Improve Your General Fitness
Increasing your level of fitness will help you manage your weight and ensure your joints arent under any added pressure. You could try walking, swimming, dancing, cycling or aerobics its up to you.
Many of Parkinsons UKs local groups have physiotherapist-led exercise classes you can join. Visit our Local Support page or call our helpline on 0808 800 0303 to find one near you.
Q What Role Does Exercise Play In Pain Management In Pd
Dr. Fleisher: Exercise and physical therapy can be tremendously helpful in managing pain in PD, in addition to being important for overall disease management.4,8 Evidence suggests that exercise is the best option we have to alter the course of PD, and it has been shown to promote neuroplasticity and neurorestoration in PD.9,10 In addition, research suggests that exercise can activate both dopaminergic and non-dopaminergic inhibitory pain pathways, which may help to modulate the experience of pain in PD.10
Good exercise options include walking, swimming, dancing, and using a recumbent bike. In particular, forms of dance with smooth movements and those that encourage bigger steps appear to be especially beneficial in helping retrain the brain that the shuffling gait of PD is not the norm. Incredible work has come out of the Mark Morris Dance Company, in New York City, which has started a Dance for PD class that has spread throughout the country. In addition, yoga and tai chi can help with balance and core strength, which are critical for people with PD.
Importantly, there doesnt appear to be an upper limit for the benefits of exercise on the disease. I encourage patients to aim for at least 30 to 45 minutes a day at least 3 to 4 days a week. Patients who are sedentary should start with 5 minutes per day for a week, and then increase the duration each week.
These Symptoms Can Interfere With Daily Activities
Poston notes that the numbness in your hands could be so severe that it can make you unable to sense an object in your hand, which could result in difficulty eating, getting dressed, and holding objects. OBrien also says that people who suffer from these symptoms sometimes cant perform everyday tasks from writing or typing to picking up objects. If you find that youre experiencing numbness or tingling thats getting in the way of your daily activities, you should talk to your doctor immediately.
RELATED: For more health content delivered straight to your inbox, .
Recommended Reading: Does Alcohol Affect Parkinsons Disease
Don’t Miss: What Disease Is Similar To Parkinson’s
Risk Of Dislocation And Failed Fixation
The rigidity in Parkinson’s disease was historically cited as a reason to avoid hemiarthroplasty in intracapsular fractures. Coughlin and Templeton reported a 37% dislocation rate. The widespread uptake of Levodopa and other pharmacotherapy in the late 1970s and early 1980s may have contributed to the declining dislocation rates in subsequently published papers. In 1988, Staeheli et al. observed one dislocation in 50 implanted hemiarthroplasties performed through a variety of surgical approaches . Turcotte et al. in 1990 reported 5 dislocations in their study with 47 posterior-approach hemiarthroplasties. Nonetheless, the relative dislocation rate seems to have remained constant, with both Whittacker et al. and Hammer reporting 3 to 4 times higher rates than in non-Parkinson’s disease patients. Walker found that the re-operation rate was four times that in Parkinson’s disease patients with hip fractures . Similarly, Karadsheh et al. have recently reported higher rates of dislocation, failed fixation and revision surgery in their cohort of 141 Parkinson’s disease hip fracture patients compared with 282 patients matched for age, gender, ASA and operation type.
Faqs About Unlock Your Hip Flexors
Q: How is this different from other hip flexibility programs?
A: What makes Rick’s program unique is knowing how to unravel the tricky layers of tension with the very difficult psoas muscle in order to effectively loosen and train it.
Rick’s one-of-a-kind sequential flow is your surest path to looser, stronger and healthier hips.
Q: Why are you selling this so cheap? What’s the catch?
A: There is none. We’re so pleased with the number of our customers who have made the investment in this program and have enjoyed life-changing results.
Our aim is to make this available to as many guys as possible, firstly to welcome more people to our CriticalBench.com audience and secondly because we’re celebrating hitting a quarter million fans on Facebook.
Q: How long will it take me to do the program?
A: The program is designed to take between 10-15 minutes in total to complete.
We recommended adding the program as a daily practice to get the best results over a longer period of time. You may wish to add this program before or after your regular gym session or use it independently.
Q: How long until I see results?
A: Although everyone is different and results may vary, we know from experience how quickly it’s possible to feel and see a difference.
