Do You Have An Off Story To Share
This post is the first in a series about what it means to be OFF. If you have a story about OFF and what youve done on your own and with your doctor that has helped you to minimize or navigate these periods, and youd like to share it with us, please send us an email at .
This post was written by the Davis Phinney Foundation.
This blog series is sponsored by Sunovion Pharmaceuticals Inc.
What Are On And Off Periods With Parkinsons Meds
While you might expect that taking a medication on a consistent schedule would guarantee your symptoms would be kept at bay, thats unfortunately not always the case with Parkinsons diseaseand thats the core of the on-off phenomenon, says Ling Pan, M.D., clinical assistant professor of neurology and neurosurgery at NYU Langone Health in New York, NY.
The on period is when the medication is doing its job to prevent tremors and other motor symptoms, explains Dr. Hui. Patients will often feel better fairly soon after taking their doseeven within half an hour, she says. Its almost like a light switch is being switched on, and they can move a lot easier.
That said, Dr. Hui explains, the effect can wear off over several hoursand thats when you hit that off period. When you first start taking the drug, though, its normal to experience a honeymoon period, she says. It may work all day, and you feel great, but overtime as the disease progresses, the medication doesnt less as long, and off-time creeps in slowly and then becomes more noticeable and more regular overtime. Typically, thats when folks with Parkinsons start to cycle between those on and off periods.
Can Parkinsons Disease Be Prevented
Unfortunately, no. Parkinsons disease is long-term disease that worsens over time. Although there is no way to prevent or cure the disease , medications may significantly relieve your symptoms. In some patients especially those with later-stage disease, surgery to improve symptoms may be an option.
You May Like: How Long Does A Parkinson’s Patient Live
How Does The Levodopa Drug Help In Managing The Symptoms Of Parkinsons Disease
In levodopa drug therapy the patient is given the drug which gets synthesized into dopamine in brain. Levodopa is considered to be the most important drug for the management of Parkinsons disease. This drug is generally given in combination with carbidopa in order to prevent nausea, caused by levodopa. It also enhances the effect of levodopa.
How Is Parkinsons Disease Treated
There is no cure for Parkinsons disease. However, medications and other treatments can help relieve some of your symptoms. Exercise can help your Parkinsons symptoms significantly. In addition, physical therapy, occupational therapy and speech-language therapy can help with walking and balance problems, eating and swallowing challenges and speech problems. Surgery is an option for some patients.
Recommended Reading: Vascular Parkinsonism And Cognitive Impairment
What Lifestyle Changes Can I Make To Ease Parkinsons Symptoms
Exercise: Exercise helps improve muscle strength, balance, coordination, flexibility, and tremor. It is also strongly believed to improve memory, thinking and reduce the risk of falls and decrease anxiety and depression. One study in persons with Parkinsons disease showed that 2.5 hours of exercise per week resulted in improved ability to move and a slower decline in quality of life compared to those who didnt exercise or didnt start until later in the course of their disease. Some exercises to consider include strengthening or resistance training, stretching exercises or aerobics . All types of exercise are helpful.
Eat a healthy, balanced diet: This is not only good for your general health but can ease some of the non-movement related symptoms of Parkinsons, such as constipation. Eating foods high in fiber in particular can relieve constipation. The Mediterranean diet is one example of a healthy diet.
Preventing falls and maintaining balance: Falls are a frequent complication of Parkinson’s. While you can do many things to reduce your risk of falling, the two most important are: 1) to work with your doctor to ensure that your treatments whether medicines or deep brain stimulation are optimal and 2) to consult with a physical therapist who can assess your walking and balance. The physical therapist is the expert when it comes to recommending assistive devices or exercise to improve safety and preventing falls.
How To Manage Parkinsons Disease After It Is Diagnosed
Along with the medication so prescribed by the doctor, it is extremely important to bring some form of lifestyle changes in order to manage Parkinsons disease. They include-
Activity: As mentioned earlier Parkinsons disease affects the patients motor abilities, it is thus important to keep the body fit by indulging into exercise regularly. The patient may do any form of exercise which he may like every day to keep the body moving. This does not let the body parts to be stiff and also slows down the progression of the disease.
Additional Help: The caregivers and well-wishers should make attempts to make the environment safe for the patient with Parkinsons disease. Modifying the environment like installing grab bars in washroom and removing obstacles which may hamper movement of the patient is important.
