Parkinsons Symptoms Including Pain And Frequent Urination
Pain is a common cause of sleep disturbances in Parkinsons, says Horvat. A study published in June 2019 in the Journal of Pain Research found that about one-third of people with Parkinsons had clinically relevant sleep disturbances, and that central parkinsonian pain was the pain subtype that was most often associated with sleep issues.
Central pain can vary widely from person to person. It can feel like a constant burning or tingling that affects the whole body or it can be an intermittent sharp episode of pain, according to the Parkinsons Foundation.
You should definitely talk to your doctor if pain or Parkinsons symptoms are waking you up or keeping you up at night, to see what your treatment options may be, says Horvat.
Frequent urination can be a sign of several different things, and so its important to pay attention to any other symptoms you may also be having, she says.
Autonomic instability is often present in Parkinsons disease, which basically means the autonomic system is not firing regularly, as it should be, says Horvat. The autonomic system controls functions that keep you alive, including your heartbeat, breathing, and digestion.
This condition can lead to incontinence or urinary retention, she says. This is something to talk with your doctor about there are some medications that can be helpful.
Financial Disclosures For The Past 12 Months
SM receives research support from the Michael J Fox Foundation , the Parkinson Foundation and Cerevel Therapeutics, was a paid consultant to MJFF, is a study site investigator for a study sponsored by Neuraly Rho, is a study site sub-investigator for a study sponsored by Biogen, and is contracted with Deep Brain Innovations, LLC. MD was an employee of the sponsor, MJFF, at the time this work was done. CK is an employee of MJFF. CM was a paid consultant for Acorda Therapeutics, on the advisory board of Denali therapeutics, received honoraria for teaching from EMD Serono, a steering committee member for MJFF Grants Canadian Institutes of Health Research, Parkinsons Foundation , National Institutes of Health , International Parkinson and Movement Disorders Society, and is contracted with Grey Matter Technologies. LC receives research support from MJFF, has received travel payment from MJFF to MJFF conferences, is a paid consultant to MJFF, receives research support from the UPMC Competitive Medical Research Fund, is study site investigator for a study sponsored by Biogen, is a site sub-investigator for a study sponsored by Voyager, received payment from Elsevier , and receives royalties from Wolters Kluwel . All other authors have no financial disclosures.
Hot Weather And Parkinsons
Was wondering if any experience more symptoms with hot Weather? Also wonder what helps to cope with hot weather?
Lots of arm jerking at moment and reply sent before I was finished. Try wearing a sweat band around your forehead. I have dozens and they really help. As I write this Im using energy and the sweating is troubling.
Increase water intake . Medication does not work well if you get dehydrated.
Wet a cotton scarf to wear round neck .
Hold wrists under cold tap for a few minutes.
Wipe over all skin with a cold flannel and leave to dry naturally.
Drink hot tea!
Dont Miss: Does Vitamin B12 Help Parkinsons
You May Like: Parkinson’s Information For Patients
What Are The Primary Motor Symptoms Of Parkinsons Disease
There are four primary motor symptoms of Parkinsons disease: tremor, rigidity, bradykinesia and postural instability . Observing two or more of these symptoms is the main way that physicians diagnose Parkinsons.
It is important to know that not all of these symptoms must be present for a diagnosis of Parkinsons disease to be considered. In fact, younger people may only notice one or two of these motor symptoms, especially in the early stages of the disease. Not everyone with Parkinsons disease has a tremor, nor is a tremor proof of Parkinsons. If you suspect Parkinsons, see a neurologist or movement disorders specialist.
Tremors
Fatigue In Parkinsons Disease And Potential Interventions
This abstract of a literature review discusses the measurement and pathophysiology of fatigue and fatigability. There rare no evidence-based treatments available. Several pilot studies are reviewed on the effects of pharmacological agents and exercise. These provide some insights on the design of future larger clinical trials. Fee for full article at IOS Press.
Recommended Reading: What Medications Are Used For Parkinson’s Disease
Is There Scientific Proof That The Time Of Year Can Affect Pd Symptoms
Despite these potential reasons that PD symptoms might be more pronounced at different times of year, especially in the winter, with cold weather and shortened days, studies that have been conducted to directly study this issue have had mixed results.
