How Can Occupational Therapy Help Parkinson’s Disease
For Parkinson’s disease, occupational therapy generally provides assessment, treatment, and recommendations in the following areas:
- Arm and hand therapy
- Driver evaluation and vehicle modification information
- Cooking and homemaking adaptations
- Ways to make the most of your energy
- Computer modifications
- Workplace or work equipment modifications
- Leisure skill development
What Is Parkinsons Disease
According to the Mayo Clinic, Parkinsons disease is a progressive nervous system disorder that affects movement.
What may start off as a mild tremor in one hand can progress into greater, more noticeable tremors. It often also evolves to include stiffness in the limbs, the slowing of movement, gait and balance problems, and difficulty talking.
An estimated 60,000 people are diagnosed with Parkinsons disease each year in the U.S. mostly people over the age of 50.
While theres no cure for Parkinsons, a variety of treatments have shown to slow the its progress, relieve symptoms, and make it easier to live, move and function.
Physical therapy is one of these essential treatments.
Promoting Physical Activity And Preventing Falls
Because PD is a chronic progressive disorder, it is probable that sustained exercise is necessary to maintain benefits. Indeed, follow-up data from a number of human exercise interventions have demonstrated a gradual return to baseline abilities after the supervised intervention is finished.7,25,38
Because weekly intervention with a physical therapist, throughout the entire course of PD, is neither realistic nor desirable, patients need to take responsibility for their physical activity and exercises. Methods have been developed, based on theories of behavior, for improving exercise habits. Strategies include exploration of the patient’s beliefs about exercise and barriers to regular exercise and discussing the possibility of looking at things differently to change beliefs and overcome barriers.4345 Together, the clinician and patient then establish reasonable goals that the patient thinks are attainable they build on those goals as exercise habits improve. Regular follow-up appointments also are important to monitor progression and provide support to the patient.
Read Also: Nursing Diagnosis For Parkinson’s Disease
What Other Services Does Physical Therapy Provide
Recommendations. A physical therapist can make recommendations for physical therapy at home, at an outpatient facility, or at a nursing or rehabilitation facility.
Work capacity evaluations. Many physical therapists can perform functional capacity evaluations to provide more information for disability claims based on physical performance. This functional capacity evaluation can be useful when the Social Security office denies disability to a person who is unable to work for an eight-hour day.
Defining The Strength Of The Recommendations
Judging the quality of evidence is only a steppingstone toward arriving at the strength of a CPG recommendation. The operational definitions for the quality of evidence are listed in , and rating of magnitude of benefits versus risk, harms, and cost is provided in . The strength of recommendation also considers the quality, quantity, and trade-off between the benefits and harms of a treatment, the magnitude of a treatmentâs effect, and whether there are data on critical outcomes. addresses how to link the assigned grade with the language of obligation of each recommendation.
Recommended Reading: Does Parkinson’s Affect Your Sense Of Taste
How Do I Find A Physiotherapist
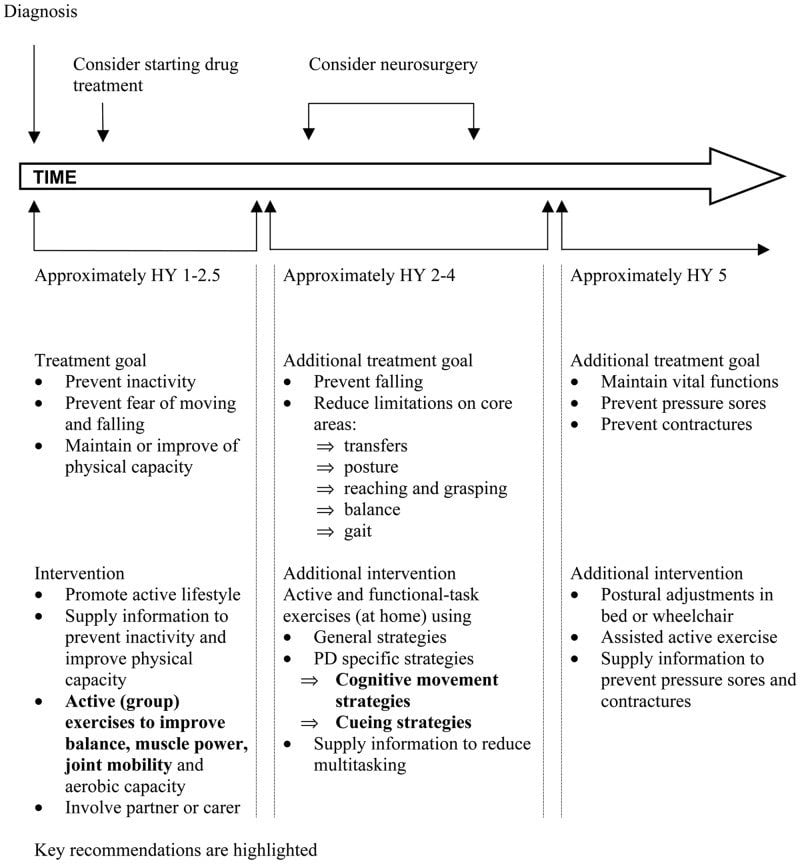
As Parkinsons is complex to manage, it is important to be seen by a physiotherapist who has experience of the condition. If you cannot find a physiotherapist with Parkinsons experience, you may want to share with the physiotherapist the European Physiotherapy Guideline for Parkinsons Disease and Pre-Assessment Information Form .