Diet: Having nutritious food is important for patients with Parkinsons disease. It is seen to be beneficial to have right amount of nutrients in order to manage the symptoms of Parkinsons disease. The patient should also discuss with the doctor the food to avoid so that they do not interfere with the working of the medicines, especially levodopa.
Also Check: Computer Mouse For Parkinson’s
How The Parkinson’s On
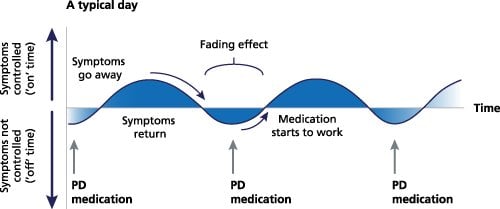
Ideally, when you take doses of a medication like levodopa on a regular schedule, you shouldn’t notice much of a difference in your symptoms between doses. In other words, your symptoms should remain relatively constant over time, regardless of when you last took your medication.
However, when the on-off phenomenon starts in Parkinson’s disease, you’ll feel better as a new dose of your medication starts to take effect, and worse before you’re due for another dose. Eventually, the duration of on states becomes shorter and the wearing off happens sooner .
Some experts have described the “on” period as akin to switching on a light, and the “off” period as the lights going off.
In an “on” state, the person with Parkinson’s disease may feel energetic and able to move around more easily. However, in an “off” state, the person may become very stiff, slow, and may even be unable to move at all for a few minutes. A person may also have difficulty speaking, and you may notice him or her slurring their words. As you can imagine, the “off” state can be quite uncomfortable.
What Causes On/off Episodes In Parkinson’s Disease
On/off episodes, also known as off time, typically happen more often as Parkinson’s disease progresses, and levodopa becomes less effective.
Carbidopa/levodopa is considered the gold standard in Parkinson’s disease treatment, meaning it’s the most effective for treating motor symptoms, such as tremor, rigidity, and bradykinesia . Levodopa works by crossing the blood-brain barrier and converting into dopamine, low levels of which are believed to be the cause of Parkinson’s symptoms. Adding carbidopa to levodopa helps prevent levodopa from breaking down before it crosses into the brain, which helps reduce side effects like nausea and vomiting.
Some people who have Parkinsons start taking levodopa at around three doses per day. If you start experiencing off episodes, your doctor may increase your dose to four or more times per day.
Off time is common: According to patient surveys, around half of patients who take levodopa report experiencing wearing off periods. Of those patients, 25% experience it 3 to 6 hours per day, and 52% have symptoms for 1 to 3 hours a day.
Don’t Miss: What Are Some Signs Of Parkinson’s Disease
What To Expect After Dbs
Surgery to implant the leads generally entails an overnight stay, while the IPG is usually implanted as same-day surgery. During recovery, your surgeon will talk to you about caring for your wounds, when you can shower, and any activity restrictions. Its usually recommended that any heavy lifting be avoided for a few weeks.
After another two to four weeks, youll return to have your device programmed. This process will continue for several weeks to ensure the stimulation settings are optimal to control your symptoms. During these visits, you will be shown how to turn the device on and off with the handheld device and check the battery level.
Once the programming has been completed, you will have regular follow-up visits to check and adjust the stimulation to maintain the most benefit for your symptoms.
Why Do Motor Fluctuations Happen
As Parkinsons disease progresses, it is common for more dopamine-producing brain cells to die, causing the benefits from Parkinsons medications to not last as long as they did before. The brain eventually reaches a point where it stops producing dopamine in large amounts and therefore must rely on medicine to replace dopamine. Researchers think this happens for two reasons:
- As Parkinson’s progresses, cells become less able to store dopamine. When this occurs, the cells are unable to release dopamine without medications, such as levodopa. When the dose fades, 60-90 minutes after taking it, there is no more levodopa for the cells to use, resulting in lower dopamine levels and a worsening of symptoms .
- The cells in your brain become more sensitive to both higher and lower concentrations of levodopa. There is a higher likelihood of experiencing off times when levodopa levels are too low and a higher likelihood of experiencing dyskinesis when levodopa levels are too high.
As a result, your doctor may advise you increase your medication doses to achieve optimal control of motor symptoms, such as tremor, slowness and rigidity. The goal is to maximize symptom control without increasing side effects.
