How Is Parkinsons Disease Treated
There is no cure for Parkinsons disease. However, medications and other treatments can help relieve some of your symptoms. Exercise can help your Parkinsons symptoms significantly. In addition, physical therapy, occupational therapy and speech-language therapy can help with walking and balance problems, eating and swallowing challenges and speech problems. Surgery is an option for some patients.
Have You Ever Thought How Challenging Drinking A Glass Of Water Can Be For Someone Suffering From Parkinsons Disease
On World Health Day, youll likely read about how healthy habits like exercising or drinking more water, can improve your health. While these are helpful tips and important topics to cover, we decided to take things a step further. What if you couldnt drink that glass of water by yourself? It can be daunting to consider, but this scenario can become all-too-real for a person suffering from Parkinsons disease. There are 10 million people in the world suffering from this disorder which is why, today, we decided to share with you how Parkinsons Disease can affect mobility and balance, and what can be done when the disorder is detected in its early stages. That is why raising awareness for this degenerative disease is important, and, while there is still much research to be done, we have high hopes that researchers will find a way to reduce the symptoms of Parkinsons disease, and eventually find a cure. This is becoming more and more urgent, given the fact that life expectancy is rising and the number of individuals with Parkinsons disease will only increase in the future. But is there another solution in sight?
Request Brochure
About Gait And Balance
Gait can be described simply as a persons manner of walking. Most people have a distinctive style of walking. In normal circumstances when people walk, their stance is upright and the center of gravity of the body is positioned in a manner that helps them coordinate their movement. As people walk, they swing their arms on the side, which also helps coordinate their motion.
Because of the bodys inability to coordinate movement in Parkinsons disease, it becomes progressively more difficult for people to maintain proper posture and coordination during walking. Most Parkinsons patients experience a range of walking difficulties, resulting in distinctive gait and balance problems.
Don’t Miss: What’s The Difference Between Parkinson’s And Ms
Medications For Parkinson’s Disease
After youve received a diagnosis of Parkinsons disease, your doctor will develop a treatment plan based on the diseases progression at the time you were diagnosed. Current pharmaceutical treatments include:
- Levodopa is a primary treatment for movement, tremors, and stiffness. Levodopa helps nerve cells make dopamine. This medication is also taken with carbidopa so that levodopa can reach the brain and stop or reduce side effects from the drug, such as vomiting, nausea, and low blood pressure.
- Dopamine agonists mimic dopamine in the brain but are not as effective as levodopa in controlling symptoms like muscle movement and rigidity.
- Catechol O-methyltransferase inhibitors block an enzyme that breaks down dopamine. They are taken with levodopa and slow the bodys ability to get rid of levodopa.
- MAO B inhibitors block monoamine oxidase B , a brain enzyme that breaks down dopamine. This allows dopamine to have longer-lasting effects.
- Anticholinergics aid in reducing tremors and muscle stiffness.
- Amantadine was first developed as an antiviral agent and can reduce involuntary movements caused by levodopa.
- Istradefylline is an adenosine A2A receptor antagonist. It is used for people taking carbidopa and levodopa but who experience off symptoms.
These drugs can have a variety of side effects. Be sure to discuss your medications with your doctor so you understand how and when to take them, what side effects may occur, and when to report any concerning side effects.
How Does Parkinson’s Disease Affect Balance

Parkinsons is a neurodegenerative disease that affects predominantly the dopamine-producing neurons in the brain. Dopamine is heavily involved in controlling the movement of your body, with reduced levels of dopamine, people with Parkinsons can experience obvious changes related to their movement including tremor, bradykinestia, limb rigidity, gait and balance problem.
Also Check: How Do They Test For Parkinson’s Disease
Medications And Other Causes
Balance issues in Parkinsons may occur due to medications or medication dosages. Some side effects of Parkinsons medications may affect blood pressure, dizziness, and balance. Higher doses of Duopa , for instance, have been associated with increased falls. Drugs used to treat other conditions, like blood pressure, may also cause dizziness and balance issues.
I am dizzy from the meds. Does anyone else have problems with the carbidopa/levodopa? asked one MyParkinsonsTeam member.
People with Parkinsons disease may also lose their balance and fall if there are items like furniture out of place, or if their home has not been adapted to meet their mobility needs. People get used to the arrangement of household items and grow comfortable moving around those spaces. If something gets moved out of place, it may pose a fall risk to someone with Parkinsons.
