Get Support For Your Mental Health
You can call our free and confidential helpline on 0808 800 0303.
It’s open Monday-Friday 9am-7pm and Saturday 10am-2pm. Our trained advisers can provide support to anyone affected by Parkinson’s.
You can also contact the Mind Infoline on 0300 123 3393, which is open 9am-6pm, from Monday to Friday.
If you need to talk to someone outside of these hours, Samaritans are free to call 24/7 on 116 213.
There are lots of places where you can connect with people who may be experiencing similar issues to you.
Neuropsychiatric Disorders In Parkinsons Disease: What Do We Know About The Role Of Dopaminergic And Non
- 1Inserm U1171 Degenerative and Vascular Cognitive Disorders, Lille University Medical Center, Lille, France
- 2CNRS, Institut des Sciences Cognitives Marc Jeannerod, UMR 5229, Lyon University, Bron, France
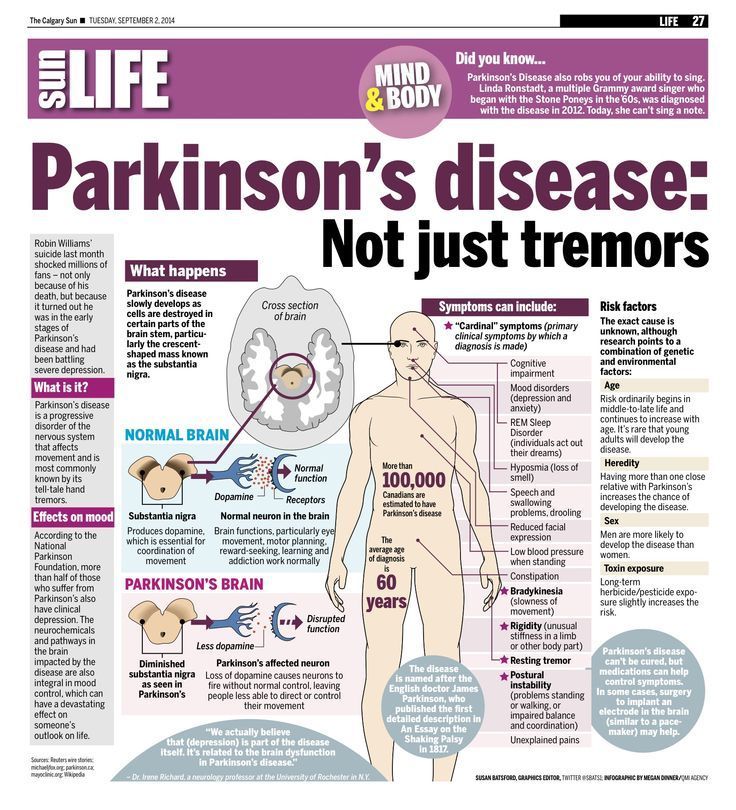
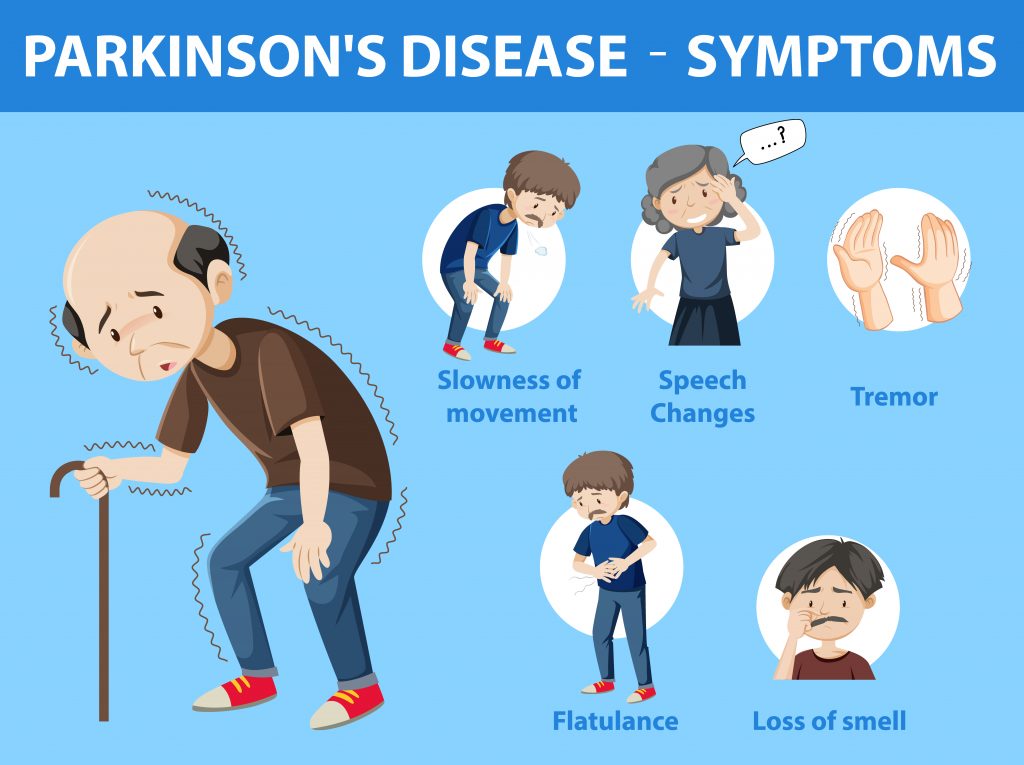
Besides the hallmark motor symptoms , patients with Parkinsons disease have non-motor symptoms, namely neuropsychiatric disorders. They are frequent and may influence the other symptoms of the disease. They have also a negative impact on the quality of life of patients and their caregivers. In this article, we will describe the clinical manifestations of the main PD-related behavioral disorders . We will also provide an overview of the clinical and preclinical literature regarding the underlying mechanisms with a focus on the role of the dopaminergic and non-dopaminergic systems.
How Is It Diagnosed
Diagnosing Parkinson’s disease is mostly a clinical process, meaning it relies heavily on a healthcare provider examining your symptoms, asking you questions and reviewing your medical history. Some diagnostic and lab tests are possible, but these are usually needed to rule out other conditions or certain causes. However, most lab tests aren’t necessary unless you don’t respond to treatment for Parkinson’s disease, which can indicate you have another condition.
Also Check: Parkinson Symptoms Caused By Medication
Depression In Parkinson’s Disease