Read Also: What Is Drug Induced Parkinson’s Disease
Parkinson’s Disease Symptoms Everyone Should Know
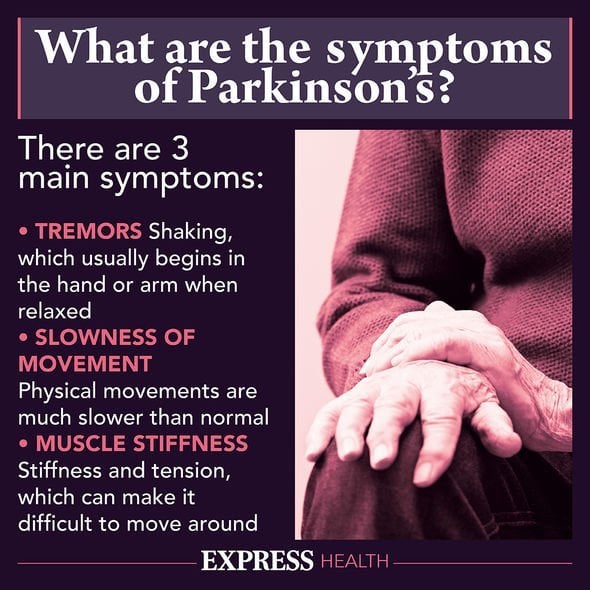
Parkinsons disease symptoms can include tremor and trouble with movement, along with emotional and cognitive changes.
Parkinson’s disease symptoms can vary significantly from person to person. Some people may have range of motor symptoms, like tremor, stiffness, and slow movements. Others may also experience the non-motor symptoms of Parkinson’s disease, such as anxiety, cognitive changes, and loss of smell.
It has to do with a chemical messenger known as dopamine, which plays a role in the brain’s ability to control movement, coordination, and emotional responses. In Parkinson’s disease, the brain cells that produce dopamine either stop doing their job or they die out, resulting in both motor and non-motor symptoms. It’s not always easy to tell if someone you care about has Parkinson’s disease. Let’s take a closer look at the symptoms of the disease and signs that someone should make an appointment with their doctor.
What Makes Pd Hard To Predict
Parkinsonâs comes with two main buckets of possible symptoms. One affects your ability to move and leads to motor issues like tremors and rigid muscles. The other bucket has non-motor symptoms, like pain, loss of smell, and dementia.
You may not get all the symptoms. And you canât predict how bad theyâll be, or how fast theyâll get worse. One person may have slight tremors but severe dementia. Another might have major tremors but no issues with thinking or memory. And someone else may have severe symptoms all around.
On top of that, the drugs that treat Parkinsonâs work better for some people than others. All that adds up to a disease thatâs very hard to predict.
You May Like: Loss Of Balance Parkinson Disease
How Do I Prevent Falls From Common Hazards
- Floors: Remove all loose wires, cords, and throw rugs. Minimize clutter. Make sure rugs are anchored and smooth. Keep furniture in its usual place.
- Bathroom: Install grab bars and non-skid tape in the tub or shower. Use non-skid bath mats on the floor or install wall-to-wall carpeting.
- Lighting: Make sure halls, stairways, and entrances are well-lit. Install a night light in your bathroom or hallway and staircase. Turn lights on if you get up in the middle of the night. Make sure lamps or light switches are within reach of the bed if you have to get up during the night.
- Kitchen: Install non-skid rubber mats near the sink and stove. Clean spills immediately.
- Stairs: Make sure treads, rails, and rugs are secure. Install a rail on both sides of the stairs. If stairs are a threat, it might be helpful to arrange most of your activities on the lower level to reduce the number of times you must climb the stairs.
- Entrances and doorways: Install metal handles on the walls adjacent to the doorknobs of all doors to make it more secure as you travel through the doorway.
What Helps On/off Episodes
There are a few different steps you can consider taking to increase your symptom-free hours during the day.
Change the dosage or timing of your carbidopa/levodopa: Taking your medication at different times, or increasing your dose, may help reduce your off time.
Try a different medication: Your doctor may suggest another medication to add to your regimen, or a new carbidopa/levodopa option, to help reduce off episodes. You may also consider newer treatments for “off” time. For example, an inhaled levodopa powder for off episodes was approved by the FDA in 2018.
