Risk Of Parkinson’s Disease In Patients With Psychiatric Disorders
The influence of mental illness early in life on the subsequent risk of PD and its clinical picture remain obscure. Several studies have identified certain psychiatric illnesses, particularly anxiety, depression and schizophrenia as risk factors for PD. Anxiety has been suggested to be one of the earliest manifestations of PD in several case-control and cohort studies.
Mild Cognitive Impairment And Dementia
Cognitive impairment and the development of dementia are increasingly being considered part of the course of Parkinsons disease. Of particular importance, nearly 90% of PD patients with dementia exhibit at least one neuropsychiatric symptom, and 77% have two or more neuropsychiatric symptoms. Risk factors for the development of mild cognitive impairment include older age at disease onset, male gender, depression, severity of motor symptoms, and advanced disease stage .
The prevalence of dementia in PD is estimated at 26% to 44%, with over 80% developing dementia within 20 years of diagnosis. Mild cognitive impairment in people with PD is associated with the development of dementia within 4 years . Depression can exacerbate cognitive impairments in PD, and the frequency of depression in PD is estimated at 25% to 33% .
In a study that examined clusters of neuropsychiatric symptoms and cognitive status in PD, it was found that in people suffering from hallucinations nearly 80% had dementia in those with mixed neuropsychiatric symptoms nearly 58% had dementia and in those with mild depression 31% had dementia. Patients experiencing hallucinations tended to have longer disease duration, more severe motor symptoms, and older age .
Degeneration Of Neurotransmitter Systems
More widespread dopaminergic deficits in the brain
By definition, all patients with PD have a moderate-to-severe loss of dopaminergic neurons in the nigrostriatal projection pathway. More widespread degeneration of dopaminergic terminals in the striatum particularly denervation of dopaminergic terminals in the associative dorsal caudate nucleus occurs in those with PD-MCI than in those with PD without cognitive impairment . However, in patients with PD-MCI, there is relative preservation of other dopaminergic systems in the brain, whilst those with PDD have a considerable loss of the lateral dopaminergic system to frontal, parietal and temporal cortical regions . In healthy individuals, cortical dopamine modulation can boost working memory as well as visuospatial and attentional processing, and promotes cognitive effort,, suggesting a key role for dopamine in cognitive function.
Fig. 2: Neurotransmitter deficits associated with cognitive decline in PD and DLB.
Noradrenergic locus coeruleus and sympathetic systems
Basal forebrain cholinergic systems
Serotonergic dysfunction is not directly related to cognitive decline
Read Also: Prayer For Parkinson’s Disease
How Are Cognitive Problems Treated
Much remains to be learned about the basic biology that underlies cognitive changes in PD. Researchers work towards the development of diagnostic tests to identify people who seem to be at greatest risk for cognitive changes and to differentiate cognitive problems in people with PD from those that occur in another disorder related but different known as dementia with Lewy bodies.
David: On Anxiety Sleep And Focusing On The Positive
David , a 74 year-old man with PD diagnosed two years ago, has been dealing with anxiety and depression for decades. I was in therapy as a teenager and young adult for issues of anxiety and depression. But about five to six years ago, the anxiety worsened, and he sought out the care of the same therapist he saw when he was in his thirties.
The intensification of his anxiety preceded his diagnosis of PD by a few years, a relatively common phenomenon in which particular non-motor symptoms of PD appear before the motor symptoms. In addition, since his diagnosis of PD, he started noticing some cognitive issues specifically trouble with his memory and word-finding difficulties.
Initially, controlling the anxiety and dealing with the cognitive changes were very difficult for David and the two issues were inter-related for him. A word-finding difficulty would inevitably trigger anxiety. I used to go crazy because I couldnt think of particular words. And that anxiety would then make it even harder to find the right word.
He cant emphasize enough the importance of a good nights sleep. He used to get four hours of restless sleep. Now with the help of his more relaxed view of life and current medication regimen, he is able to get 6-7 hours of restful sleep and that has led to a major improvement in his quality of life.