Depression has been reported to be very common in patients with PD. In fact the relationship of depression and PD follows a vicious cycle, with the presence of either increasing the risk of other disorder. The risk of PD is patients with depressive disorders have been reported to be more than that seen in general population. A large sample retrospective study of a matched cohort of 23,180 participants , reported that patients with depression were 3.24 times more likely to develop PD compared with the control patients. Another register-based study that had data of 105,416 subjects evaluated the history of depression in patients diagnosed with PD and reported a life time prevalence of depression prior to onset of PD to be 9.2% compared to 4% in the control population and the difference between the two groups was statistically significant and the odds of having depression in patients with PD was 2.5. Few studies have evaluated the incidence of depression in patients with PD and reported the incidence rate to be 1.86-5.1% per year.
David: On Anxiety Sleep And Focusing On The Positive
David , a 74 year-old man with PD diagnosed two years ago, has been dealing with anxiety and depression for decades. I was in therapy as a teenager and young adult for issues of anxiety and depression. But about five to six years ago, the anxiety worsened, and he sought out the care of the same therapist he saw when he was in his thirties.
The intensification of his anxiety preceded his diagnosis of PD by a few years, a relatively common phenomenon in which particular non-motor symptoms of PD appear before the motor symptoms. In addition, since his diagnosis of PD, he started noticing some cognitive issues specifically trouble with his memory and word-finding difficulties.
Initially, controlling the anxiety and dealing with the cognitive changes were very difficult for David and the two issues were inter-related for him. A word-finding difficulty would inevitably trigger anxiety. I used to go crazy because I couldnt think of particular words. And that anxiety would then make it even harder to find the right word.