Vitamins For Parkinson’s Disease
Apart from traditional pharmaceutical treatments, if you have Parkinsons disease, your doctor may recommend vitamins with antioxidant properties. While it is best to get these from food sources as part of a healthy, balanced diet, some people need to take supplements. These vitamins include:
- Vitamin B12
- Folate
Don’t Miss: What Can You Do For Parkinson’s Disease
Balancepro Insoles Can Improve Walking Stability For Parkinsons
The key inventor of BalancePro insole, Dr. Stephen Perry has conducted a research study using the BalancePro insoles with people with Parkinsons disease. BalancePro insoles provides increased plantar sensory stimulation during gait in a group of individuals with Parkinsons disease in comparison with healthy age-matched controls. Spatialtemporal parameters of gait were evaluated using an instrumented carpet, and muscle activation patterns were evaluated using surface electromyography . All participants were tested with both BalancePro insoles and conventional insoles while walking 20 feet. Results indicated that the use of the BalancePro insoles produced a significant increase in single-limb support time. Additionally, the muscle activation sequence of the tibialis anterior was normalized by the facilitatory insole, at the time of initial ground contact. These changes may lead to an overall improvement in gait pattern and stability, and suggests that the use of the BalancePro insoles may be a useful treatment strategy for improving the gait of individuals with Parkinsons disease. This also provides support for the role of facilitation of the foot sole sensation in improving motor output in individuals with Parkinsons disease2.
Is Parkinsons Disease Inherited
Scientists have discovered gene mutations that are associated with Parkinsons disease.
There is some belief that some cases of early-onset Parkinsons disease disease starting before age 50 may be inherited. Scientists identified a gene mutation in people with Parkinsons disease whose brains contain Lewy bodies, which are clumps of the protein alpha-synuclein. Scientists are trying to understand the function of this protein and its relationship to genetic mutations that are sometimes seen in Parkinsons disease and in people with a type of dementia called Lewy body dementia.
Several other gene mutations have been found to play a role in Parkinsons disease. Mutations in these genes cause abnormal cell functioning, which affects the nerve cells ability to release dopamine and causes nerve cell death. Researchers are still trying to discover what causes these genes to mutate in order to understand how gene mutations influence the development of Parkinsons disease.
Scientists think that about 10% to 15% of persons with Parkinsons disease may have a genetic mutation that predisposes them to development of the disease. There are also environmental factors involved that are not fully understood.
Don’t Miss: Do You Get Pain With Parkinson’s
How Does Parkinsons Disease Progress
The Parkinsons Foundation states there are typical patterns of progression of Parkinsons disease that can be defined in 5 stages:
With proper treatment, most individuals with Parkinsons disease can lead long, productive lives for many years after diagnosis. In fact, life expectancy for those affected by Parkinsons is about the same as for people without the disease. Its the quality of life of those affected by Parkinsons disease that suffers, so how can we tackle all the challenges the disease poses to ones quality of life?
What Are The Symptoms Of Parkinsons Disease
Symptoms of Parkinsons disease and the rate of decline vary widely from person to person. The most common symptoms include:
Other symptoms include:
- Speech/vocal changes: Speech may be quick, become slurred or be soft in tone. You may hesitate before speaking. The pitch of your voice may become unchanged .
- Handwriting changes: You handwriting may become smaller and more difficult to read.
- Depression and anxiety.
- Sleeping disturbances including disrupted sleep, acting out your dreams, and restless leg syndrome.
- Pain, lack of interest , fatigue, change in weight, vision changes.
- Low blood pressure.
Recommended Reading: How Close To A Cure For Parkinson’s
Balance Exercises For People With Parkinsons Disease
Parkinson is a progressive disorder of the central nervous system, affects an individuals motor system and results in shaking, tremors, difficulty in walking, etc. While there are medications like Levodopa and Amantadine which are often prescribed to Parkinsons disease. Exercising could be one of the best ways to stay healthy in Parkinson. So, maintaining balance can be a challenge for people who are suffering from Parkinsons disease. Today, we will share top 12 balancing exercise for people with Parkinsons disease.