In one initial study, patients motor scores, as defined by the Unified Parkinsons Disease Rating Scale, were compared in various months of the year, and no differences were found. Similarly, another study demonstrated that seasonal variation did not affect hallucinations in PD, with no exacerbation of the condition during the winter.
In a different study, however, prescriptions of PD medications were analyzed in the winter and summer months. More PD meds were prescribed in the winter months, suggesting that there is a variability in PD symptoms depending on the season. Another study looked at non-motor symptoms which suggested that patients blood pressure fluctuations, sleep, and hallucinations were worse in the winter months than in the summer.
Although results from research studies are not clear, it is certainly possible that some people with PD may experience a variability in their symptoms as it relates to the season. If this is the case for you, discuss this with your doctor. Adjustments in your treatment and lifestyle depending on the time of year may be a good solution to help you feel better year-round.
Fatigue In Parkinsons Disease: Report From A Multidisciplinary Symposium
A summary of a symposium in October, 2014, reviewing what is known about the diagnosis and treatment of fatigue, its physiology, and what we might learn from other disorders in which fatigue figures prominently, and concluding with focused recommendations to enhance understanding and treatment of fatigue in Parkinsons disease.
Don’t Miss: Parkinson Like Tremors In Dogs
Clinical Measures Of Fatigue In Pd
A systematic critique of rating scales for diagnosis and severity of PD fatigue used pre-determined criteria for Recommended, Suggested, or Listed, depending on the quality of data. The FSS met the necessary criteria to be recommended for both diagnostic screening and severity measurement., The Multidimensional Fatigue Inventory was designated as recommended for rating fatigue severity, and may be more sensitive to change with interventions than the FSS. For diagnostic screening only, two other scales were recommended: Functional Assessment of Chronic Illness TherapyFatigue Scale and Parkinson Fatigue Scale . Since the MDS review article, the Modified Fatigue Impact Scale has been validated in a study involving 100 PD patients. This scale involves evaluation of cognitive as well as physical and social functioning.
Drinking Well Water Is Linked With A Higher Likelihood Of Developing Parkinsons
A growing body of research suggests that there is a correlation between drinking well water and developing Parkinsons Disease later in life. One particular study, conducted by a team at UCLA and published in the journal Environmental Health Perspectives, found that those who consume well water are statistically more likely to develop PD. After reviewing the medical records and personal histories of 700 people living in Californias farm belt between 1974 and 1999, they determined that those who ultimately developed PD had consumed private well water on average 4.3 years longer than those who did not.
Read Also: How To Test For Parkinson’s
Can Parkinsons Be Treated Without Medication
Medication aside, there are many ways people living with Parkinsons disease can improve their health and well-being, preserve physical function, ease symptoms and enhance quality of life. Chief among these are getting regular exercise, eating a healthy diet, staying hydrated and getting an adequate amount of sleep.
You May Like: Sam Waterston Parkinsons
How Are Sleep Problems Treated In People With Parkinsons Disease
Your provider will recommend treatments that address whats causing your sleeping challenges. Your provider may:
- Change your medication: If a medication could be causing your sleep issues, your provider may decide to adjust your treatment plan. Reducing the dose or switching medicines may solve the problem.
- Prescribe a new medication or therapy: If you have a sleep disorder, your provider will discuss your options. In some cases, your provider may recommend a new medication. If you have sleep apnea, wearing a special oral appliance can help. The device enables you to get a steady flow of oxygen, so your body doesnt gasp for air.
- Suggest lifestyle changes: Your daily habits and sleeping environment can help or hurt your sleep efforts. Setting regular sleep and wake times, keeping the room dark and avoiding electronic screens at bedtime may improve how well you sleep. If you have REM sleep disorder, your provider will discuss options for how best to protect you while you sleep.
You May Like: Diet For People With Parkinson’s
How Can I Prevent A Heat Illness What Can I Do To Reduce My Risk Of Heat Illnesses
Heat illnesses are very preventable. Use the following simple steps to keep yourself from getting overheated:
- Drink water every 15 minutes when working or exercising in a hot environment, even if youre not thirsty. If you need to be out in extreme heat , drink a total of two to four glasses of water each hour.
