dynamic model of palliative care services
Read Also: Parkinson’s And Massage Therapy
Early Signs Of Parkinsons Disease Dementia
In the beginning, PDD can be subtle. Early on, there may be memory loss and difficulties with daily activities, says Michael S. Okun, M.D., executive director of the Norman Fixel Institute for Neurological Diseases at University of Florida Health in Gainesville. Delusions or hallucinations may also start to happen. Dr. Petrossian points out that there can be an overlap between the early signs of dementia and mild cognitive impairment due to Parkinsons disease, which can make it difficult to learn new skills and recall information or conversations.
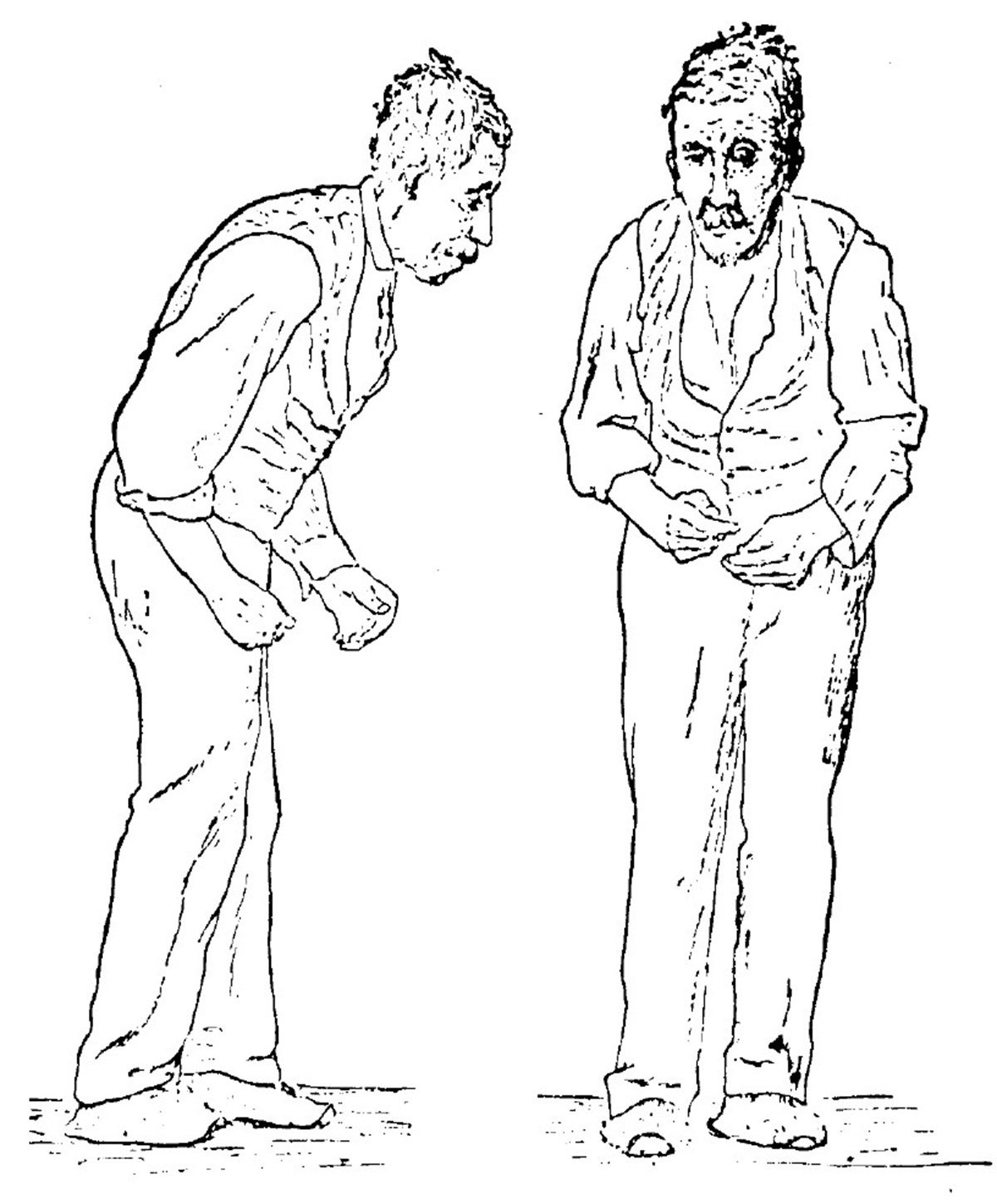
Stage One Of Parkinsons Disease
In stage one, the earliest stage, the symptoms of PD are mild and only seen on one side of the body , and there is usually minimal or no functional impairment.