Key lessons that David can share about his mental health include:
Recommended Reading: Parkinson’s Bike Therapy
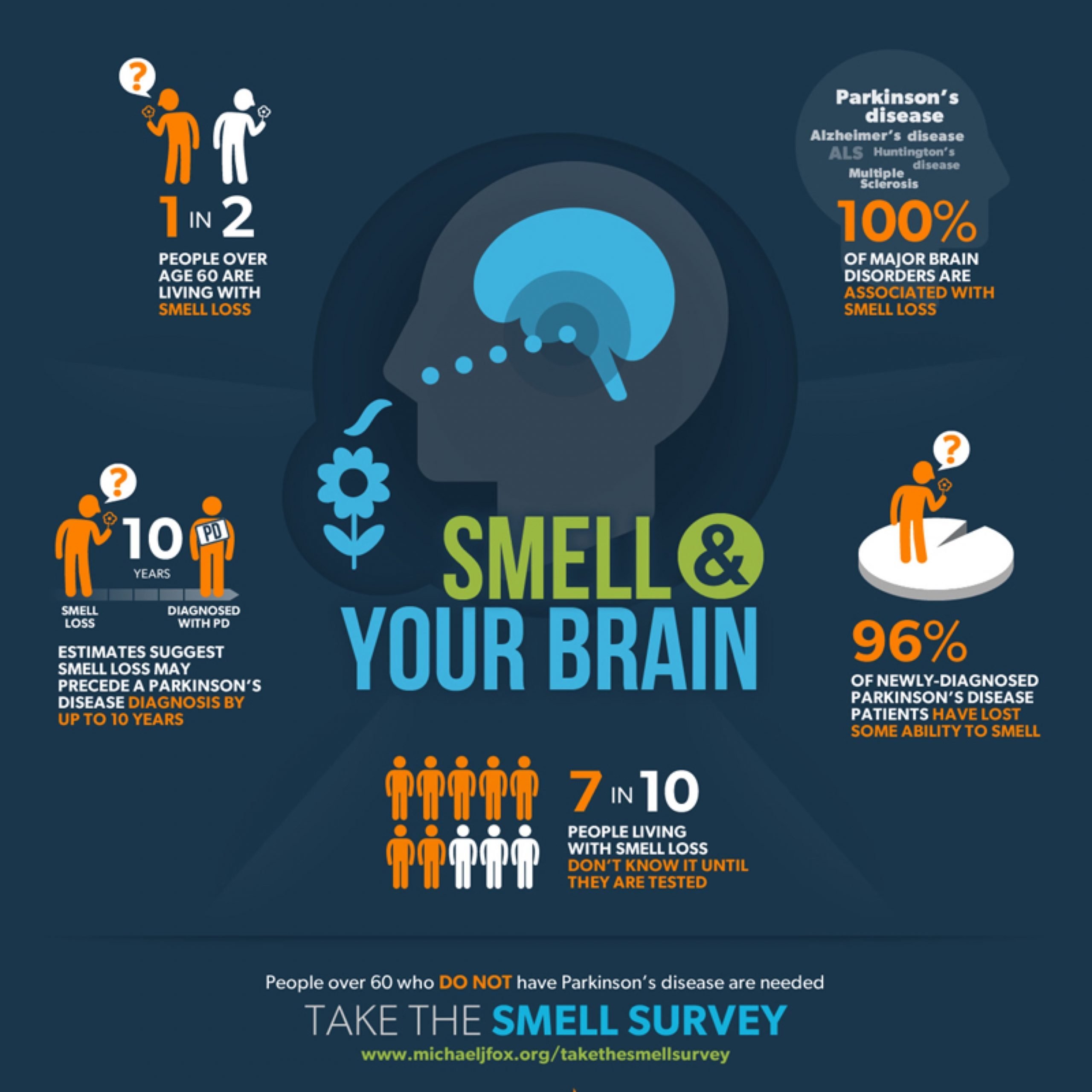
Prodromal Pd Phenotypes And Conversion
Recent evidence suggests that individuals with prodromal features of PD, such as hyposmia , REM sleep behaviour disorder and reduced dopamine transporter binding, may present with worse cognitive performance compared with people without any or with only one of these features,,. Interestingly, prodromal PD and DLB may overlap and it is not yet known how to distinguish between those who will develop PD versus those who will develop DLB. Of note, cognitive deficit has been recently defined as a new prodromal marker and has been included in the last update of the research criteria for prodromal PD.
