How Common Is Parkinsons Disease Psychosis
Between 20-40% of people with Parkinsons report the experience of hallucinations or delusions. When followed as the disease progresses over the years, this number increases. The increase does not mean that the hallucinations are persistent across the majority of patients. However, it is important to note that these statistics sometimes include delirium, in which the symptoms are temporary due to medication that needs to be adjusted or infection that needs to be treated, and isolated minor symptoms or minor hallucinations, including illusions, where instead of seeing things that are not there , people misinterpret things that are really there. These are the most common types of psychosis in people with PD, with different studies placing the occurrence between 25-70% of people with Parkinsons. Typically, if the person with PD only has these minor hallucinations, their doctor will not prescribe an antipsychotic medication, though more significant psychosis that requires medication may develop over time. In one study, 10% of those with minor hallucinations had their symptoms resolved within a few years, while 52% saw their symptoms remain the same and 38% saw their psychosis symptoms get worse.
We recommend that people with Parkinsons not use a single percentage to represent the prevalence of hallucinations and PDP. Parkinsons is a complex disease and as it progresses the percentages and risk of symptoms will change.
Also Check: Pfnca Wellness Programs
How Can Caregivers Support Their Loved Ones
Caring for someone who sees, hears, or believes things that arent real can be very difficult. Try to be as patient and calm as you can.
Avoid arguing with the person. If they still have insight, gently explain that what theyre seeing isnt real. Tell anyone who cares for or visits your loved one what to expect, and how to respond.
Stay in close contact with the persons doctor. If their symptoms dont improve, ask whether they need a medication adjustment.
Check whether the person needs hearing aids or glasses. Poor hearing or vision can sometimes lead to hallucinations. It can also help to turn on bright lights at night, to prevent the shadows that may trigger visual illusions.
Secure any dangerous objects, and keep pathways in the home clear to prevent falls and injuries. If you ever feel like the person is a risk to themselves or others, call their doctor.
Read Also: Parkinsons Getting Out Of Chair
Types Of Hallucinations In People With Parkinsons Disease
Hallucinations involve the five senses: sight, smell, touch, hearing, and taste.
People with hallucinations have sensory experiences that feel real to them, but are not actually happening and are not apparent to anyone else.
Types of hallucinations include:
- Auditory: Hearing things
- Gustatory: Tasting things
For people who experience Parkinsons-related hallucinations, the hallucinations are usually visual. They are typically non-threatening, but less commonly they can be of a threatening nature.
