Signs And Symptoms Of Dysautonomia
Dysautonomia refers to a disturbance of the autonomic nervous system, the nerve pathways which regulate unconscious bodily functions including heart rate, blood pressure, digestion, salivation, perspiration, micturition , and some sexual functions. Patients with dysautonomia experience symptoms of fainting or dizziness when changing to an upright position . The lightheadedness results from a decrease in blood pressure upon rising which decreases the amount of blood working against gravity to reach the brain. When a patient collapses to the floor, the amount of blood reaching the brain increases as the blood pressure rises, and the patient regains consciousness. Other typical symptoms of autonomic nervous system dysfunction are constipation, impotence in males, and loss of bladder or bowel control leading to incontinence or constipation. Some patients experience abnormal sweating and develop reddish-blue discoloration of the skin known as the cold hand or cold foot sign. MSA patients also frequently snore, have longer than normal pauses in breathing during sleep , and exhibit combative behavior while asleep, known as REM sleep behavioral disorder .
Avoidance Of Postural Hypotension
One particularly serious problem, the drop in blood pressure upon standing up ” rel=”nofollow”> fainting and thus injury from falling), often responds to fludrocortisone, a synthetic mineralocorticoid. Another common drug treatment is the alpha-agonistmidodrine.
Non-drug treatments include “head-up tilt” , salt tablets or increasing salt in the diet, generous intake of fluids, and pressure stockings. Avoidance of triggers of low blood pressure, such as hot weather, alcohol, and dehydration, are crucial. The patient can be taught to move and transfer from sitting to standing slowly to decrease risk of falls and limit the effect of postural hypotension. Instruction in ankle pumping helps to return blood in the legs to the systemic circulation. Other preventative measures are raising the head of the bed by 8 in , and the use of compression stockings and abdominal binders.
Distinguishing Between Parkinsons Disease And Msa
It can be challenging to differentiate between PD and MSA. Early on in the course of the illness, MSA can manifest with mild parkinsonism and autonomic dysfunction. These clinical features are also often present in PD. Furthermore, in the beginning, the parkinsonism of MSA can be minimally responsive to levodopa, complicating the distinction between the diseases even more. Both diseases have a high rate of REM behavior sleep disorder . Therefore, it is very common for someone with MSA to initially receive a diagnosis of PD.
Over time, clinical features may develop that are not as common in PD and may suggest MSA as a diagnosis. However, although these features are not as common in PD, they can still be present in PD, so diagnosis remains difficult. The more features that are uncommon in PD that are present, the more the clinical situation warrants the consideration of MSA as the diagnosis. These red flags include:
- Poor levodopa response
- Facial dystonia from levodopa
- Sleep-disordered breathing such as obstructive sleep apnea
- Inspiratory stridor during daytime or sleep
- Jerky tremor when performing an action
- Axial postural abnormalities
- Cold, darkened/reddened hands and feet
- Severe difficulty with speech
- Severe difficulty with swallowing
- Pseudobulbar affect the Involuntary and uncontrollable reactions of laughing or crying that are out of proportion to the cause of the emotional response
You May Like: Idiopathic Parkinson’s Disease Life Expectancy
Characterization Of Structural Connectivity Differences
In order to test for intergroup differences in interregional NOS between PD, MSA, and HC, we used TFNBS. This approach combines threshold-free cluster enhancement, a method frequently used in voxel-wise statistical inference, and network-based statistics, commonly used for statistical analysis of brain graphs. Initially, the symmetric 18×18 connectivity matrices M of all individual subjects underwent group testing, where an F statistic was calculated for each entry i, j using the general linear model, producing a group 18×18 raw F statistic matrix Mstat. With TFNBS, the raw statistic value of each Mstat edge is replaced by its TFNBS score. Concretely, this score is determined by the heights of its neighboring edges and by the strength of the statistical effect thus, the final TFNBS scores are influenced by how topologically clustered these effects are. Finally, a p value is ascribed to each entry in the TFNBS-enhanced matrix through permutation testing. Further description of this method can be found in Baggio et al. .
Gender was included in the intergroup connectivity analyses as a covariate of no interest, and control of the false discovery rate to 5% was used to correct for multiple testing across the connectome. Post-hoc comparisons were then tested in the significant connections found with TFNBS. Connectivity Fig. was drawn using Surf Ice .