Brain Boost: A Conversation On Thinking
In this 1-hour webinar a panel of experts and a person with Lewy Body Dementia answered moderator questions about cognitive changes typical in those with Parkinson’s Disease and Lewy Body Dementia . They discussed what’s normal and what’s not, the impact cognitive changes have on everyday life, what you can do to preserve brain health, strategies for both the person with PD and care partners to cope with cognitive changes, and what researchers know about predicting who is likely to suffer significant cognitive change with PD.
Read Also: Parkinson Silverware
What Are The Types Of Parkinsons Hallucinations
Hallucinations can affect any of the five senses:
- Sight . Seeing something that isnt there, such as insects crawling on the walls or a deceased relative.
- Hearing . Hearing voices or sounds that arent real.
- Smell . Smelling an odor that isnt there, like cookies baking or a skunks spray.
- Feeling . Feeling imaginary things, like bugs crawling on your skin.
- Taste . Having a strange taste in your mouth that isnt from something youve eaten or a medical condition.
Some people sense the presence of a person or an animal nearby. Others see real objects transform into other things for example, a vase changes into a dog.
Its more common to have hallucinations at night, when the darkness creates shadows. Hallucinations can last anywhere from a few seconds to a few minutes.
Early in the disease, most people with Parkinsons psychosis have insight, which means they understand that what theyre experiencing isnt real. Later in the disease, often people lose insight and believe that what they see, hear, or feel is real.
Language Dysfunction In Parkinsons
There are several functions within language, including naming objects, generating words, comprehension, and verbal concepts. PD most often affects a persons ability to find a word, although as PD progresses, additional language difficulties may develop, including difficulty naming, difficulty comprehending information, and the use of more simplified and less spontaneous speech.3,4
Read Also: Sam Waterston Parkinson’s
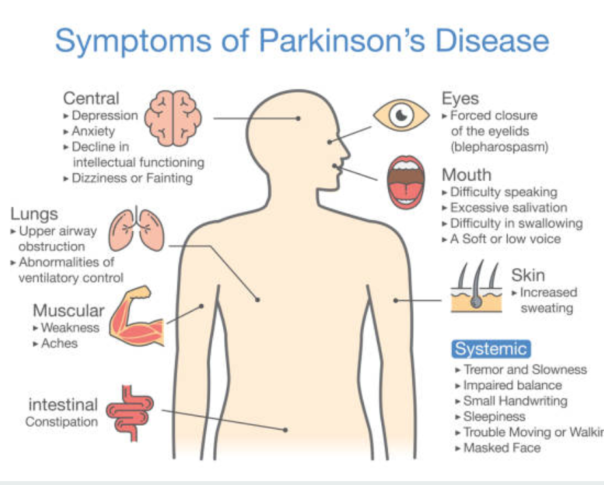
How Does Parkinsons Affect The Body
Parkinsons Disease has a big physical impact on the body, as most of the side effects and symptoms are physical. Physical impacts on the body includes:
- Slowing of the body
- A tremor that is often apparent when the body is at rest
- Stiffness of a limb or the body as a whole
- Moving at a much slower
- Trouble walking or mobility
- Difficulty keeping ones balance
- Loss of coordination & balance problems
- Loss of ability to express emotions through facial expressions
- Difficulty controlling movement throughout the body
- Sudden drops in blood pressure
These physical side effects of this disease can heavily impact an individuals quality of life, as well as their ability to live the same type of life that they did before their diagnosis. Technically speaking, Parkinsons will have a huge impact on an individuals physical well-being, as most of the symptoms and side effects directly impact their way of life. Parkinsons can also worsen over time for some individuals, causing their physical wellness to suffer greatly. Parkinsons can cause individuals to lose their ability to walk, sit or stand as they used to. This will impact their overall bone and muscle mass, giving their body a greater chance of deterioration over time.
Biomarkers Of Cognitive Decline
Many of the pathologies associated with cognitive impairment can be identified in vivo using a variety of imaging and blood-based or CSF-based markers. These biomarkers can be used to provide an increased understanding of the mechanisms underlying cognitive impairment in PD and, from a clinical perspective, can identify patients with an increased risk of early and rapid cognitive decline.