Often people with Parkinsons disease psychosis see small people or animals, or loved ones who have already died. They are not interacting with them, just being observed.
Auditory hallucinations are more common in people with schizophrenia, but can happen with Parkinsons disease. With Parkinsons disease, auditory hallucinations are usually accompanied by visual hallucinations.
More specific types of hallucinations experienced by people with Parkinsons disease include:
You May Like: Mental Changes With Parkinson’s Disease
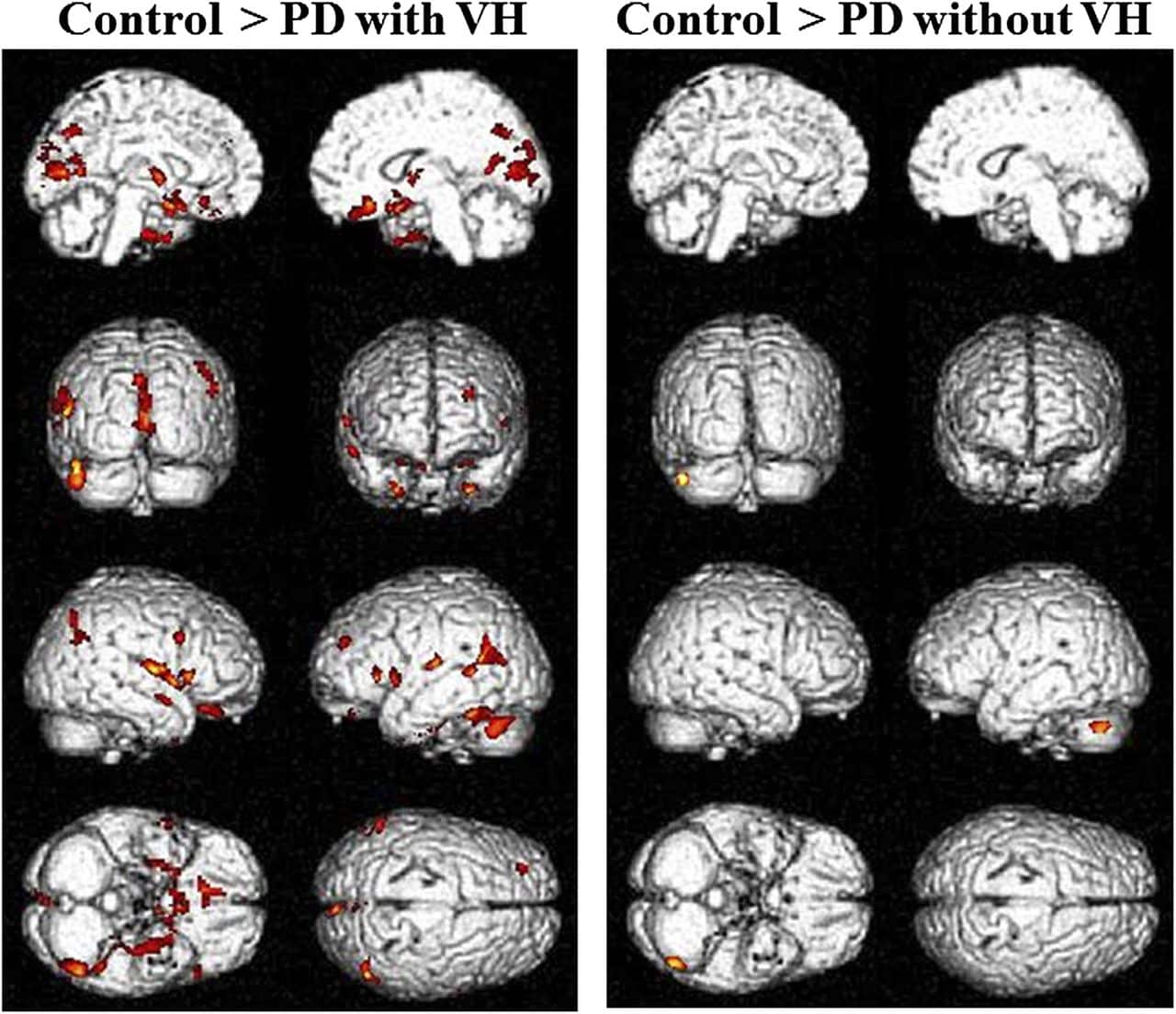
Demographics And Clinical Scores
Demographic results are summarized in Table 1. All groups were matched for age and there were no significant differences in duration of PD or levodopa dose between the PDD-CVH and PDD-NCVH groups. PDD patients displayed a significant reduction in global cognitive function, UPDRS motor score relative to controls, with the PDD-CVH group global cognitive function and motor function were significantly worse when compared to the PDD-NCVH group. The NPI recorded the severity of hallucinations as mild in 29.4% PDD-NCVH which were phenomenologically classified as Illusions , presence , shadow , and simple by the NEVHI. Further stringent grouping into PDD_NVH dropped the reporting of mild hallucinations to 10%.
Table 1. Participant demographics and clinical scores.
Do Hallucinations Go Away
Some visual hallucinations are so mild they might not even register on a conscious level, Dr. Ramdhani says. For instance, you may see a shadow thats not there, or glimpse something in your peripheral vision that clears when you turn your head. For some people, those may go away on their own, especially with a change in medication. In more advanced stages, though, these hallucinations may occur along with delusions, which means a false belieflike thinking your spouse isnt your real partner. Dr. Ramdhani says this can happen due to cognitive impairment, such as dementia.
You May Like: Video Of Parkinson’s Tremor
Whats The Treatment For Parkinsons Disease Psychosis
The single most important thing to do when it comes to Parkinsons disease psychosis is to tell your care providers and partners the minute you notice changes in your vision, hearing, thinking and behavior. The earlier they know whats going on, the sooner they can begin interventions to help you feel better.
Once you bring your concerns up to your doctor, they will typically do a clinical evaluation, review your medications and dosage, assess your lifestyle and determine the severity of your symptoms. Depending upon what they find, they may refer you to counseling or therapy, adjust your medication, change your medication, eliminate medication or do all of the above. If none of those strategies work, they may try antipsychotic drug therapy to see if they can adjust chemical levels in the brain. This can bring with it an entirely different set of problems so its important to be invested every step along the way and be sure youre well-informed before you move in that direction.