What Lifestyle Changes Can I Make To Ease Parkinsons Symptoms
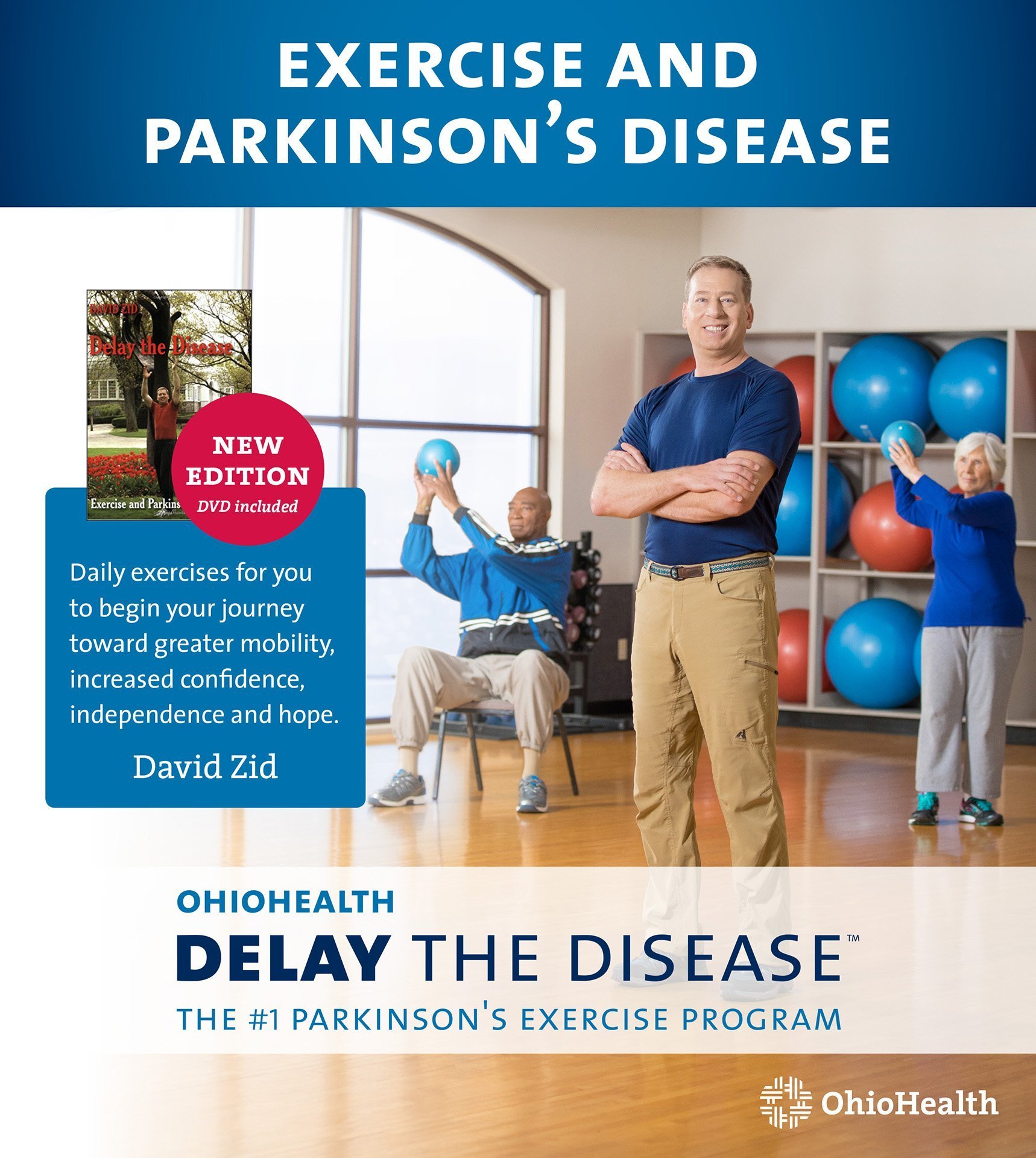
Exercise: Exercise helps improve muscle strength, balance, coordination, flexibility, and tremor. It is also strongly believed to improve memory, thinking and reduce the risk of falls and decrease anxiety and depression. One study in persons with Parkinsons disease showed that 2.5 hours of exercise per week resulted in improved ability to move and a slower decline in quality of life compared to those who didnt exercise or didnt start until later in the course of their disease. Some exercises to consider include strengthening or resistance training, stretching exercises or aerobics . All types of exercise are helpful.
Eat a healthy, balanced diet: This is not only good for your general health but can ease some of the non-movement related symptoms of Parkinsons, such as constipation. Eating foods high in fiber in particular can relieve constipation. The Mediterranean diet is one example of a healthy diet.
Preventing falls and maintaining balance: Falls are a frequent complication of Parkinson’s. While you can do many things to reduce your risk of falling, the two most important are: 1) to work with your doctor to ensure that your treatments whether medicines or deep brain stimulation are optimal and 2) to consult with a physical therapist who can assess your walking and balance. The physical therapist is the expert when it comes to recommending assistive devices or exercise to improve safety and preventing falls.
Recommended Reading: Non Shaking Parkinson’s Disease
Parameters And Data Analysis
Prior to analysis, all force-plate raw time series data were band-pass filtered between 0.001 and 10 Hz. For all sway values, the mean of the four trials per condition was used in statistical analysis.
Sway data were also analysed according to a continuous PID control model in a subgroup of eight patients in addition to the healthy controls using a custom script developed in MATLAB according to the following established method where standing is considered analogous to an inverted pendulum . Assumptions included using ballistic elbow reaction time as a measure of delay in feedback control and that the body was rigid . Ballistic elbow flexion was considered a reasonable estimate of postural reaction times given its strong reticulospinal innervation . Patient height was used to convert sway data to angular displacement according to trigonometry. The resultant parameters were gains in time domains of future, present and past scaled in arbitrary units . To facilitate statistical analysis, we normalized these values in the Parkinsons disease patients relative to the data for healthy controls and expressed the difference as a percentage. The mean of each percentage yielded a single value of PID model function for each patient/condition relative to healthy controls.