For some it may be as soon as their first session for others it may take a few sessions to really start seeing the benefits. Again, it depends on the body in question.
Q: Who is this program suitable for?
Q: Are the exercises hard to perform?
You May Like: Parkinson’s Disease And Eating Problems
Stay Informed On Your Parkinsons Journey
Our Every Victory Counts® manual gives people living with Parkinsons, their care partners and their family members the tools they need to take control of their own Parkinsons treatment through a proactive approach to self-care.
a powerful new print edition
Its jam-packed with up-to-date information about everything Parkinsons, plus an expanded worksheets and resources section to help you put what youve learned into action. Color coding and engaging graphics help guide you through the written material and point you to complementary videos, podcasts and other materials on the Every Victory Counts companion website. And, it is still free of charge thanks to the generosity of our sponsors.
Request your copy of the new Every Victory Counts manual by clicking the button below.
Diane Schuirman-Hagedorn has young-onset Parkinsons disease and works as a strategic communications consultant. You can email her .
Managing Pain In Parkinson’s
This article summarizes the incidence, types, and causes of reported pain in Parkinson’s Disease . A table of recommendations on how to involve patients with Parkinson’s in their own pain management is provided, along with approaches to pain assessment. Finally, there is a discussion of pain management principles in PD, including optimization of dopaminergic medications, use of analgesics, and innovative treatments for pain management .
Read Also: Judy Woodruff Parkinson’s Disease
When Hip Pain Turns Into Parkinsons Disease
Received a referral from an orthopod for home physical therapy to see a client who had fallen at home. She had both hips replaced in the last few years. The referral said Left Hip Pain. Eval and Treat. I figured I was walking into a situation of someone who had a painful left hippossible hip contusionprobably would need a home safety assessment, some ice/heat, massage, gentle stretching and move toward more aggressive strengthening and fall prevention strategies.
When I saw her, she could hardly move and was in a lot of pain from the most recent fall that occurred the night before. Pain not from her hip but instead her back and left rib area because of the latest fall. She could hardly move from the pain. I arranged for an x-ray for possible rib or spinal fractures. The x-ray did show left side rib fractures.
So, I prodded a little deeper. Reviewed her medications againhmmdepakote, clonazepam and about ten other meds including a narcotic for the pain. That explains itor does it?
It is very easy to get tunnel visioned into seeing what the referral script saysleft hip pain. But do I see the tree and miss the forest. A tree can tell you a lot, but step back and look at the forestyou may be surprised at the view.
This is one reason I love working as a home health physical therapist. I can make time to look at the tree and even step back and view the forest.
Loosening Your Hip Flexors Can Actually Be Easy With The Sequential Flow Method
Like unfolding a sheet or unpacking a parcel, opening up the muscles in your hips requires it to be done in the right order.
Try to release one muscle before another and you’ll add to your tightness. Getting it wrong really can make it worse.
It’s why so many people give up trying to fix the problem themselves and believe incorrectly that they have to live with the problem. But hoping the problem will go away by not exercising is just as damaging.
To explain in more detail about this flow, let me introduce you to leading Kinesiologist and Injury Specialist Rick Kaselj, MS.
Rick is “THE” guy fitness professionals go to when they want to learn about the latest techniques to help their own clients. He’s given over 352 live presentations to more than 8,152 health professionals in the US and Canada.
I first met Rick when he helped me fix a shoulder problem. He was one of the few injury specialists I met who helped athletes by focusing on getting them back to training, rather than avoiding workouts.
Rick showed me what so many other injury specialists hadn’t – how to work through the right sequence of techniques to unlock the tension and tightness in my muscles to properly solve the problem.
He’s the guy I turned to when my wife, Courtney, was struggling with pain and discomfort in her hips after the birth of our son Lincoln.
In the days and months following the birth, she experienced pain in her legs and discomfort when walking and sitting. She was struggling to sleep.
Read Also: Apps For Parkinson’s Patients
Pain Management In Patients With Parkinsons Disease: Challenges And Solutions
This review focuses on the diagnosis and management of Parkinson-related pain. It reviews the incidence and prevalence of PD, general pain and PD-related pain, the pathophysiological pathways of pain in PD, physiological pathways of pain relief, measurements of pain, clinical diagnosis of PD-related pain, and treatment strategies.