Referral procedures depend on the country in which you live in some countries physiotherapy is prescribed by a doctor but in others you can contact a physiotherapist direct. Depending on where you live, treatment may or may not be accessible through your countrys national health system. In some countries you need to be referred by your neurologist in order to get the cost of physiotherapy reimbursed.
Training and accreditation varies throughout Europe so you should always check the experience of anyone you consult and the likely costs before treatment starts.
Your national Parkinsons organisation may be able to provide information based on members experiences. See also, Other Parkinsons organisations.
Clinical Motor Cardinal Signs
A-/hypo-/bradykinesia: These terms are defined, collectively, as slowed voluntary movement. Separately, akinesia indicates the absence of voluntary movement, while hypokinesia means smaller movements, and bradykinesia refers to slowness of movement. They usually determine any impairment in fine motor movements, facial expression , monotonic and hypophonic speech with a reduction of speed, and general motion amplitude. This can have an important impact in functional skills like arm swinging when walking, raising from a chair, handwriting, and general gesturing .
This cardinal sign is one of the best that emerges from its origin of dysfunction, which is cited in this chapter . It has been determined especially by a characteristic involving the movement programming of the cerebral cortex, in particular the supplementary motor area .
2. Rest tremor : this sign is usually asymmetric, consisting of alternate contractions of agonist and antagonist muscles, including flexors, extensors, pronators, and supinators of the wrists and arms, resulting in the pill rolling movement of the hand. It has a medium frequency and tends to disappear with action. The legs, lower jaw, or head may also be involved, resulting in an adduction-abduction movement of the lower limbs and yes-yes or no-no motion in the head .
Also Check: Medications Contraindicated In Parkinson’s
The Basic Elements Of Exercising With Parkinsons
There are four core elements of exercise that are important for people with PD:
Including all four of these elements in your exercise regimen is ideal .
Aerobic activity or high-intensity exercise may be particularly important for Parkinsons and general health
High-intensity exercise has been formally studied in PD with impressive results. The Study in Parkinson Disease of Exercise Phase 2 enrolled 128 people with early PD, who were not yet on dopaminergic medication into three groups:
- a high-intensity treadmill exercise group, in which people exercised at 80-85% of their maximum heart rate
- a moderate-intensity treadmill exercise group, in which people exercised at 60-65% of their maximum heart rate
- a wait-list control group
After six months, the high-intensity group had essentially no change in their motor scores, whereas the control group had a three-point worsening of their motor scores.
Currently, the SPARX3 trial is enrolling participants and underway. This trial is similar to SPARX2, but with a goal of studying many more participants.
Forced exercise
Cognitive challenges in exercise
Balance Impairment And Falls In Parkinsons Disease
One of the most challenging symptoms of Parkinsons disease that fundamentally affects quality of life is balance impairment that can lead to falls.
Falls are one of the major causes of emergency room visits and hospitalizations for people with PD, so finding ways to prevent as many falls as possible is a high priority for people with PD. Thankfully there are things you can do to improve your stability and decrease the likelihood of falling, and well share some helpful tips and advice below.