Characteristics Of Atypical Msa: Parkinsons Disease Mimics
Case illustration
A 67-year-old female : presented with a 1-year history of worsening dexterity of her left hand. Examination revealed an asymmetrical tremor of the hand at rest with cogwheel rigidity and bradykinesia. Her symptoms and signs improved with levodopa therapy . Over the next 3 years, she developed motor fluctuations, generalized peak-dose dyskinesia, worsening dysarthria, urinary frequency and constipation. She also reported intermittent mild non-threatening visual hallucinations. Orofacial dystonia and urinary incontinence then became more intrusive. She died aged 75. The final clinical diagnosis was Parkinsons disease. Autopsy confirmed the pathological diagnosis of MSA . There were frequent depositions of neuritic plaques but no neurofibrillary tangles were found in the brain. Key clinical features of all Parkinsons disease mimics are provided in Supplementary Table 2.
Atypical MSA versus typical MSA or Parkinsons disease
Red flag features in atypical MSA versus typical MSA or Parkinsons disease
| Pathological diagnosis . |
|---|
You May Like: Is There Pain With Parkinson’s
Multiple System Atrophy With Orthostatic Hypotension
Some people experience multiple system atrophy with orthostatic hypotension, also called Shy-Drager syndrome. This is a rare type of hypotension that leads to progressive decline of the autonomic nervous system, which controls involuntary functions, such as blood pressure, breathing, digestion, and heart rate. Parts of the brain that control these functions progressively malfunction.
Researchers have not discovered what causes nervous system damage in patients with this type of hypotension.
This type of hypotension is characterized by severe orthostatic hypotension along with very high blood pressure when lying down. Additional symptoms may include slowed movements, decreased coordination, problems with speech, muscle tremors, and urinary incontinence.
There is currently no cure for this type of hypotension. But there are effective treatments to manage symptoms. Most patients die from the condition seven to 10 years after they are diagnosed.
Signs And Symptoms Of Cerebellar Dysfunction
MSA-C is characterized by poor coordination and progressive loss of balance . In addition, patients with MSA-C may have tremor with action, which is different from the resting tremor seen in typical Parkinson’s disease. This tremor is present during activities, such as reaching for objects or eating, and can be elicited on examination by the finger-to-nose maneuver. Other features include slurring of speech, difficulty with swallowing, and progressive weakness. The first symptom is usually mild incoordination in the hands and legs, which eventually progresses to loss of balance requiring a walker or a wheelchair.
Also Check: Loss Of Smell And Parkinson’s
Characteristics Of Atypical Msa: Psp Mimic
Case illustration
A 54-year old female developed dragging of her left leg and frequent falls. She also complained of urinary frequency and urgency that progressed to incontinence. She was initially diagnosed as having Parkinsons disease. She then developed double vision on looking up and down at age 58, and a vertical supranuclear gaze palsy and apraxia of eyelid opening was observed at age 60. The clinical diagnosis was revised to PSP. Throughout the course of her illness, she was reported as having antecollis, contractures of her feet and a jerky myoclonic postural and action tremor of the hands. Emotional lability and pathological laughter were also prominent features in her last 3 years of life. She died 9 years after onset of her first symptoms. At autopsy, a pathological diagnosis of MSA was made. Tau immunohistochemistry showed moderate numbers of neurofibrillary tangles and neuropil threads in the transentorhinal cortex . There was no amyloid- pathology in the brain. Key clinical features of all PSP mimics are described in Supplementary Table 2.
Atypical MSA versus typical MSA or PSP
Patients And Sample Collection
Healthy controls and patients with probable MSA-C, probable MSA-P, and PD who were diagnosed at Hokkaido University Hospital, Obihiro Kosei General Hospital, and Kushiro Rosai Hospital were enrolled in this study. Diagnosis of MSA-C and MSA-P was made on the basis of the second consensus statement on the diagnosis of MSA . Patient background data at the time of sample collection were retrospectively obtained from medical records. Clinical parameters included scores on the Scale for the Assessment and Rating of Ataxia , Barthel Index , the Unified Multiple System Atrophy Rating Scale , and the Unified Parkinsons Disease Rating Scale .
Patients with concurrent malignant tumors, psychiatric disorders, collagen diseases, endocrine diseases, or infections were excluded from our study, since these conditions are previously reported to alter the expression profile of some miRNAs. For the same reason, healthy controls with no known neurological disease or comorbidities were selected. In the MSA-C and MSA-P groups, blood samples that had been obtained at the time of or prior to the diagnosis of probable MSA were used for analyses.