One of the first identified predictive markers was temporo-parietal atrophy on MRI , confirmed in many subsequent studies. In addition, basal forebrain atrophy observed using MRI is also associated with cognitive impairment in PD,. Hypometabolism in the medial frontal and parietal regions using FDG-PET is associated with a decline in executive and memory function. More recent MRI techniques, such as diffusion tensor imaging, also hold promise as biomarkers of cognitive function. For example, increased radial and axial diffusivity in the thalamus observed using diffusion tensor imaging was associated with a decline in MoCA scores.
Read Also: Similar To Parkinsons
Other Causes For Your Symptoms
Many people with Parkinsons also have depression or anxiety. These conditions can affect your motor function, balance, memory, or recall. Treating your depression or anxiety may help improve cognitive symptoms.
Parkinsons often causes sleep problems, like insomnia or waking during the night, or fatigue. Poor sleep and fatigue can affect your memory, walking, ability to complete tasks, alertness, or concentration.
A lack of vitamin B12 and thyroid problems can also cause cognitive symptoms. Your doctor will want to rule these out before making a diagnosis.
How Are Mental Health Problems Treated In Parkinsons Disease
Mental health problems in Parkinson’s disease can be treated with a combination of medication, talking therapy and lifestyle changes. Your doctor may also suggest joining a Parkinsons support group so that you can share your challenges with other PD patients.
Other ways to care for your mental health if you have Parkinson’s include:
Parkinson’s disease and mental health problems are not easily cured. However, there are a variety of treatment options and lifestyle changes that can boost your mental wellbeing and improve your overall quality of life.
Don’t Miss: Sam Waterston Tremor
Patient And Public Involvement
In the past years, there has been growing attention on the need to include patients, their caregivers and families in all stages of the research process. The increasing contribution of patient and public involvement groups in defining research questions, designing and conducting clinical trials, disseminating outcomes, and shaping research roadmaps reflects the concept of research as a shared effort among all stakeholders. Although in PD research this concept is increasingly being recognized, further involvement of patients and families, also inclusive of diverse patient populations, in research focused on PD-associated cognitive impairment is needed.
Classification Issues And Prodromal Stages
The proposal that dementia prior to or simultaneous with motor symptoms can be included in the diagnostic criteria for PD, has reopened the long-standing debate on whether PDD and DLB should be considered the same disease,,,. A deeper understanding of the pathophysiological processes underlying these two synucleinopathies, such as the relative contribution of -amyloid and tau pathology in cortex and striatum, the extent of cortical Lewy pathology and -synuclein load in the hippocampus, the severity of neuronal loss in the substantia nigra, and cholinergic cell loss, is required to better understand the relationship between PD and DLB.
Although some risk factors for cognitive impairment have been identified,,, further research is needed to better identify any early evidence of cognitive impairment in genetic at-risk populations and in individuals with clinical features of prodromal PD to provide opportunities for prevention strategies and early precision therapy interventions.
Don’t Miss: Parkinson Bicycle Cleveland Clinic
Do Something Nice For Yourself Every Daydo Not Drop Out Of The Mainstream Of Life
Enlist other family members to assist on a regularly scheduled basis Hire aides at home for several hours on a regular basis Participate in exercise programs Participate in education seminars and support groups Consult with a mental health professional Have a home safety evaluation Make use of adult day-care programs
Care partners must be reminded that their health is at stake, and that they are entitled to have some free time to recharge their emotional batteries. Recommendations for alleviating the burden for the primary care partner are listed in Box 2. Care partners should all be encouraged to participate in PD support groups and educational programs, as they will benefit from the advice and experience of others who have had to cope with similar situations. Consultation with a mental health professional is important for care partners who are becoming overwhelmed or depressed.
Family members or friends often say they are willing to pitch in and help the primary care partner without committing to a specific schedule. The assistance of other family members should be arranged on a predictable and regular basis. This might enable the primary care partner to make plans in order to re-engage in the mainstream of life . The assistance of family members on a haphazard basis or only during emergency situations does not ease the ongoing daily burdens for the care partner.