Functional Exercise For Chronic/persistent Pain
There are some simple exercises that you can try around the house to help:
- If you experience pain in your legs, keep them strong by practising standing up and sitting down in a chair.
- If your shoulders are aching, start by loosening them with some shoulder rolling actions, then by lifting an object that is slightly weighty from a shelf, and then replacing it. This increases the range of movement in your back, shoulders and arms, and then your strength.
Recommended Reading: Parkinson’s Dry Mouth Treatment
Akinetic Crisis And Pain
This type of pain may occur in the advanced stages of Parkinsons. Its brought on by akinetic crisis, which is a rare and sometimes dangerous complication of Parkinsons.
Akinetic crisis involves a worsening of Parkinsons symptoms, which can include severe rigidity, a complete loss of movement, fever and difficulty swallowing. People with Parkinsons who have akinetic crisis pain say that they feel pain in their muscles and joints, and experience headaches. Some people also experience whole-body pain.
This type of pain can be brought on if you abruptly stop taking Parkinsons medication, or if you develop an infection, both of which can cause Parkinsons symptoms to suddenly get worse. Akinetic crisis requires urgent medical help. If it looks like someone is experiencing akinetic crisis, call 999.
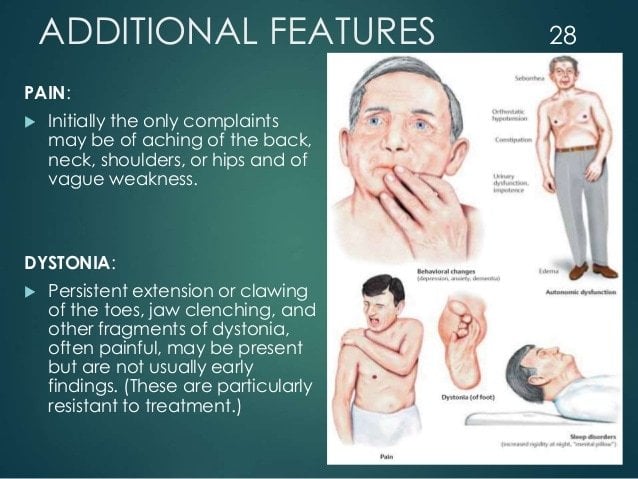
Second Type Of Leg Pain Is Caused By Dystonia

When related to levodopa, it usually occurs as a wearing off but can also occur at peak dose. In most cases this leg pain is unilateral and has direct correlation to medication intake. When pain is due to dystonia, it is more common in early morning. This type of leg pain is usually accompanied by toes curling and foot abnormally posturing.
Read Also: Parkinson’s Phase 3 Trials
Active Research Into Several Aspects Of Parkinsons Pain
Researchers are working to better understand the mechanisms behind pain in Parkinsons so that it can be more effectively addressed. They are looking for objective measurements, such as brain imaging, to diagnose and monitor pain, and to evaluate response to treatment. And, theyre investigating several drugs and deep brain stimulation for their potential benefits in treating Parkinsons disease pain.
Q What Is The Pain Experience In Pd And Does It Differ Between Genders
Dr. Fleisher: As with almost everything else in PD, the pain experience is highly individualized, and no 2 people, regardless of gender, will have the same symptoms. Female gender appears to be an independent risk factor for chronic pain in PD, even though PD is more common in men than in women.2 Pain intensity also is higher in women than in men with PD.1
There is a lot of interesting research examining the contributions of hormones to the greater prevalence of PD in men or, conversely, the lower prevalence in women.3 Once we better understand the roles of sex hormones in the pathophysiology of PD, we may better understand whether hormones also play a role in the higher incidence of with PD.
Also Check: Wearable Technology For Parkinson Disease
Before I Was Finally Sent To A Neurologist I:
- Saw numerous orthopedic specialists.
- Worked with 10 physical therapists.
- Had x-rays, a steroid injection and five rounds of prolotherapy .
- Had 10 MRIsboth hips, lower spine, shoulder, brain. Several body parts were scanned twice.
- Had two EMGs.
- Was tested multiple times for rheumatoid arthritis.
- Was advised to eat a gluten-free diet.
- Was hospitalized for a skin infection.