Don’t Miss: Can Parkinson’s Cause Death
What Is Occupational Therapy
Occupational therapy can help people with Parkinson’s disease stay active in daily life. By improving your skills, showing you different ways to complete tasks, or introducing you to handy equipment, an occupational therapist can help you perform everyday activities with greater ease and satisfaction. An occupational therapist may also recommend making changes to your home or workplace to promote your independence.
How Can Physical Therapy Help Parkinson’s Disease
Physical therapy is an important part of a treatment plan for Parkinson’s disease. It aims to help individuals with Parkinson’s disease remain active and independent as long as possible. According to a recent meta-analysis, physical therapy significantly improves symptoms related to motor skills. The Parkinson’s Foundation states that increasing physical activity to 2.5 hours a week or more can help people with Parkinson’s disease maintain their quality of life.
Overall, physical therapy can help with the following:
- Increasing endurance
- Reducing pain
Because physical therapy improves motor skills and decreases pain, you can expect it to help with many of your regular activities, such as getting up from a chair, climbing stairs and getting into and out of a car.
Physical therapy can also improve other symptoms associated with Parkinson’s disease, such as depression, anxiety and fatigue. Lastly, it can help with other health issues that impair mobility, like joint pain.
Doctors recommend beginning an evidence-based physical therapy program as soon as possible. Exercise can induce neuroplasticity, or the brain’s ability to change in response to behavioral changes. When you begin physical therapy, your brain learns new ways to move and think. Exercise also helps brain cells stay healthy. In other words, physical therapy may slow the progression of Parkinson’s disease.
Recommended Reading: Gender Differences In Parkinson’s Disease
How To Exercise With Parkinsons
Whether you’re a first-time exerciser or a lifelong athlete, the key to working out with Parkinsons is to safely and regularly move your body in a variety of ways. Your fitness regimen should include these four main categories of exercise:
- Aerobic activity
- Balance, agility, and multi-task exercises
- Stretching
People with Parkinsons should strive to perform aerobic activity at least three times weekly and to complete exercises from the other categories two to three times each week.
In total, the Parkinsons Foundation suggests performing 150 minutes of moderate tovigorous exercise weekly.
To help you achieve this goal, try these helpful tips:
- Invest in a treadmill, elliptical, or exercise bike. This will make it convenient to perform aerobic exercise from your home, regardless of the weather.
- Obtain a set of light hand weights from a local exercise shop or thrift store. These can be used for a wide variety of strength training exercises.
- Follow along with one of the many online exercise classes on YouTube that are tailored to people with Parkinsons disease. The Parkinsons Foundation and the Davis Phinney Foundation offer many great online exercise videos.
- Connect with a workout buddy by finding a local Parkinsons support group associated with the American Parkinson Disease Association
Thanks For Signing Up

We are proud to have you as a part of our community. To ensure you receive the latest Parkinsons news, research updates and more, please check your email for a message from us. If you do not see our email, it may be in your spam folder. Just mark as not spam and you should receive our emails as expected.
Recommended Reading: Parkinson’s Disease Causes Death
Maintaining General Fitness Muscle Force Aerobic Capacity And An Upright Posture
When a person is found to have postural deformities or malalignment , the therapist should assess whether the condition is due to muscular, joint, or skeletal factors. If it is restricted to soft tissue factors, then I recommend visual feedback coupled with carefully designed strengthening or stretching programs. My observations suggest that lying flat in a supine or prone position for at least 30 minutes every day is advisable in order to maintain muscle length. When the malalignment cannot be volitionally corrected, the provision of orthoses or special seating and bedding may be considered. These interventions await validation with controlled clinical trials.
When Should I See A Physiotherapist
A physiotherapist can provide advice and suggest strategies to help you at any stage of your Parkinsons. If appropriate, a physiotherapist can provide treatment to prevent, stabilise or reduce any problems you experience relating to your general mobility and the way you function in your daily activities.
It is recommended that you talk with a physiotherapist as soon as possible after your diagnosis so that they can support you to self-manage your Parkinsons.
You should also talk with a physiotherapist if:
- you find regular exercise difficult or you are uncertain about what type of exercise to do
- you have queries on the frequency, intensity and safety aspects of exercising
- you experience walking problems, for example slowness, shuffling, hesitation or freezing
- you experience balance problems resulting in falls, nearly falling or fear of falling
- you find it difficult to get out of a chair, bed or car, or if turning in bed is difficult
- you experience pain, for example in your neck, back or shoulders.