He cant emphasize enough the importance of a good nights sleep. He used to get four hours of restless sleep. Now with the help of his more relaxed view of life and current medication regimen, he is able to get 6-7 hours of restful sleep and that has led to a major improvement in his quality of life.
Key lessons that David can share about his mental health include:
You May Like: Difference Between Parkinson’s And Lewy Body Dementia
The Hallucinations Of Parkinsons Disease
People living with Parkinsons disease frequently experience visual hallucinations. These symptoms can occur in between 8% and 20% of patients during their illness. It is possible to have hallucinations that are visual, such as seeing animals or people, or that are auditory, such as hearing voices. While hallucinations are uncommon in the majority of patients, they can be persistent in others. Parkinsons disease patients may also exhibit increased hallucinations as the disease progresses as a marker of how severe it is. Although hallucinations do not always indicate a more serious condition, they can be a source of distress for those who have them. hallucinations can be caused by other non-motor symptoms like incontinence or insomnia. Although hallucinations are not the end of Parkinsons disease, they are one of the first symptoms that patients will experience. Affirming that hallucinations are a significant challenge for those with the disorder.
Drug Reactions: Psychosis And Impulse Control Disorders
PD pharmacologic treatment emphasises dopamine replacement, dopamine receptor stimulation, or prevention of enzymatic breakdown of dopamine in the synaptic cleft.3 While these drugs have their effects on a variety of CNS neurotransmitter systems, they primarily affect dopamine transmission. Thus, it is not surprising that they often produce dramatic behavioural changes that cause significant difficulties for patients and their families and carers.5 There are convincing data that suggest that treatment with dopaminergic agents may be associated with the development of a variety of impulse control disorders in some patients.5 Impulse control disorders, including severe gambling and hyper-sexuality as well as shopping and binge eating, can be extremely disruptive to patients and families.
As with psychosis, impulse control disorders are more commonly associated with the dopamine agonists, pramipexole and ropinirole.11 Given the impact of impulse control disorders, clinicians need to educate patients and monitor them for the early signs of these disturbances.5
Delusions are uncommon in the first two years of PD therapy, but may also occur and, as with hallucinations, are often preceded by vivid dreams.5 These delusions are usually persecutory in nature, including fears of being injured, influenced, poisoned, filmed, and/or tape-recorded.5
Read Also: Microbiome Diet For Parkinsons Disease
Also Check: Exercises For People With Parkinson’s Disease
How Common Is Parkinsons Disease Psychosis
Between 20-40% of people with Parkinsons report the experience of hallucinations or delusions. When followed as the disease progresses over the years, this number increases. The increase does not mean that the hallucinations are persistent across the majority of patients. However, it is important to note that these statistics sometimes include delirium, in which the symptoms are temporary due to medication that needs to be adjusted or infection that needs to be treated, and isolated minor symptoms or minor hallucinations, including illusions, where instead of seeing things that are not there , people misinterpret things that are really there. These are the most common types of psychosis in people with PD, with different studies placing the occurrence between 25-70% of people with Parkinsons. Typically, if the person with PD only has these minor hallucinations, their doctor will not prescribe an antipsychotic medication, though more significant psychosis that requires medication may develop over time. In one study, 10% of those with minor hallucinations had their symptoms resolved within a few years, while 52% saw their symptoms remain the same and 38% saw their psychosis symptoms get worse.
We recommend that people with Parkinsons not use a single percentage to represent the prevalence of hallucinations and PDP. Parkinsons is a complex disease and as it progresses the percentages and risk of symptoms will change.
What Lifestyle Changes Can I Make To Ease Parkinsons Symptoms
Exercise: Exercise helps improve muscle strength, balance, coordination, flexibility, and tremor. It is also strongly believed to improve memory, thinking and reduce the risk of falls and decrease anxiety and depression. One study in persons with Parkinsons disease showed that 2.5 hours of exercise per week resulted in improved ability to move and a slower decline in quality of life compared to those who didnt exercise or didnt start until later in the course of their disease. Some exercises to consider include strengthening or resistance training, stretching exercises or aerobics . All types of exercise are helpful.