The symptoms of PD at stage one may be so mild that the person doesnt seek medical attention or the physician is unable to make a diagnosis. Symptoms at stage one may include tremor, such as intermittent tremor of one hand, rigidity, or one hand or leg may feel more clumsy than another, or one side of the face may be affected, impacting the expression.
This stage is very difficult to diagnose and a physician may wait to see if the symptoms get worse over time before making a formal diagnosis.
Also Check: Does Weed Help With Parkinson’s
Hospice Care For Patients With End Stage Parkinsons Disease
The goal of hospice services is to provide a quality, peaceful death while allowing the person with Parkinson Disease to remain in a familiar environment such as their home, assisted living or long-term care facility. Hospice provides ongoing education related to caring for a loved at home. It can be overwhelming to care for a loved one that is no longer able to do the things that they normally were able to do in the earlier stages of the disease. Unfortunately, in the later stages of PD patients eventually lose the ability to care for themselves and require assistance with most activities of daily living. Some families struggle seeing their loved ones deteriorate and often feel helpless as PD symptoms are irreversible. Unfortunately, there is no cure for PD but certain medications have been approved to help with symptoms and slow down the progression of the disease.
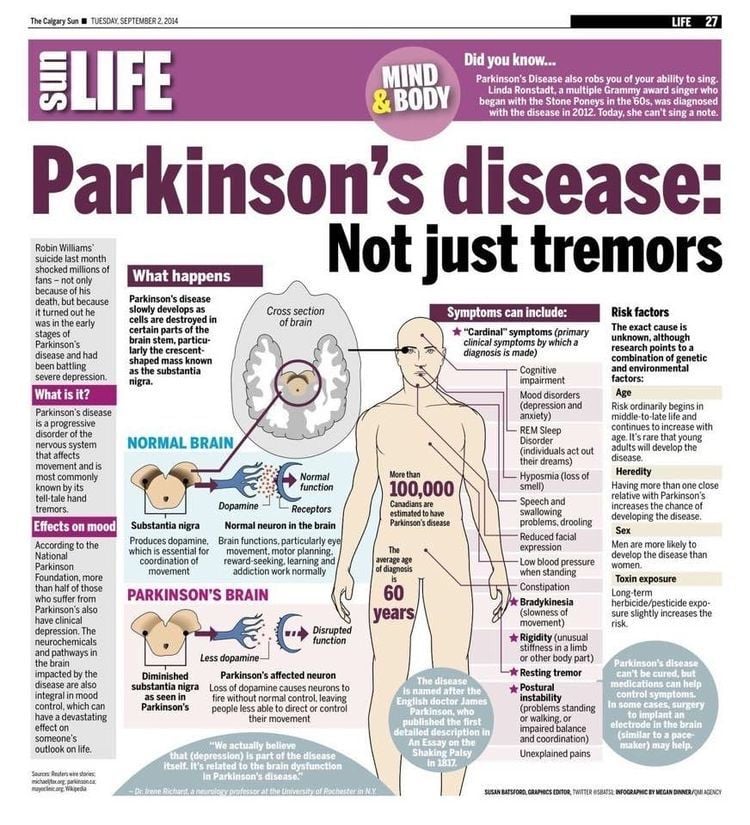
What Is Parkinsons Disease
Parkinsons disease is a condition where a part of your brain deteriorates, causing more severe symptoms over time. While this condition is best known for how it affects muscle control, balance and movement, it can also cause a wide range of other effects on your senses, thinking ability, mental health and more.
Also Check: Drugs For Tremors Of Parkinsons
You May Like: Foods Not To Eat With Parkinson’s Disease
What Are The Next Steps To Take If A Carer Thinks A Person Has Reached Advanced Stage Pd
In the advanced stages of PD, a persons care may become more complex. Carers can work with the person they are caring for as well as social and healthcare professionals and family members to come up with a care plan.
The APDA suggests that if caring duties become too difficult to carry out with one person, they can consider hiring a home health aide to help carry out caring duties.