You should always let your neurologist know if you are seeing a physiotherapist.
Read Also: What Medication Is Used To Treat Parkinson’s Disease
Common Physical Therapy Goals
As a physical therapy patient, you will work with a physical therapist to set and achieve realistic goals. A physical therapist will create a tailored, research-based exercise routine for you. They will first evaluate your current abilities and consider the areas you want to improve. The therapist will then design an exercise program to target those areas. Typically, physical therapy involves small achievements that build to a bigger goal.
Although your physical therapist will create an exercise plan based on your unique needs, shared goals for patients with Parkinson’s disease include:
Reach Out For Support
It can be challenging living with Parkinson’s disease, but you do not have to manage the symptoms alone. If you find yourself feeling discouraged or frustrated, share your feelings with others. Spend time with supportive friends and family members, or consider joining a support group. You might also speak with a counselor to address depression, anxiety or any other mental health issues you experience. By taking care of your mental and emotional health, you will be better positioned to reach your physical health goals.
Also Check: Walking With Parkinson’s Disease
Get Your Parkinsons Plan Of Attack
If youre looking for help in getting your daily Parkinsons exercise program off the ground, you can get your Parkinsons Plan of Attack Foundations Checklist here. Designed to help you wake up each day confident and excited to take control of your Parkinsons and live well, the checklist will remind you of the actions you can take each day to live with greater health, energy and joy.
How To Start Exercising If Youre Living With Parkinsons
Safety is key. The first thing you need to do is talk with your neurologist and primary care doctor to make sure that the exercise regimen that you embark upon is safe for you.
Next, ask for a referral for physical therapy. A physical therapist will be able to figure out what movement challenges you may have and design a program to help you improve. There are certain physical therapists with additional training in Parkinsons. Your physical therapist will work with you for your allotted sessions, and then can help you plan your ongoing exercise regimen that is tailored to you. You can contact the APDA National Rehabilitation Resource Center for Parkinsons Disease for help finding resources in your area.
Additionally, physical therapy can help counteract the tendency for people with PD to reduce the size of their movements. The Lee Silverman Voice Technique has designed a program called LSVT-BIG which trains participants to make big movements. You can search for an LSVT-trained professional near you.
Anyone starting out on an exercise program could benefit from APDAs Be Active & Beyond exercise guide which includes clear photos with simple instructions that are easy to follow, with exercises that address all levels of fitness.
Also Check: Does Parkinson’s Make You Forget Things
How Does Physical Therapy Help Parkinson’s Disease
Physical therapy cannot cure Parkinson’s disease, because at this time, neurological damage cannot be reversed. But therapy can help you compensate for the changes brought about by the condition. These “compensatory treatments,” as they’re called, include learning about new movement techniques, strategies, and equipment. A physical therapist can teach you exercises to strengthen and loosen muscles. Many of these exercises can be performed at home. The goal of physical therapy is to improve your independence and quality of life by improving movement and function and relieving pain.
Physical therapy can help with:
- Balance problems
- Immobility
- Weakness
Important note: Some physical therapists may apply diathermy to relieve muscle aches and pains. This could be dangerous to patients who have deep brain stimulators.
Physical Therapy And Occupational Therapy Goal Templates

Part of a therapy plan of care requires PTs and OTs to establish appropriate Physical Therapy and Occupational Therapy goals. As a PT, I work to create specific Physical Therapy goals for every patient based on their needs.
As a clinical instructor, I realized that therapy goal setting is not always a strong suit for my students or soon to be new therapy grads.
This lead to the creation of the Efficiency Formula and eventually the Therapy Goal Templates which you can find below.
My goal here is to introduce you to the Efficiency Formula so that you can produce a well written therapy goal that is defensible and appropriate for your patients. For over 80 examples of therapy goals broken down by body region, take a look at the Therapy Goal Templates Guide at the end of this article.
Don’t Miss: Parkinson Association Of Southwest Florida
Occupational Therapy For Early Onset Parkinsons
Occupational therapists are similar to physical therapists, but they focus on more specific goals related to functioning. In other words, occupational therapist help us function to the best of our ability. For people with early onset Parkinsons disease, routine tasks such as walking, running, standing up from a chair or moving into and out of bed can become difficult occupational therapists are trained to evaluate these kinds of difficulties and help the person and/or the environment adapt as needs and abilities change.
LEARN MORE