Eat a healthy, balanced diet: This is not only good for your general health but can ease some of the non-movement related symptoms of Parkinsons, such as constipation. Eating foods high in fiber in particular can relieve constipation. The Mediterranean diet is one example of a healthy diet.
Preventing falls and maintaining balance: Falls are a frequent complication of Parkinsons. While you can do many things to reduce your risk of falling, the two most important are: 1) to work with your doctor to ensure that your treatments whether medicines or deep brain stimulation are optimal and 2) to consult with a physical therapist who can assess your walking and balance. The physical therapist is the expert when it comes to recommending assistive devices or exercise to improve safety and preventing falls.
Read Also: Music Therapy For Parkinsons
Also Check: What Is The Average Age For Parkinson’s Onset
What Triggers Bpd Psychosis
Borderline personality disorder is characterized by a chaotic emotional climate in which impulsivity and instability of self-image, affect, and relationships coexist. A persons perception of abandonment or rejection, as well as other factors such as inter-personal stressors, are frequently to blame for most borderline personality disorder symptoms, including psychosis.
What Are The Early Warning Signs Of Psychosis?
If you notice any of the symptoms before an episode begins, you should seek immediate medical attention. You may notice symptoms such as depression, anxiety, feeling different, or having abnormal thoughts. It is not always obvious what these symptoms are, especially during the first episode of psychosis. What does it feel like to have psychotic episodes? Adult BPD patients also experience a variety of other psychotic symptoms in addition to AVH, such as hallucinations visual hallucinations, 8% gustatory hallucinations, 17% olfactory hallucinations, 15% tactile hallucinations , thought insertion , thought blocking , being influenced by another persons thoughts ( The symptoms can cause an overwhelming sense of social isolation, as well as difficulties in everyday life. If you are experiencing any of these symptoms, you should consult with your doctor. Psychosis episodes can be difficult to manage, but medications and therapy can help.
Apathy In Parkinson’s Disease
Apathy is understood as a reduced interest and participation in normal purposeful behavior, lack of initiative with problems in initiation or sustaining an activity to completion, lack of concern or indifference and a flattening of affect. Many studies have evaluated the prevalence of apathy in patients with PD using different scales and have reported a prevalence rate of 16.5-70%, depending on the assessment procedure and the study population. Evidence suggests that apathy in PD is not related to depression, anxiety, severity of motor symptoms. However, some of the recent studies suggest high level of comorbidity between apathy and depression in patients with PD. However, some studies suggest that apathy may be a side effect of DBS and other suggest that apathy in PD is determined by the level of cognitive impairment. Recent evidence suggests that in non-depressed non-demented patients, apathy may in fact be a predictor of cognitive decline and dementia in PD.
You May Like: Balance And Parkinson’s Disease
Next Steps With Indoor Exercises
Have fun exploring the variety of options with indoor exercises. Remember, exercise helps your mind, body, and spirit and is an excellent way to curb the symptoms of Parkinsons. If you need help finding the right classes, events, or programs, dont hesitate to contact us at PCLA. Our mission is to improve the lives of people with PD, and exercise is a surefire way to do so.
Also Check: Using Cbd For Parkinsons Disease
Sleep Disorders In Parkinson’s Disease
Sleep disorders are very common in patients with PD and have a significant negative impact on their quality of life. The sleep-related problems in patients with PD can be broadly classified into daytime manifestations, nocturnal sleep disturbance, sleep-related movement disorders and parasomnias. The daytime sleep manifestations include excessive daytime sleepiness . The nocturnal sleep disturbances include insomnia and obstructive sleep apnea. The common sleep-related movement disorder include restless leg syndrome. The common parasomnias include RBD. As with depression and anxiety disorders, sleep disorders are also reported to increase the risk of development of PD in the later life. A longitudinal population-based prospective study reported increased risk of PD in patients with EDS. This risk persists after controlling for various confounders like mid-life cigarette smoking and coffee drinking, bowel movement frequency, cognitive functions, depressed mood, and insomnia. Overall, EDS was associated with a three-fold increase in the risk of developing PD. Clinic-based studies that have looked at the risk of developing PD in patients with sleep disorder have mainly focused on RBD and these studies suggest that when the patients with RBD are followed over the period, 16-65% of patients develop PD and the incidence of PD increases with longer follow-up duration.
