Tips For Dealing With Chronic Pain
Chronic pain is one that last more than 3-6 months , or pain that extends behind the expected period of healing. This blog post explains the different types of pain caused by Parkinsons disease and how to address pain brought on by the disease, by medications, or by comorbid disease. It is always best to treat pain before it becomes chronic.
Signs And Symptoms That Tell You To Be Mindful
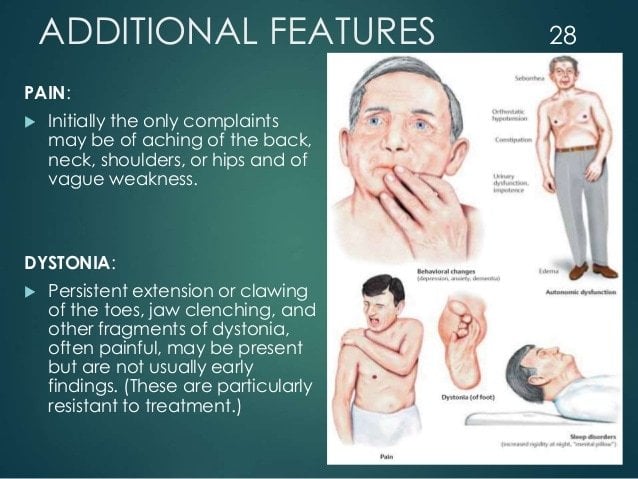
Sometimes it comes without advising, but sometimes it provides you signals like rigidity on the backside, numb discomfort while sitting or rising. Dont neglect these signs it might bring about acute lower pain in the back in the future. So when you get alerting signals, its much better not to overstrain your body. Relax for a few days till these signals are gone and after that begin your workouts again.
Usual reasons for lower pain in the back:
- Incorrect handling of points like raising any type of weight unexpectedly
- Excessive connecting as well as extending your back too much
- Lengthy hours of resting
- If you are really tall
- Physical work that give stress to your back
- Crashes
Relax is a crucial point when suffering from lower back pain. Due to the fact that often, it is a simple stretching of the muscle mass that causes the pain, and a few days remainder can recover you. Yet it is not that straightforward constantly pain on your lower back can be a signal of something being wrong inside. So if you are prone to these backaches, it is far better to get a physicians recommendations and act as necessary. Parkinsons Disease And Low Back Pain
Some other kinds of workouts to enhance your lower back muscular tissues.
Besides the 11 Finest stretches and also Workouts to Reinforce Your Lower Back, here are some of the various other types of simple workouts that can aid you gain lower back stamina are given listed below:.
Who Should I See To Discuss My Parkinsons Pain
Your first point of contact should be your primary doctor. Whether that means your family doctor, neurologist, or Movement Disorder Specialist , start by asking them how to manage your pain. They may prescribe you one of the medications listed above, offer suggestions about altering your lifestyle, or refer you to a pain specialist.
Pain management specialists are physicians with specialized training in the field of evaluating, diagnosing, and treating pain so, speaking to one of these specialists might be helpful for you. Be sure to get a referral from your primary care doctor, though, to ensure you are visiting a physician who understands the complexity of treating Parkinsons-specific pain.
Health and wellness providers like physical therapists, acupuncturists, and massage therapists can also be valuable members of your care team. Be willing to try new things and approach alternative therapies with an open mind, as no ones path with Parkinsons pain is the same. What works for someone else may not work for you and vice versa. Consider visiting different specialists to find a treatment plan that works best for you.
Also Check: Diseases Similar To Parkinsons
Strengthening Exercises Or Stretching May Be Helpful
Imagine that the spine is like a telephone pole or the mast of a sailboat. If the pole is not exactly upright, even a slight tilt requires a great force to keep it from tilting further and falling. In the human body, this means that the lower back muscles are under great stress. It also means that the tension on the back bones is much increased as well. This worsens whatever problems, like arthritis, that are already present. The same process applies to the neck, although the forces are less great. Strengthening exercises or stretching may be helpful. Almost everyone over the age of 60 has arthritis in their spine. Luckily most dont have pain from it, but those who do will have it worsened by the spine curvature caused by the PD.