Dont Miss: Judy Woodruff Parkinsons
A Caregivers Guide To Parkinsons Disease Psychosis
While more than 50% of those taking carbidopa-levodopa may experience psychosis , medication management of these symptoms is a balancing act. First, families must bring psychotic behavior to the attention of your medical team. Medical causes of the behavior, like infection must be ruled out, followed by a review of medications and possible medication adjustments before a lifestyle changes and possible medications for treatment are added.
Read Also: Is Coffee Bad For Parkinson’s Disease
How Quest For Life Can Help
While medical teams focus on eradicating disease, Quest for Lifes focus is on empowering people to heal and live as vitally as possible. Quest for Life can help through our residential programs and 1-day workshops.
- Our 5-day residential Quest for Life program nourishes, educates and supports you to adopt a healthy lifestyle which creates an environment for profound healing. In addition to medical education about how the disease is best managed, the program explores many avenues of physical, mental, emotional and spiritual healing and encourages participants to find their own best answers. Partners and loved ones are encouraged to attend and some focused sessions are conducted specifically for them.
- Our 1-day workshop Living Mindfully with Cancer and Illness shows you ways to improve your health and create an environment for profound healing.
Quest for Life knows how to help: research shows that participants feel better after attending a program and that this improvement increases over time.
If youre living with Parkinsons Disease, fill in the Contact Form below and one of our Program Advisors will be in touch to answer your questions or to ascertain the most appropriate program for your needs.
Read Also: On And Off Phenomenon
Management Of Visual Hallucinations In Pd
Understanding the complex interactions between neurotransmitter systems in the context of neurodegeneration secondary to PD assists in efforts to treat psychotic symptoms as they arise. Management is complex and varies between patients. The first consideration should most obviously be prevention. When these symptoms occur acutely, systemic illness should be considered and treated. When symptoms persist, an increasing array of treatment options are available and can be tailored to the individual patient. A treatment algorithm is presented in .
FIGURE 1. Management flow chart for visual hallucinations in Parkinsons diseasea
a COMT=catechol-O-methyltransferase.
Recommended Reading: Parkinson’s Disease Is Caused By
Relation With Sleep Abnormalities
Idiopathic RBD, characterized by loss of normal atonia during REM sleep, is considered a risk factor for Parkinsons disease and other synucleinopathies: over 80% of idiopathic RBD patients may eventually develop a neurodegenerative disorder linked to -synuclein accumulation in the brain . Visuo-perceptual deficits have been reported in patients with RBD , with impairments in colour vision and visuospatial construction . Those RBD patients with sensory abnormalities at baseline have also been claimed to develop a form of Parkinsons disease with more prominent cognitive involvement . Later, at mid-stage, this same association, RBD and poor colour discrimination, is again linked with a more rapid and aggressive disease course . Although RBD is a rare prodromal sign in patients presenting with motor symptoms, up to a third of patients develop RBD in the course of their illness . When it occurs, it is associated with visuo-perceptual dysfunction, including errors in object recognition and complex figure copying . The presence of RBD in Parkinsons disease is also predictive of progressive cognitive dysfunction .
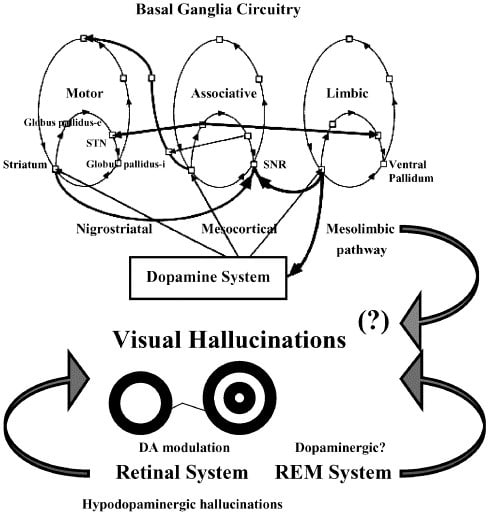
Pathology Of Neurotransmitter Pathways In Pd Psychosis And Relevance Of Medications
The distribution of pathology in PD involves key components of dopaminergic and other important neurotransmitter pathways implicated in PD psychosis. Dopamine is synthesized in the substantia nigra, with projections to the striatum, limbic system and frontal lobe , and five recognized dopamine receptors with broad distribution throughout the brain and peripheries at varying levels of expression . It is known that dopaminergic medications have differential actions across these receptors, and, similarly, antipsychotic medications display different binding affinities for individual dopamine receptors .