Don’t Miss: Is Parkinson’s A Prion Disease
Caring For A Person With Advanced Parkinsons Disease
In this 47-minute webinar Anne Wallis, Associate Director of Education at the Parkinsons Foundation, talks with doctor of physical therapy, Sarah King, about when to look for outside help, how to lasso the power of your friends and family , and how to build an allied healthcare team that decreases your stress and improves your loved ones care.
Complications Of Deep Brain Stimulation Surgery
Over the past 15 years, DBS has increasingly been used as a treatment for PD, and in spite of many studies, its impact on NMS appears to be varied and complex . In addition to the relationship between DBS and ICDs already discussed, other psychiatric findings after DBS have included both overall improvement and occasionally worsening of depression, anxiety, psychosis, mania, apathy, and emotional lability . In controlled DBS studies, no between-group differences in mood were found after DBS surgery , and one study reported improvement in anxiety symptoms with DBS . Interestingly, in one controlled study comparing STN with globus pallidus interna DBS, patients who received STN DBS were more likely to experience worsening in both depressive symptoms and processing speed , but meta-analyses of RCTs have come to mixed conclusions on this topic . Clinically, pre- and postoperative psychiatric and cognitive monitoring are important with DBS, especially given reports of postsurgical suicide ideation and completed or attempted suicide , although analysis of data from one RCT found no increase in suicide ideation or attempts in the 6-month period after patients were randomized to DBS versus best medical therapy .
Don’t Miss: Que Es La Enfermedad De Parkinson Y Sus Sintomas
How Can Caregivers Support Their Loved Ones
Caring for someone who sees, hears, or believes things that arent real can be very difficult. Try to be as patient and calm as you can.
Avoid arguing with the person. If they still have insight, gently explain that what theyre seeing isnt real. Tell anyone who cares for or visits your loved one what to expect, and how to respond.
Stay in close contact with the persons doctor. If their symptoms dont improve, ask whether they need a medication adjustment.
Check whether the person needs hearing aids or glasses. Poor hearing or vision can sometimes lead to hallucinations. It can also help to turn on bright lights at night, to prevent the shadows that may trigger visual illusions.
Secure any dangerous objects, and keep pathways in the home clear to prevent falls and injuries. If you ever feel like the person is a risk to themselves or others, call their doctor.
Which Medications Can Make Confusion And Hallucinations Worse
As PD progresses, non-motor symptoms including psychosis and hallucinations become more prominent both for the patient and caregivers.9 Dopaminergic medication can exacerbate these symptoms and this can be reduced through a last in, first out approach. 27,28 Medications that have an anticholinergic effect also may cause or worsen acute confusion and the anticholinergic burden in the patients medication history should be considered.29
Recommended Reading: Is Drooling A Sign Of Parkinsons Disease
Don’t Miss: Parkinson’s And High Blood Pressure
How Can It Help In Parkinsons
Nordic walking can improve fitness in the same way that running does, but it is much kinder to the ankles, knees and hips as it has a much lower impact on the joints. This can be particularly attractive if you experience joint pain.
Perhaps the most important advantage of Nordic walking if you have Parkinsons is that is allows you to maintain and develop your ability to walk well by:
- enhancing balance and coordination
- improving mobility and creating more fluid movements
- correcting posture, particularly the stooped position associated with Parkinsons
- reinforcing the alternating movements of the arms and legs which can be lost in Parkinsons and so improving stability
- boosting independence and quality of life.
Various studies 1,2 have shown that people with Parkinsons who participate in Nordic walking programmes have improved functional independence and quality of life. It seems that mood also improves.
Once the basic steps have been learnt you can tailor your programme to suit how you feel at any particular time. Walking in a group also has social and psychological benefits.
Carers and family members who walk with you may find that they too feel fitter and have fewer aches and pains.
References