PD patients also frequently have an aching discomfort in their muscles, particularly in the thighs and shoulders. I think this is due to the rigidity, or stiffness, that is part of the Parkinsons Disease syndrome, but Ive seen many patients with this pain and no apparent stiffness on examination, hence not explained. It is common and it often, but not always, responds to alterations of the usual Parkinsons Disease medications for movement. Exercise and stretching may be helpful as well and should always be tried first before increasing medications.
Pain is a challenge in PD. We cant measure it and often cannot find its cause. It is, however, often treatable, and reducing pain improves quality of life.
Examples Of Pain Scales In Pd
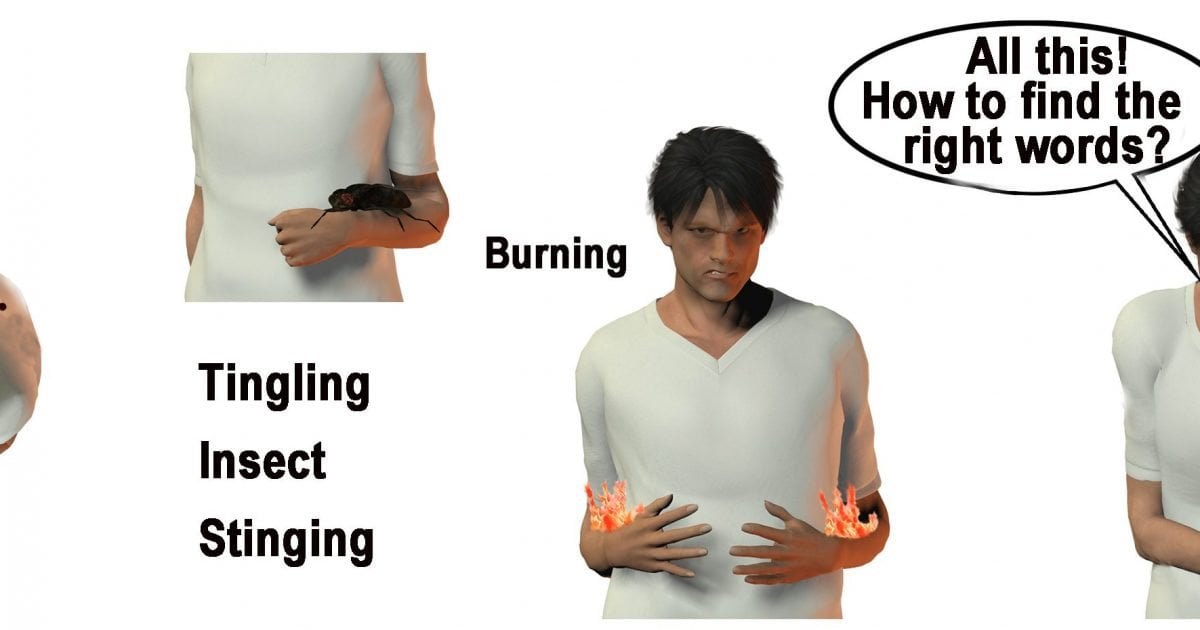
Pain-O-Meter
This is a self-administered pain assessment tool developed for the purpose of improving pain assessment and management in acute and chronic pain patients, not exclusively for PD pain. It is a hard, white, plastic tool. Two methods for assessing pain are located on the Pain-O-Meter . The first is a 10-cm VAS with a moveable marker that patients use to rate their pain. The second is a list of 15 sensory and eleven affective WDSs. Each WDS is assigned an intensity value that can be as low as 1 or as high as 5 .
| Durationa of disease, 5 years/> 5 years | Pain before/after PD diagnosis | Durationb of pain/day, 10 h/> 10 h | VAS,c5 cm/> 5 cm | Pain expressions by participants |
|---|
Notes: POM results for PD and chronic pain patients. Data from Skogar et al.
P
Abbreviations: PD, Parkinsons disease h, hours VAS, visual analog scale RLS, restless legs syndrome POM, Pain-O-Meter.