In microarray analysis, plasma samples of 11 patients with probable MSA and of six age- and sex-matched healthy controls fulfilling the criteria listed above were used. In RT-qPCR, plasma samples were obtained from 31 patients with probable MSA-C, 30 with probable MSA-P, and 28 with PD, as well as from 28 healthy controls.
You May Like: Movie Stars With Parkinson’s Disease
A New Blood Test That Might Help With Diagnosis
Researchers recently discovered a blood test that can detect a specific protein found in the blood of Parkinsons patients but not MSA patients. The protein, known as alpha-synuclein, is produced in nerve cells in the brain and can be detected in the blood. It is one of the proteins that accumulate and damages the brains of people with both MSA and Parkinsons. However, the protein collects in different cells in the brain, depending on which disease it is.7
Support For People With Multiple System Atrophy
If you have MSA and are finding coping with day-to-day life difficult, your doctor or nurse can refer you to a social worker.
They can carry out an assessment and recommend the help you need. For example, you may need:
- care attendants who can help with everyday tasks such as housework, dressing and washing
- meals on wheels your local council may be able to offer financial help for this check your eligibility for getting meals at home
- benefits you may be eligible for a number of benefits, such as Attendance Allowance and Personal Independence Payment
- home adaptations to make moving around at home easier and ensure your home environment is as comfortable as possible
Find out more about care and support needs assessments.
Also Check: Parkinson’s Disease And Vision Problems
What Is Multiple System Atrophy
Multiple system atrophy is a progressive neurodegenerative disorder characterized by a combination of symptoms that affect both the autonomic nervous system and movement. The symptoms reflect the progressive loss of function and death of different types of nerve cells in the brain and spinal cord.
Symptoms of autonomic failure that may be seen in MSA include fainting spells and problems with heart rate, erectile dysfunction, and bladder control. Motor impairments may include tremor, rigidity, and/or loss of muscle coordination as well as difficulties with speech and gait . Some of these features are similar to those seen in Parkinsons disease, and early in the disease course it often may be difficult to distinguish these disorders.
MSA is a rare disease, affecting potentially 15,000 to 50,000 Americans, including men and women and all racial groups. Symptoms tend to appear in a persons 50s and advance rapidly over the course of 5 to 10 years, with progressive loss of motor function and eventual confinement to bed. People with MSA often develop pneumonia in the later stages of the disease and may suddenly die from cardiac or respiratory issues.
While some of the symptoms of MSA can be treated with medications, currently there are no drugs that are able to slow disease progression and there is no cure.
MSA includes disorders that historically had been referred to as Shy-Drager syndrome, olivopontocerebellar atrophy, and striatonigral degeneration.
Dti And Volumetry Data Of Subcortical Structures
Measures of mean FA and MD were calculated for each subcortical ROI to evaluate the microstructural diffusion properties of the 18 subcortical structures. Complementarily, the FreeSurfer volume-based stream was used to extract the volume of each ROI, which is often used as a marker of atrophy. Gender was included as a covariate in all analyses. Intracranial volume was also used as a covariate in the volumetric comparisons.
Don’t Miss: Does Sam Waterston Have Parkinson
How Is It Treated
Currently, there are no treatments to delay the progressive neurodegeneration of MSA, and there is no cure. There are treatments to help people cope with the symptoms of MSA.
In some individuals, levodopa may improve motor function however, the benefit may not continue as the disease progresses.
The fainting and lightheadedness from orthostatic hypotension may be treated with simple interventions such as wearing compression stockings, adding extra salt and/or water to the diet, and avoiding heavy meals. The drugs fludrocortisone and midodrine sometimes are prescribed. In 2014, the U.S. Food and Drug Administration approved the medication droxidopa for the treatment of orthostatic hypotension seen in MSA. Dihydroxyphenylserine helps to replace chemical signals called neurotransmitters which are decreased in the autonomic nervous system in MSA. Some medications used to treat orthostatic hypotension can be associated with high blood pressure when lying down, so affected individuals may be advised to sleep with the head of the bed tilted up.
Bladder control problems are treated according to the nature of the problem. Anticholinergic drugs, such as oxybutynin or tolteridine, may help reduce the sudden urge to urinate.