While loss of dopaminergic neurons within the substantia nigra is a central pathological feature of PD , neuronal loss also occurs in multiple other subcortical nuclei with projections to cortical, limbic, and basal ganglia regions. These include the dopaminergic nuclei of the ventral tegmentum, noradrenergic locus coeruleus, serotonergic raphe nuclei, histaminergic tuberomammillary nucleus of the hypothalamus, and cholinergic nucleus basalis of Meynert and the pedunculopontine nucleus . LB deposition and neuronal loss in the locus coeruleus occurs earlier and is more prominent than PD pathology in the substantia nigra, with some evidence that pathology in this region may contribute to subsequent dopaminergic cell loss, because noradrenergic neurons directly innervate the substantia nigra .
Also Check: What Is Vascular Parkinson’s Disease
Face And Emotion Recognition
The ability to recognize faces is impaired in Parkinsons disease , with performance correlated with grey matter density in the fusiform face area, the region involved in face recognition in the heathy brain . There is particular difficulty in interpreting facial expressions , with greater impairment for negative emotions including disgust , sadness and fear . This greater deficit for emotional face processing in Parkinsons disease may be explained by the presence of two distinct face processing pathways that are sensitive to different spatial frequency ranges: face identification, associated with the fusiform face area, is more activated by high spatial frequency ranges . In contrast, subcortical pathways, including the amygdala, are activated by fearful faces, and are driven by coarse, low spatial frequency information . The finding that performance improves in patients treated with l-DOPA is consistent with the involvement of dopaminergic neurons in this pathway .
Risk Factors For Parkinsons Psychosis
Understanding the risk factors for hallucinations and delusions can help you recognize symptoms of Parkinsons psychosis. The following factors may increase the likelihood of experiencing hallucinations and delusions:
- Advancing cognitive impairment, including worsening memory loss
- History of depression
- Sleep disorders and sleep disturbances
- Changes to medications
- Worsening medical conditions outside of Parkinsons
We have noticed that when my father had delusions, its been when his general health is not good, or when he has been in the hospital for PD-related issues, a MyParkinsonsTeam member commented.
Questionnaires used in a clinical setting can help assess the risk of developing hallucinations or delusions, or establish that they are occuring. These include:
- PD nonmotor symptom scale
- Parkinson Psychosis Questionnaire
- Scale for Evaluation of Neuropsychiatric Disorders in Parkinsons Disease
Individuals with Parkinsons or their caregivers can speak with a neurologist to understand if any of these tools would be helpful in their particular situation.
Also Check: Voice Amplifiers For Parkinsons
Read Also: Theracycle For Parkinson’s Disease
What Should I Do When My Loved One Is Experiencing A Hallucination
Most importantly, dont try to convince your loved one that what theyre experiencing isnt real. Theyll feel like youre putting down an experience that seems authentic to them.
Once a person has lost insight, itll be very difficult to convince them that what theyre experiencing isnt happening. Trying to argue with them may agitate and even enrage the person. Making them anxious could cause their hallucinations to get worse.
Instead, talk to the person gently and reassuringly. You might say something like, I understand that you see a dog in the corner of the room. Everything is going to be OK. Youre safe. You might even say that the dog must have left already.
Remember that the person cant control what theyre experiencing. Try to be as sympathetic as you can when you talk to them.
One approach that can help is to turn on all the lights in the room. Hallucinations are more likely to happen in dimly lit areas, and this can be caused by disease-related changes that affect the eyes.
Then, have the person really focus on what theyre seeing. That may reset their brain and help them see whats actually in front of them.
If the person doesnt have insight, try a distraction. Move them to a different room. Turn on the TV or play a game they like.
Try to keep your loved one as calm as possible. If they become very agitated or violent, call their doctor or 911.
Hallucinations And Rem Sleep Disorders In Parkinsons Disease
At timestamp 1:58 in this recording of Thrive: HAPS 2020 Caregiver Conference, you will find a one hour talk by neurologist Joohi Jimenez-Shahed, MD. In it she delves into what REM sleep behavior disorder is and is not, and the distinctions between hallucinations, delusions, and delirium. Managment options for RBD and hallucinations are included.