Anhedonia In Parkinson’s Disease
Although anhedonia is understood as a symptom of depression in patients with PD, studies suggest that it may be characteristic of PD itself which could be due to the dysfunction of the dopamine reward pathway in the mesolimbic area. Studies that have evaluated the prevalence of anhedonia have reported a range of 7% to 45.7%. With regards to the prevalence of anhedonia and depression, studies suggest a strong correlation between the two however, in many patients anhedonia is present in the absence of depression. Studies also suggest an association between anhedonia and apathy. Studies are inconclusive with regard to the relationship of anhedonia with severity of motor symptoms. With regards to management of anhedonia, which is independent of depression, no studies have specifically evaluated the efficacy of any pharmacological agent.
Recommended Reading: Pfnca Wellness Programs
Treatment Of Neuropsychiatric Conditions
Drug treatments for neuropsychiatric symptoms are available, but most have limited evidence for safety and efficacy when used to treat patients with PD.7
Anxiety and DepressionAntidepressants are among the best studied, and recent systematic reviews suggest that selective serotonin reuptake inhibitors are the most effective and well-tolerated in patients with PD.8 However, other classes of antidepressants such as selective serotonin and norepinephrine reuptake inhibitors and tricyclics may be equally effective, although with a slight increase in potential side effects. While there are currently no evidence-based drug treatments for anxiety in persons with PD, antidepressants are likely useful, and cognitive-behavioral therapy has demonstrated efficacy across several trials for both anxiety and depression.9
ApathyTreatment of apathy is a major unmet need. Optimizing dopaminergic management for the motor symptoms of PD can improve the patients level of activity but does not eliminate apathy.
Impulse-Control DisordersTreatment of impulse-control disorders includes eliminating the triggering agent, which is usually a dopamine agonist, and obtaining appropriate psychiatric consultation.
What Are The Signs Of Depression
Depression can sometimes make your Parkinson’s symptoms worse. Get in touch with your doctor if you notice any of these things happening to you for longer than 2 weeks at a time.
- You have a depressed mood.
- You can’t find pleasure in things that you once enjoyed.
- You have trouble getting to sleep or you sleep too much.
- Your appetite changes.
- You have thoughts of death.
You May Like: Judy Woodruff Parkinson’s
Impact Of Pd Treatments
The clinical choice of initial PD medication inhibitor) at disease onset does not seem to make a difference in terms of cumulative dementia rates,. However, there is strong evidence that medications with anticholinergic properties , and particularly the long-term exposure to multiple medications or medications with greater anticholinergic properties, are associated with worse long-term cognition in the general population and patients with PD,, and thus represent a target for clinical management. In patients with PDD, simplification of antiparkinsonian treatment through a stepwise withdrawal of non-levodopa PD medications starting with anticholinergic drugs, followed by amantadine, selegiline, dopamine agonists and then catechol-O-methyltransferase inhibitors, might be useful, particularly if comorbid psychosis is present.
In addition, several studies have found that DBS can worsen cognitive functioning as a result, cognitive testing is recommended as part of the pre-DBS surgery evaluation process, and patients with severe cognitive impairment should not undergo brain surgery. However, the use of model-based stimulation parameters to minimize the spread of the electrical current to non-motor portions of the subthalamic nucleus reversed the cognitive decline that occurred after DBS in one study. Encouragingly, a subsequent study of DBS in younger patients with shorter disease duration showed short-term cognitive tolerability similar to the best medical therapy.
Thinking Changes In Parkinson’s

In this 1-hour webinar Travis Turner, PhD, explains why you might be referred for a neuropsychological evaluation, what is done during such an evaluation, how the information learned during an evaluation is used, and tips for performing your best during an evaluation. After the talk he answered several questions about coping with cognitive changes when you have PD or are caring for someone with PD.
Also Check: Diseases Similar To Parkinsons
How The Brain Progresses With Pd
In this one-hour webinar movement disorder specialist Yasar Torres-Yaghi shared how the pathology of Parkinson’s disease begins in the gut before progressing to the brain. As the pathology expands throughout the brain it affects more neurotransnitters than just dopamine causing both motor and non-motor symptoms. Dr. Torres-Yaghi shares a widely used cognitive evaluation tool before answering questions about communicating well with your neurologist and advocating for the care you need.