Kings PD Pain Scale
Recommended Reading: Pfnca Wellness Programs
Mechanical Constraint Of Rigidity
Rigidity is one of the cardinal symptoms of PD and can be evident across axial, proximal, and distal body segments. Although largely neural rather than peripheral in its generation , the rigidity associated with PD elicits a significant mechanical constraint that associates with impaired gait quality , turning , standing postural sway , and diminished quality of life . Direct measurement of axial rigidity by slow, passive trunk or hip rotation in stance demonstrates an increased rigidity with PD that correlates with clinical symptom scores and with difficulty walking or rolling over . Thus, rigidity is a pervasive impairment in PD that influences mobility, balance, and daily life.
Lower Back Pain And Parkinsons Disease
Lower back pain is an extremely common problem in the general population, as well as for people with Parkinsons disease . It tends to make moving more difficult, adding to the challenges of PD. Tim Nordahl, PT, DPT, a physical therapist at Boston University gave an excellent presentation as part of APDAs Lets Keep Moving Webinar Series. Because this is such a prevalent issue, and because there are things you can do to help alleviate your back pain, I wanted to summarize and highlight this important topic.
Also Check: Weighted Silverware
Active Research Into Several Aspects Of Parkinsons Pain
Researchers are working to better understand the mechanisms behind pain in Parkinsons so that it can be more effectively addressed. They are looking for objective measurements, such as brain imaging, to diagnose and monitor pain, and to evaluate response to treatment. And, theyre investigating several drugs and deep brain stimulation for their potential benefits in treating Parkinsons disease pain.
How To Deal With The 6 Common Causes Of Leg Pain In Pd
Severe leg pain is a common complaint from people with PD. Lately, it is understood that central pain is common to Parkinsons disease, and can even be the first sign of PD, usually bilaterally. This blog post lists six causes of lower limb pain, and the importance of treating it. Treatments depend on properly identifying the source of pain. Some treatment suggestions are included.
Read Also: Yopd Life Expectancy
Other Treatments Of Lower Back Pain
NSAIDs which include medications such as ibuprofen and naproxen, as well as acetaminophen, can be very beneficial for pain in PD, as they are for the general population. These medications do not typically have neurologic side effects, so they are well tolerated in people with PD. They can have other side effects though, so as always, discuss all medications that you are taking, including over-the-counter medications, with your doctor. If these medications do not provide sufficient back pain relief, your doctor may prescribe a pain medication. In addition, he/she may refer you for a procedure such as an epidural injection to help with lower back pain. Rarely, surgery may be recommended if a specific structural reason for pain is identified.
Revisiting Pain In Pdthe 50 Shades Of Pain Experienced By Parkinsons Patients
Pain is a quality of life issue for people with Parkinsons disease and can be under treated by doctors who may assume that is worsens as the disease progresses, although for some pain is an initial symptom of PD. This article helps focus your physicians attention in the right direction to accurately diagnose your pain.
You May Like: Parkinson Bicycle Cleveland Clinic
Pathophysiological Pathways Of Pain In Pd
The origin of pain in PD remains poorly understood. At times, it appears as dystonia when the dopaminergic effects wear off. The pathophysiological mechanisms behind this phenomenon are most probable by which dopamine, in the network with other monoamines such as noradrenaline and 5-hydroxytryptamine , interacts through inhibitory and excitatory pathways. Abnormalities in descending pathways affect central pain processing. In addition, clinically registered neuropathic pain and other muscular pain sensations are described by PD patients. This has led to the exploration of pathways other than those secondary to rigidity, tremor, or any other motor manifestations of the disease, with abnormal nociception processing in PD patients suffering from pain as the most likely suspect. The basal ganglia process somatosensory information in different ways, and increased subjective pain sensitivity with lower electrical and heat pain thresholds has been reported in PD patients. This abnormal processing also comprises PD-related disorders such as multiple system atrophy, which exhibits almost the same prevalence of pain as PD.
The pathophysiological basis of sensory disturbances in PD, the so-called pain matrix with information from different loci, processed in the BG.
Abbreviations: PD, Parkinsons disease BG, basal ganglia GPe, globus pallidus externa, GPi, globus pallidus interna STN, subthalamic nucleus.