Also Check: Homeopathic Medicine For Parkinson Disease
Changes In Eye Movements
Subtle oculomotor changes can be seen in Parkinsons disease, with voluntary saccades particularly affected. Latency and velocity are preserved but amplitude is reduced, producing hypometric movements . Saccades to a remembered target are particularly impaired and show a multistep pattern . These are thought to arise from deficits in oculomotor pathways in the brainstem, cerebellum, basal ganglia and frontal lobes. In addition, patients with Parkinsons disease commonly show convergence insufficiency, that impacts on near activities and may lead to double vision on reading . Pronounced oculomotor abnormalities, when present, usually indicate an atypical Parkinsonian syndrome, but supranuclear vertical gaze impairment has rarely been reported in pathologically confirmed Parkinsons disease. Early decreased saccadic velocity, preservation of saccadic latency and paresis of vertical saccades favour a diagnosis of progressive supranuclear gaze palsy . Cerebellar type eye movement abnormalities, such as gaze-evoked nystagmus, abnormal vestibulo-ocular-reflex suppression, down-beat nystagmus, and excessive square wave jerks are more suggestive of multiple system atrophy .
Practical Tips For Caregivers Of People With Parkinson’s Psychosis
This 2-page tip sheet has bullet point suggestions for what to do if the person you care for experiences hallucination, delusions or confusion, or becomes agitated or aggressive. In addition, there are tips for how to best be prepared for a doctors appointment when you bring this behavior to the attention of your medical team.
Also Check: Parkinson’s Disease Fact Sheet
Management Of Dopaminergic Agents
Most PDD patients with VH use dopaminergic agents to ameliorate motor symptoms. However, these drugs may exacerbate VH in patients with PDD . This exacerbation is considered to be due to the overactivity of the mesolimbic system caused by an unnatural dopaminergic stimulation. Of course, other drugs, such as anticholinergics, antidepressants, and N-methyl-D-aspartate antagonists, can cause VH however, these are less frequently used, and most of them have a low risk . Thus, reducing the dose of dopaminergic agents ameliorates the symptoms of VH.
Not all patients require VH treatment since, in some mild cases, patients can understand that VH are unreal. In such cases, motor symptom treatment is prioritized therefore, dopaminergic agents can be continued. Goetz et al. evaluated the prognosis of PD patients who have VH with insight . Eighty-one percent of the patients progressed to VH without insight during 3-year follow-up . If VH cause delusions or violent behavior, doses of dopaminergic agents should be reduced. However, abruptly discontinuing them can cause severe rigidity and rhabdomyolysis, possibly leading to neuroleptic malignant syndrome thus, gradual tapering is recommended.
Figure 3.
Three-year follow-up result of PD patients who had VH with insight . Eighty-one percent of the patients progressed to VH without insight. Fifteen percent reduced PD medication and retained insight.
Demystifying Hallucinations Night Terrors And Dementia In Parkinsons
This two-hour webinar includes extensive discussion about hallucinations, delusions, illusions and other examples of Parkinsons psychosis in Parkinson’s. Presenters: Rohit Dhall, MD, MSPH and Vergilio Gerald H. Evidente, Director, Movement Disorders Center of Arizona in Scottsdale. Pay particular attention to Dr. Rohit Dhalls description of the causes of PD psychosis as well as treatment options and what to discuss with your movement disorder specialist. Dr. Evidente gives a clear description on differences in PD dementia, Alzheimer’s and other dementias.
Don’t Miss: Parkinson’s Phase 3 Trials
Hallucinations According To The Duration Of The Disease
We found that the prevalence of hallucinations of all types and of visual hallucinations in the 3 months preceding inclusion in the study increased with the duration of the disease. Moreover, the duration of Parkinsons disease was an independent predictor of visual hallucinations in the multivariate analysis. Other studies gave conflicting results on the relationship between hallucinations and disease duration. In a retrospective study of 100 patients, logistic regression analysis also showed an association between `psychosis and an increased duration of the disease . An association between the duration of the disease and the occurrence of hallucinations was also found by some investigators but not by others .
Table 1
Read Also: Diseases Similar To Parkinsons