- Take periodic rest breaks in the shade, a cool area or air-conditioned space.
- When working or exercising outside in hot, humid weather, wear a hat and loose, lightweight, light-colored cotton clothing.
- Do not drink alcohol or beverages that contain caffeine.
- Avoid going outdoors for activities or exercise when the temperature and humidity are high.
- Wear sunscreen. A sunburn reduces your bodys ability to cool down. It can also dehydrate you.
- Wear a wide-brimmed hat and sunglasses outside.
- Avoid eating a hot, heavy meal.
- Pace yourself. Rest often.
- Monitor your urine output. If you urinate too much you could have a heat illness.
Remember that your body needs electrolytes, not just water. You can get electrolytes from common sports drinks, or powders you can add to your water. Choose an electrolyte drink or solution thats low in sugar.
You May Like: Sam Waterston Tremor
Fourth Type Of Leg Pain Is Radicular Pain
In this case, the pain is caused by compression of nerves in lumbar area which results in weakness, numbness and tingling, and loss of reflexes from buttocks to foot in a distribution of a nerve. It can be acute or chronic, and can be worse with standing and sitting, or better with laying down. Of note: in my experience many patients including myself have these symptoms not because of physically herniated disc but rather by the stretching of a nerve in the canal as it exists due to severe musculoskeletal rigidity and abnormal posturing.
Don’t Miss: Dopamine Agonist For Parkinson’s
Tips For Better Sleep
The best place to start is with your doctor, who may be able to change or adjust your Parkinsonâs medications so that they interfere with sleep less. In some cases, you might be able to take a medication that helps you stay awake during the day so you sleep better at night.
If you have a sleep disorder or depression, other medications may help. Be sure to ask your doctor before taking any over-the-counter sleep medications. Many contain an antihistamine, which can actually make Parkinsonâs symptoms worse.
There are also sleep strategies you can try for yourself:
Stick to a regular sleep schedule. Getting up and going to bed at the same time every day, even on weekends, can help regulate your sleep cycle.
Avoid caffeine for at least six hours before bedtime. That means chocolate as well as coffee, tea, and sodas with caffeine.
Stay active during the day and avoid taking naps. The energy you expend during the day will leave you more tired at night. Complete your exercise regimen at least 3 hours before bedtime to optimize pre-sleep relaxation.
Get outside for some exercise every day. Morning sunshine helps set your biological clock.
Limit fluids in the evening. Avoid drinking a lot of fluid in the hours before bed to cut down on the need to urinate in the middle of the night.
Try a relaxation routine. Get in the habit of treating yourself before bed to a relaxing activity such as a hot bath or shower or a gentle massage.
When To Seek Hospice Care
When you or your loved one have a life expectancy of six months or less, you become eligible for hospice care a type of comfort care provided at the end of life for someone living with end-stage Parkinsons disease. Hospice provides extra support so your loved one can live as comfortably as possible.
If you have experienced a significant decline in your ability to move, speak, or participate in activities of daily living without caregiver assistance, its time to speak with a hospice professional.
Read more: What is hospice care?
Some of the things that determine whether your loved one with end-stage Parkinsons is eligible for hospice include: difficulty breathing, bed bound, unintelligible speech, inability to eat or drink sufficiently, and/or complications including pneumonia or sepsis.
If you live in South Jersey, our nurse care coordinator can answer your questions and decide if your loved one is ready for hospice care. Call us 24/7 at 229-8183.