Adjust your diet: Because levodopa is a protein building block, it competes for absorption in the brain with other proteins. It’s best not to eat a high-protein meal before taking your medication. For example, you may save fish, meat, and cheese for dinner and eat more carbs and vegetables during the day.
Consider a clinical trial: If you’re interested, there are also several treatments in development for “off” time in Parkinson’s disease.
Participating in clinical trials helps create the treatments of tomorrow. Start your search for a local Parkinsons disease clinical trial opportunity.
Recommended Reading: Parkinson’s Disease Funding Opportunities
Current Approaches To The Treatment Of Off Episodes In Parkinsons Disease
Olivier RascolResearch Network Departments of Clinical Pharmacology and Neuroscience, Toulouse University Hospital, Toulouse, France
The poor efficacy of levodopa in treating the OFF phenomenon in PD is caused by several pharmacokinetic issues including poor bioavailability, being only absorbed through the jejunum. Levodopa tablets can remain in the stomach for several hours due to issues with gut emptying, delaying the drug reaching the brain. In addition, levodopa has a short plasma elimination half-life of 60â90 minutes.33,34 The pulsatility of levodopa plasma levels dysregulates the cerebral and synaptic mechanism, generating post-synaptic abnormal plasticity and abnormal motor function.35,36 Objectives in PD treatment development have therefore been to find faster-acting drugs, to improve the bioavailability of levodopa, and to stimulate dopamine receptors in a more continuous manner. Approaches include:37
- alternate formulations of levodopa with longer duration of action
- inhibitors of dopa decarboxylation at the periphery to increase availability of levodopa in the central nervous system
- inhibiting catechol-O-methyltransferase to increase availability of levodopa in the central nervous system
- inhibiting monoamine oxidase B to reduce dopamine elimination
- increasing dopamine release and
- dopamine agonists to mimic dopamine.
People With Pd May Not:
- Discuss the timing of their motor symptoms or realize that motor symptoms occur during OFF periods
- Be aware that non-motor symptoms could be linked to OFF periods
- Be aware that there may be variations during the day as symptoms may improve and then re-emerge
In addition, patients may try to be at their best for office visits.
Don’t Miss: How Do You Get Parkinson Disease Symptoms
Off Periods For Me Are Best Defined As Not Knowingwhat Is Going To Happen
Israel R., Living with Parkinson’s Since 2007
Lynn H., Living with Parkinson’s Since 2010
Michael B., Living with Parkinson’s Since 2011
Brenda V., Living with Parkinson’s Since 2012
Steven D., Living with Parkinson’s Since 2005
Gary R., Living with Parkinson’s Since 2008
Steven D., Living with Parkinson’s Since 2005
Israel R., Living with Parkinson’s Since 2007
Return Of Symptoms: Off Periods
Many people with Parkinsons disease fluctuate between periods in which symptoms are controlled and periods in which they return.3,6 This is commonly referred to as ON and OFF periods. The progression of Parkinson’s disease contributes to the return of symptoms and this can occur despite optimized treatment.7,8
Also Check: Best Parkinson’s Doctors In Nj
Help Your Patients Uncover The Troublesome Symptoms Of Off Periods9
Both physicians and patients agree: OFF periods can be one of the most difficult aspects of Parkinsons disease. Its understood that recognizing the symptoms of OFF periods is challenging because of a variety of reasons, including interpatient symptom variability and reliance on patient reporting.9
People with OFF periods may not discuss their symptoms or communicate the impact of the symptoms to their healthcare provider as they may be unaware that the changes they are experiencing are a result of OFF periods. Because patients may not recognize the more subtle changes they are experiencing as symptoms of OFF periods, enhancing communication around the full spectrum of symptoms is important.9
What Is The On/off Phenomenon In Parkinsons
The ON/OFF phenomenon in PD happens when someone experiences flares of symptoms between regularly scheduled doses of levodopa.
During an ON episode, the levodopa is working well and symptoms improve. During an OFF episode, the levodopa isnt working and symptoms return or get worse.
A 2018 review found that 25 to 50 percent of people with PD developed OFF episodes within 2 years of beginning treatment with levodopa. Within 10 years of starting treatment, most people with PD had OFF episodes.
OFF episodes can affect different people in different ways. They may follow a predictable pattern or occur unpredictably. They may set in suddenly or gradually.
The researchers behind a
Read Also: Parkinson’s And Similar Diseases