Fixed abnormal muscle postures may be controlled with injections of botulinum toxin.
Sleep problems such as REM sleep behavior disorder can be treated with medicines including clonazepam, melatonin, or some antidepressants.
Low Blood Pressure When Standing Up
Someone with MSA will often feel lightheaded, dizzy and faint after standing up. This is known as postural hypotension and is caused by a drop in blood pressure when you stand up or suddenly change position.
When you stand up after lying down, your blood vessels usually narrow quickly and your heart rate increases slightly to prevent your blood pressure from dropping and decreasing blood flow to your brain.
This function is controlled by the autonomic nervous system. But with MSA, this system does not work properly, so the control is lost.
You May Like: Vascular Parkinsonism And Cognitive Impairment
What Causes Msa And Parkinsons
Neither disease has a clearly understood cause, but Parkinsons seems to have more of a genetic component than MSA, meaning it runs in families. MSA almost always occurs sporadically, meaning randomly, without any recognizable pattern. Both diseases seem to have some connection with environmental contaminants.3
One key difference is that the nerve destruction in Parkinsons tends to occur in the areas of the brain that control movement, whereas MSA affects whats called the autonomic nervous system. This is the system that controls the automatic functions of the body, like blood pressure, breathing, bladder function, and muscle control.5
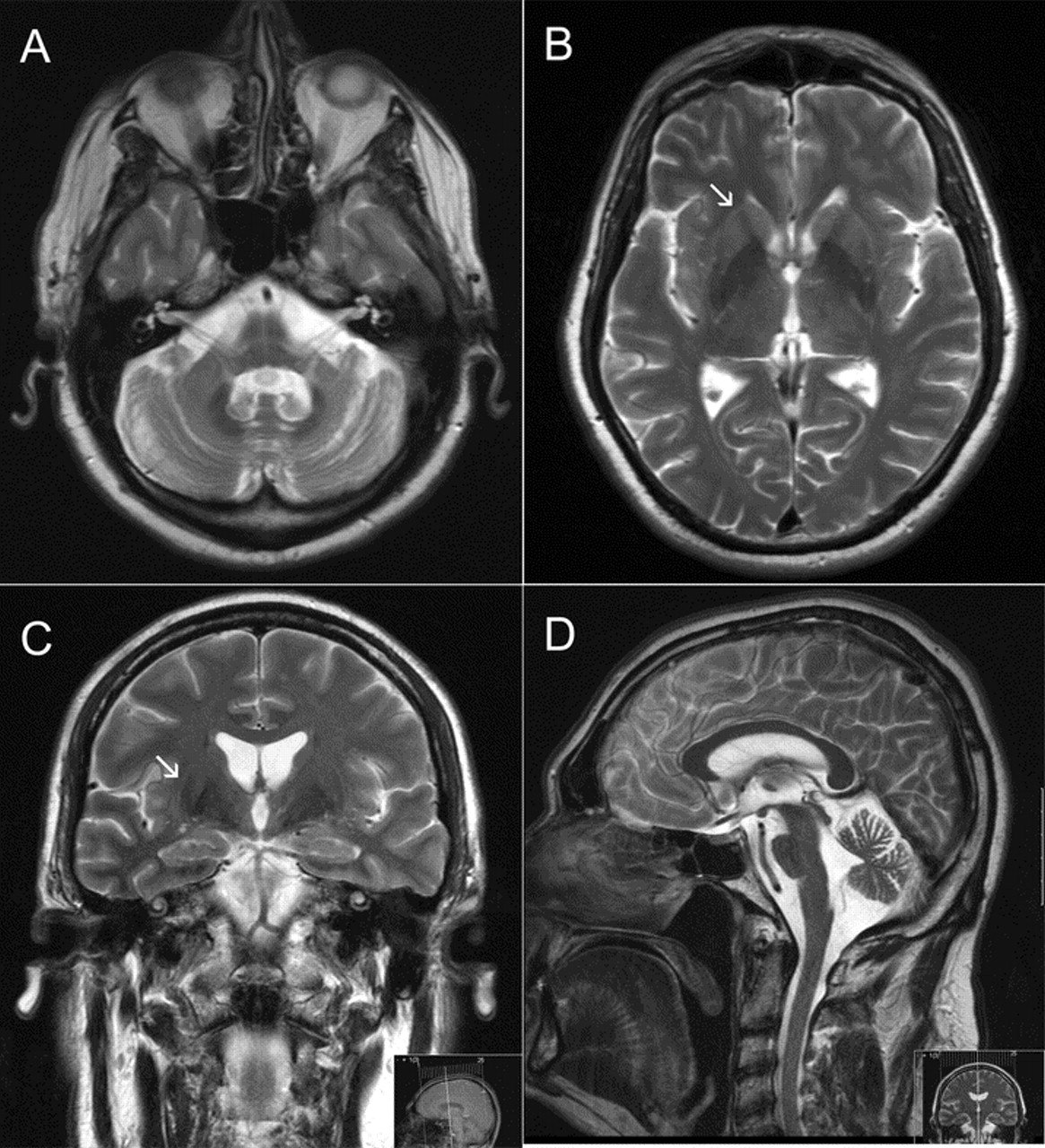
Locating The Cerebellum And Basal Ganglia
|
The cerebellum is located below the cerebrum just above the brain stem. The cerebellum coordinates the bodys movements. With information it receives from the cerebral cortex and the basal ganglia about the position of the limbs, the cerebellum helps the limbs move smoothly and accurately. The basal ganglia are collections of nerve cells located deep within the brain. They include the following structures:
The basal ganglia help smooth out muscle movements and coordinate changes in posture. |
Don’t Miss: Is Drooling A Sign Of Parkinson’s
Mirna Target Prediction And Gene Ontology Analysis
In order to search for pathways or processes that are relevant to the up-regulated and down-regulated miRNAs, we extracted predicted target genes of the identified miRNAs using miRmap and searched for statistically significant GO processes relevant to the predicted genes using MetaCore from Clarivate Analytics .
Similar Symptoms Between Multiple System Atrophy And Parkinsons