Don’t Miss: How Many People In Us Have Parkinsons
What Causes Parkinsons Disease
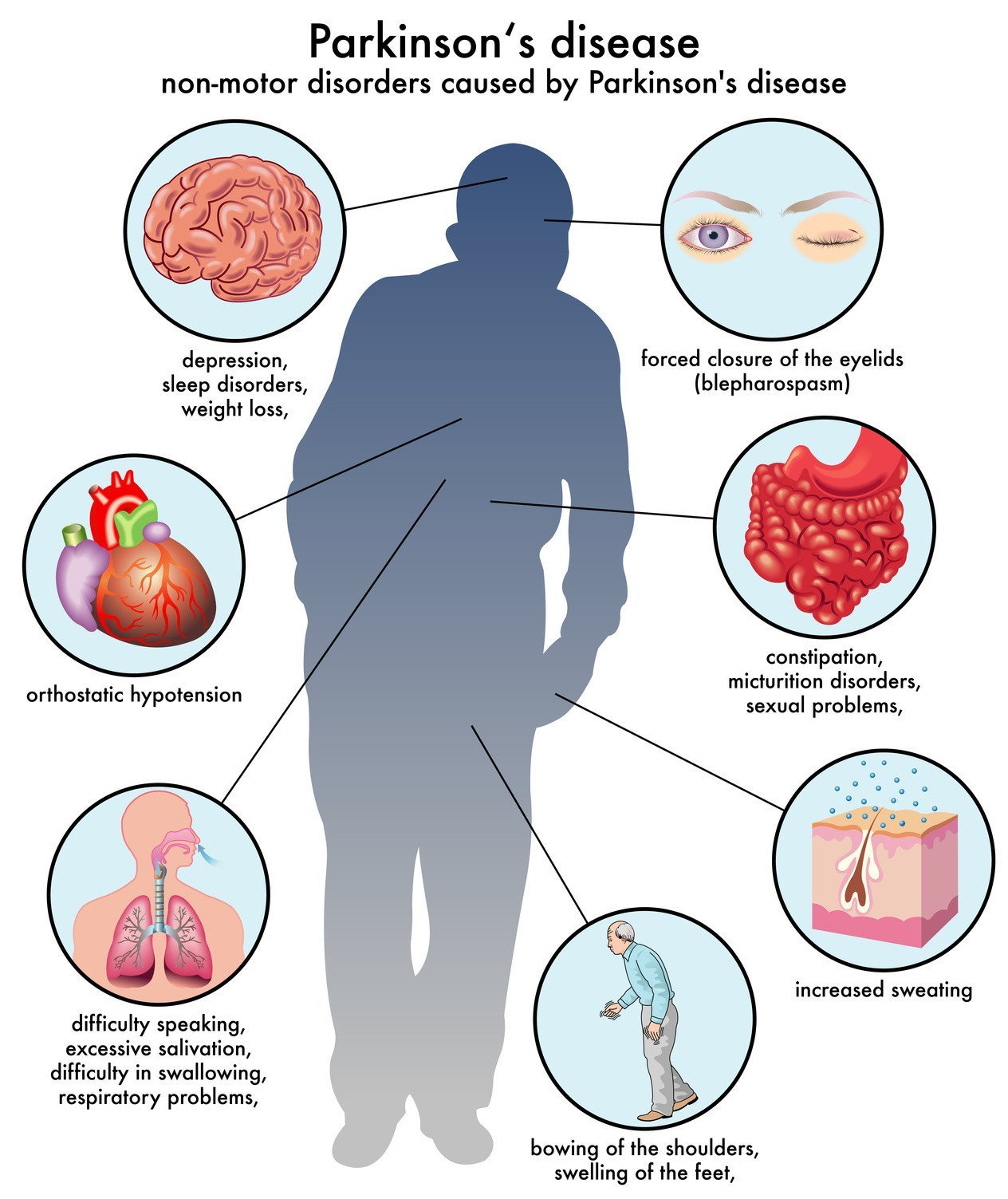
Parkinsons disease occurs when nerve cells in an area of the brain called the substantia nigra become impaired or die. These cells normally produce dopamine, a chemical that helps the cells of the brain communicate . When these nerve cells become impaired or die, they produce less dopamine. Dopamine is especially important for the operation of another area of the brain called the basal ganglia. This area of the brain is responsible for organizing the brains commands for body movement. The loss of dopamine causes the movement symptoms seen in people with Parkinsons disease.
People with Parkinsons disease also lose another neurotransmitter called norepinephrine. This chemical is needed for proper functioning of the sympathetic nervous system. This system controls some of the bodys autonomic functions such as digestion, heart rate, blood pressure and breathing. Loss of norepinephrine causes some of the non-movement-related symptoms of Parkinsons disease.