Theory Of Pd Progression: Braaks Hypothesis
The current theory is that the earliest signs of Parkinsons are found in the enteric nervous system, the medulla and the olfactory bulb, which controls sense of smell. Under this theory, Parkinsons only progresses to the substantia nigra and cortex over time.
This theory is increasingly borne out by evidence that non-motor symptoms, such as a loss of sense of smell , sleep disorders and constipation may precede the motor features of the disease by several years. For this reason, researchers are increasingly focused on these non-motor symptoms to detect PD as early as possible and to look for ways to stop its progression.
Page reviewed by Dr. Ryan Barmore, Movement Disorders Fellow at the University of Florida, a Parkinsons Foundation Center of Excellence.
Also Check: What Medications Can Cause Parkinson’s
What Are The Symptoms Of Parkinson Disease
Parkinson disease symptoms usually start out mild, and then progressively get much worse. The first signs are often so subtle that many people don’t seek medical attention at first. These are common symptoms of Parkinson disease:
- Tremors that affect the face and jaw, legs, arms, and hands
- Slow, stiff walking
Definition Of Parkinsons Disease
Parkinsons syndrome is characterized by the clinical triad of rigor, tremor, and akinesia as well as possible postural instability.
Based on etiology, one can further distinguish between idiopathic Parkinsons disease, which is synonymous with Parkinsons disease, and atypical and symptomatic parkinsonism.
Idiopathic Parkinsons disease or Parkinsons disease is considered a diagnosis of exclusion, in the absence of a specific cause.
Symptomatic Parkinsonism, however, is triggered by certain identifiable factors. For example, in the context of intoxication, manganese or lead may cause the disease. Parkinsons syndrome is also triggered by medication, e.g., neuroleptics.
Parkinsons syndrome occurring in the context of other neurodegenerative diseases is referred to as atypical Parkinsonism.
Recommended Reading: Does Vitamin B12 Help Parkinsons
You May Like: Voice Therapy Exercises For Parkinson’s
What To Expect In The Late Stages Of Parkinsons Disease
The late stages of PD are medically classified as stage four and stage five by the Hoehn and Yahr scale:
- Stage Four of Parkinsons Disease In stage four, PD has progressed to a severely disabling disease. Patients with stage four PD may be able to walk and stand unassisted, but they are noticeably incapacitated. Many use a walker to help them. At this stage, the patient is unable to live an independent life and needs assistance with some activities of daily living. The necessity for help with daily living defines this stage. If the patient is still able to live alone, it is still defined as Stage Three.
- Stage Five of Parkinsons Disease Stage five is the most advanced and is characterized by an inability to arise from a chair or get out of bed without help. They may have a tendency to fall when standing or turning, and they may freeze or stumble when walking. Around-the-clock assistance is required at this stage to reduce the risk of falling and help the patient with all daily activities. At stage five, the patient may also experience hallucinations or delusions.1,2
Recommended Reading: Weighted Silverware For Parkinsons
Parkinsons Disease: When Is It Time For Hospice
Knowing when its time for hospice care when living with Parkinsons Disease can be difficult as the disease may take many years to progress and each person with the disease may also exhibit a range of different symptoms. However, entering the end-stages of the disease , patients will have symptoms that will indicate that it is time to seek hospice assistance:
Also Check: Mental Changes With Parkinson’s Disease
Starting Palliative Care In Patients With Pd
Patients with PD benefit early from palliative care in view of the impact of the disease impairing autonomy and quality of life. The provision of palliative care in patients with PD focuses on unmet needs and should be aligned with patient priorities. It is recommended that a palliative care approach should be applied from the early phase, throughout the course of the disease, complementing but not replacing other treatments . However, like other patients with chronic neurological condition, the individual needs may vary over time, therefore it is suggested that a model of dynamic involvement of palliative care services should be adopted . The services can be triggered at times of particular symptoms or psychosocial issuessuch as the start of new interventions or at the very end of life.
For patients with complex physical, social, psychological and/or spiritual needs that do not respond to simple or established protocols of palliative care, there should be access to the support from specialist palliative care service .
However, rate of use of hospice in PD patients has been low . Caregivers often considered palliative care services to be synonymous with hospice care, and hence they did not consider this service option . Health care workers also have uncertainty about timing of palliative care, such that it was often not introduced until a crisis point .