Initially, it is difficult to differentiate multiple system atrophy from Parkinsons. The similar symptoms that present in both the diseases include, tremors, rigidity and slowing of movements, incoordination and lack of balance, speech problems with difficulty speaking, orthostatic hypotension leading to spells of lightheadedness and fainting especially from seated position to standing position, bladder problems including both urinary urgency and urinary hesitancy and difficulty emptying bladder.
Recommended Reading: Parkinson’s Age Of Onset
Progression Of Autonomic And Functional Status
This is based on a preliminary analysis of 25 patients with MSA and 20 patients with PD who had completed follow-up evaluation at 12 months .3). The change in autonomic symptoms, was almost three-fold greater in MSA than PD . COMPASS_Change at 56.9±45.9 was significantly greater in MSA than PD . When domains were confined to the five selected , variance was less and the change in autonomic symptoms in MSA at 49.8±37.8 was significantly greater than in PD .
Results at 1 year of follow up or last available autonomic data.
COMPASS_Change and COMPASS_Change_Select based on a modified Autonomic Symptom Profile, percent of patients with orthostatic hypotension, CASS, TST%, and orthostatic increment in plasma norepinephrine expressed as a percent.
Blood Test May Distinguish Parkinsons From Multiple System Atrophy
A highly sensitive and specific blood test has been developed that can distinguish Parkinsons disease from multiple system atrophy , a team at the University of California, Los Angeles Health reported.
The test examines the levels of a protein called alpha-synuclein in exosomes tiny vesicles released by cells that end up in the blood. In Parkinsons, alpha-synuclein comes from neuron-derived exosomes, while in MSA it comes from exosomes released by oligodendrocytes, another type of brain cell.
Based on the content and origin of the exosomes, this test can help discriminate between Parkinsons disease and MSA.
This is a major breakthrough, because it allows us to analyze whats going on in the brain using a blood test, Gal Bitan, PhD, the studys senior author and a professor of neurology at the David Geffen School of Medicine at UCLA, said in a university press release.
The study, -Synuclein in blood exosomes immunoprecipitated using neuronal and oligodendroglial markers distinguishes Parkinsons disease from multiple system atrophy, was published in Acta Neuropathologica.
Parkinsons and neurodegenerative diseases such as MSA have several symptoms in common, including muscle rigidity and tremors. Because of this overlap in symptoms, many cases are misdiagnosed.
Incorrect diagnoses can also affect clinical trial results, as potential treatments would be tested in people without the disorder under evaluation.
You May Like: Parkinson’s And Swollen Feet And Ankles