Scientists arent sure what causes the neurons that produce these neurotransmitter chemicals to die.
Sweating And Temperature Regulation In Pd
People with Parkinsons experience changes to the autonomic nervous system, which controls sweating. While sweating controls temperature regulation, too much or too little sweating can result in feeling overheated. Here are some resources to understand sweating and temperature regulation, and how to cope with it.
You May Like: First Signs Of Parkinson’s
How Is Fatigue Treated
Although fatigue is common in Parkinsons, it has often been rather neglected by doctors. There are numerous causes of fatigue that are unrelated to Parkinsons but these still need to be recognised for treatment to be successful.
You should first talk with your doctor or specialist to let them know how fatigue affects you and what changes you have noticed over recent months. They will then carry out any tests they feel are appropriate.
Medication: If your doctor suspects that your Parkinsons treatment is a factor they may recommend a change in medication so that symptoms are better managed, which should give you more energy.
Sleep: It is important to understand the reasons for poor sleep and to treat symptoms that disturb your sleep pattern. For example tremor, stiffness or restless legs may interrupt your sleep, or you may need to use the toilet at night. Your doctor will be able to suggest ways to manage these symptoms and so improve your sleep and reduce fatigue.
See also: Apathy.
Lifestyle: Advice to improve fitness through regular daily exercise may be useful. Depending on where you live, you may be referred to an occupational therapist or physiotherapist specially trained in the management of fatigue who can suggest a personal programme of activity and relaxation. In some countries your doctor may refer you to specialist community teams who help people manage chronic fatigue syndrome and can advise on fatigue disorders.
Parkinsons Disease Education Consortium 2018 Research Program Overview
This work was undertaken as part of the Michael J Fox Foundations Parkinsons Disease Education Consortium 2018 research program. The PDEC objective relevant to the present analysis was to understand how individuals with PD experience fatigue.
The PDEC 2018 research program undertook a mixed-methods approach that involved three phases , each of which built on prior phases. Initial phases were aimed at in-depth analysis in a small sample, before expanding to a larger cohort of people with PD. Phase 1 was an online journaling activity, in which an online moderator interacted with individuals with PD via a series of structured activities. Phase 2 involved semi-structured telephone interviews with a different set of participants. Phase 3 involved deployment of a survey to the Fox Insight study cohort. Each of these phases is detailed further below. Participants provided informed consent to each phase separately.
Fig.1
Flow chart of study recruitment phases.
Read Also: Parkinson’s Disease Is The Result Of
Pragmatic Management Of Fatigue In Pd
Treatment approaches focused on fatigue in PD are faced with 2 main limitations: lack of clear insight into its pathophysiology and mechanisms, and probably its multifactorial nature . Therefore, as stated by Kluger and Friedman, contemporary treatment of fatigue in PD is limited to an empirical approach based on plausible hypotheses .
Dont Miss: Living With Parkinsons Disease Video
Imaging Of Fatigue In Pd

Motor symptoms in PD result from nigrostriatal dopaminergic denervation, but dopaminergic dysfunction does not appear to be related to fatigue in PD. In the ELLDOPA cohort, 49 levodopa-naive PD patients with fatigue had similar –CIT striatal dopamine transporter uptake as 82 PD patients without fatigue. Another study showed no difference in 18F-dopa uptake between 10 fatigued PD subjects and 10 nonfatigued PD subjects.,
Serotonin transporter uptake has been reported to be reduced in chronic fatigue syndrome,, suggesting that nondopaminergic pathways may be involved in PD fatigue. Pavese et al. compared serotonergic transporter uptake ligand 11C-DASB) in seven PD subjects with fatigue and eight PD subjects without fatigue. Serotonin transporter binding in the caudate, putamen, ventral striatum, insula, and thalamus was decreased in the fatigued patients. The relationship of the cholinergic system to PD fatigue has not been investigated. The autonomic nervous system may also be involved in PD fatigue. One study found that pressor responses in norepinephrine and dobutamine infusion tests were greater and MIBG cardiac uptake was decreased in PD subjects with fatigue compared with those without fatigue.,
Don’t Miss: How Can You Die From Parkinson Disease