Why Is Fall Prevention So Important
Oftentimes a fall will cause no injury or a mild, easily reversible injury, however, sometimes a fall can cause moderate to significant injury.
In addition to the fall itself potentially causing a fracture or head injury, the fall could possibly result in an ER visit, hospital stay, or surgery, which can sometimes set off a series of events that has the possibility of worsening a persons PD even more substantially. Hospitalizations can interfere with medication timing, contribute to simultaneous infection, precipitate hallucinations, and increase confusion. Each of these setbacks can spawn additional setbacks which can contribute to the worsening of PD overall. In addition, immobilization after a fracture can interfere with exercise and physical therapy goals. For all of these reasons and more, it is important to do all that you can to reduce the chance of falls.
Also Check: Canes For Parkinson’s Patients
People With Parkinsons Are At High Risk Of Falling
According to a retrospective fall study of 489 in-patients admitted to a department of neurology, approximately 60% of PD patients had a history of at least one fall over the previous twelve months1. Gait and posture impairment are the main causes of falls for Parkinsons. There is increasing evidence that these motor impairments may be partially due to deficits within the sensory system.
What Medications Are Used To Treat Parkinsons Disease
Medications are the main treatment method for patients with Parkinsons disease. Your doctor will work closely with you to develop a treatment plan best suited for you based on the severity of your disease at the time of diagnosis, side effects of the drug class and success or failure of symptom control of the medications you try.
Medications combat Parkinsons disease by:
- Helping nerve cells in the brain make dopamine.
- Mimicking the effects of dopamine in the brain.
- Blocking an enzyme that breaks down dopamine in the brain.
- Reducing some specific symptoms of Parkinsons disease.
Levodopa: Levodopa is a main treatment for the slowness of movement, tremor, and stiffness symptoms of Parkinsons disease. Nerve cells use levodopa to make dopamine, which replenishes the low amount found in the brain of persons with Parkinsons disease. Levodopa is usually taken with carbidopa to allow more levodopa to reach the brain and to prevent or reduce the nausea and vomiting, low blood pressure and other side effects of levodopa. Sinemet® is available in an immediate release formula and a long-acting, controlled release formula. Rytary® is a newer version of levodopa/carbidopa that is a longer-acting capsule. The newest addition is Inbrija®, which is inhaled levodopa. It is used by people already taking regular carbidopa/levodopa for when they have off episodes .
You May Like: Emotional Symptoms Of Parkinson’s
Impaired Kinesthesia Affects Sensory Integration
Central sensory integration involves active interpretation of visual, vestibular and somatosensory inputs for orientation of the body in space. When sensory information is unavailable or conflicting, a process of sensory reweighting occurs so the nervous system ignores ambiguous, unhelpful information and relies more on useful sensory information. For example, somatosensory input normally contributes 70% to postural stability when standing on a firm surface with eyes open but, but vestibular input contributes 100% to postural stability when standing on an unstable surface with eyes closed . Patients with advanced PD are often unable to stand on an unstable surface with eye closed, although their vestibular system is usually normal . This finding suggests that patients with PD may take more time for the sensory reweighting process than healthy people. Another problem in sensory orientation is that the patients with PD have impaired use of proprioception for a kinesthetic body map. For example, patients with PD have difficulty perceiving small changes in surface inclination, i.e., impaired kinesthesia . Consequently, a poor sense of kinesthesia in PD is compensated by an over-reliance on vision for postural orientation.
Bradykinesia Impairs Postural Responses And Anticipatory Postural Adjustments
Automatic postural responses to unexpected external perturbations of the bodys CoM can be classified into feet-in-place and change-in-support strategies . In patients with PD, both types of postural response strategies are smaller and slower than normal. Feet-in-place postural responses are slow to develop force with reduced scaling up for larger perturbations, often leading to displacement of the body CoM within base of support . Interestingly, postural responses are even weaker with levodopa medication . Patients with PD are also unable to quickly change postural muscle synergies with changes in initial support conditions, called inflexible central set, for example, standing versus-sitting posture, holding versus-free stance, surface translation versus-rotation, and voluntary resist versus-relax . The difficultly adapting the pattern of muscle activation for changes in conditions may explain why it is difficult for patients with PD to benefit from assistive devices, such as canes and walkers, to improve stability.
Change-in-support strategies are also slowed and smaller due to bradykinesia . Small compensatory stepping responses in response to external perturbations are larger when patients are provided a visual cue and can see their stepping leg . However, when the stepping leg is not visible, the step to a visual target falls short, consistent with an increased visual dependence to overcome bradykinetic compensatory steps .
Read Also: Parkinson’s Big Movement Exercises