- Tried a chiropractor, acupuncture, rolfing, massage and a naturopath.
- Went from walking five miles a day to not being able to walk around the block.
I was and still am working full-time, and Im fortunate to work in a supportive office. I made it a priority not to take sick days, though I often had medical appointments multiple times a week and needed to recuperate from injections.
Causes Of Groin Pain That Comes From The Hip
Groin pain that originates in your hip can vary in how it feels. It can be either sharp or dull, and either sudden or gradual. Its type and severity will depend on its cause.
If your pain results from problems in your muscles, bones, tendons, or bursae, it will probably become worse when you move.
Learn what conditions originating in your hip might be causing your groin pain, and the best treatment options.
Read Also: Young Onset Parkinson’s Life Expectancy
Exercises For Parkinsons Disease
The chiropractor could also recommend exercises for the patient to try at home to maintain wellness in between visits. Aerobic exercises are performed to increase the delivery of oxygen within the body and assist neurotransmitters in keeping the heart, lungs, and nervous system healthy. Patients with PD are often found to benefit from exercises that feature changes in tempo, activity, or direction, as these promote the improvement of the patients ability to shift between activities or multitask. Rhythmic activities, such as dancing, skipping and cycling are also encouraged.
Walking, swimming, hiking, and aerobics are just a few activities that the patient could do both alone and with friends or a class. Anyone who engages in exercise should switch up their routine between rhythmic, repetitive movements and random practice exercise. These exercises are meant to relieve stiffness, reduce depression, and improve mobility, balance, posture, and gait. Natural symptom relief and quality of life improvements are the easiest treatments that a PD patient can try.7
Recommended Reading: Primidone For Parkinsons Disease
Strengthening Exercises Or Stretching May Be Helpful
Imagine that the spine is like a telephone pole or the mast of a sailboat. If the pole is not exactly upright, even a slight tilt requires a great force to keep it from tilting further and falling. In the human body, this means that the lower back muscles are under great stress. It also means that the tension on the back bones is much increased as well. This worsens whatever problems, like arthritis, that are already present. The same process applies to the neck, although the forces are less great. Strengthening exercises or stretching may be helpful. Almost everyone over the age of 60 has arthritis in their spine. Luckily most dont have pain from it, but those who do will have it worsened by the spine curvature caused by the PD.
PD patients also frequently have an aching discomfort in their muscles, particularly in the thighs and shoulders. I think this is due to the rigidity, or stiffness, that is part of the Parkinsons Disease syndrome, but Ive seen many patients with this pain and no apparent stiffness on examination, hence not explained. It is common and it often, but not always, responds to alterations of the usual Parkinsons Disease medications for movement. Exercise and stretching may be helpful as well and should always be tried first before increasing medications.
Pain is a challenge in PD. We cant measure it and often cannot find its cause. It is, however, often treatable, and reducing pain improves quality of life.
Recommended Reading: Games For Parkinson’s Patients
Arthroplasty In Patients With Parkinsons Disease
An interview with Lee M. Zuckerman, MD
An article in the January 2009 issue of the Journal of the AAOS reviews the evaluation and treatment of orthopaedic conditions in patients with Parkinsons disease . In an interview with AAOS Now, author Lee M. Zuckerman, MD, chief orthopaedic resident at SUNY Downstate Medical Center in Brooklyn, N.Y., focused on issues relating to total joint arthroplasty in Parkinsons patients.
AAOS Now: Is it true that the tremors experienced by a patient with Parkinsons will loosen an implanted prosthesis?
Dr. Zuckerman: No real data exists on this issue, or on whether a cemented or press-fit implant is better for patients with PD. Because patients with PD have tremors and rigidity, one theory was that the constant motion and muscular imbalance would prevent proper incorporation and increase the wear of the implant, leading to failure. In initial studies, patients were immobilized in an attempt to counteract this, but this resulted in worsening of the rigidity and tremor. Patients who are mobilized early actually do better and have similar short-term outcomes to patients without PD.
Parkinsons disease doesnt seem to be a real contraindication for TJA its more an issue of getting the patient mobilized to prevent the symptoms from worsening and proper patient selection.
AAOS Now: Is there any reason not to perform TJA on a patient with PD?
AAOS Now: Is one treatment better than another for hip fractures in patients with Parkinsons disease?