What Can I Do On A Regular Basis To Manage My Pain
Remember, youre your best advocate as you understands how your pain feels. Understanding and communicating the kind of pain youre experiencing can greatly inform your treatment plan and will allow your doctors to address the type and severity of your specific pain. Keep your care team informed about activities that cause pain or the times of day your pain is worst so they can help fine-tune your care plan. Do you notice the pain starting to creep in at a certain point after you take your medication? Do you feel fine when you bike but experience pain when you jog? Did you start experiencing this pain before or after your Parkinsons diagnosis? Taking stock of these sorts of questions can be helpful as you work with your care team to effectively treat your pain.
Incorporating approved medications and following the pain ladder can also help you find the right pain management solution, as can taking steps in your everyday life to be an active participant in your own pain management. Regular stretching, heat and cold treatments, exercise, yoga, and dance can all help reduce your pain, and they are all steps that you can take on your own. Making adjustments to your home and workspace, such as minimizing places where fall risks are likely, using an ergonomically designed desk, sleeping in a comfortable bed, and wearing clothes and shoes that dont exacerbate pain, can help you establish a more pain-free daily routine.
Don’t Miss: Cleveland Clinic Parkinson’s Bicycle Study 2017
Lower Back Pain In People With Parkinsons
In a previous blog, we discussed pain and PD in general and highlighted different types of pain that a person with PD might experience.
PD contributes factors that can cause or worsen lower back pain, such as rigidity of the trunk muscles or dystonia of the trunk muscles. Both rigidity and dystonia can fluctuate with medication timing and correlate with ON and OFF time.
In addition, PD can be associated with central pain, which is poorly understood and thought to be due to abnormalities in the brain itself. Some new research suggests that PD can change how the brain feels pain that the loss of dopamine can make pain feel worse or make a person more likely to feel pain.
We know that:
- there is a higher prevalence of lower back pain in people with PD vs aged-matched controls
- certain features of PD such as increased age, depression, rigidity, and stooped posture are associated with lower back pain
- lower back pain can make it harder to deal with the challenges of PD because it is associated with lower activity levels. This can breed a vicious cycle in which lower back pain leads to decreased activity levels and then lower activity levels conspire to make the lower back pain worse
Chiropractic Care For Low Back Pain Gait And Posture In A Patient With Parkinsons Disease: A Case Report And Brief Review
Eric Chun Pu Chu1^, Arnold Yu Lok Wong2^, Linda Yin King Lee3
1 New York Chiropractic and Physiotherapy Centre , 41/F Langham Place Office Tower , Hong Kong, Department of Rehabilitation Sciences, The Hong Kong Polytechnic University, Hong Kong , School of Nursing and Health Studies, The Open University of Hong Kong, Hong Kong , China
^ORCID: Eric Chun Pu Chu, 0000-0002-0893-556X Arnold Yu Lok Wong, 0000-0002-5911-5756.
Correspondence to:
Keywords: Chiropractic back pain gait cyclogram Parkinsons disease walking difficulty
Received: 18 April 2021 Accepted: 09 June 2021 Published: 25 October 2021.
doi: 10.21037/acr-21-27
Read Also: On Off Phenomenon
My Parkinson’s Story: Pain
This 10-minute video alternates between an interview with a man and and doctors. The man shares his experience with pain as a symptom of Parkinson’s disease. The doctors explain that pain is common in Parkinson’s disease, often due to rigidity or dystonia, which can be exacerbated by “off” periods. Pain caused by Parkinson’s symptoms can be relieved by Parkinson’s medications, exercise, DBS and botox injections. Pain is an invisible symptom that should be mentioned to your neurologist.
How Is It Categorized
Doctors categorize pain as nociceptive, which refers to pain from tissue damage, or as neuropathic, which refers to pain that arises from the nerves. Some pain is both nociceptive and neuropathic. Most people with PD experience nociceptive pain.
This type of pain is generally localized to a specific area of the body. The most common areas for people with PD to experience pain are the neck, upper back, and the extremities . Neuropathic pain is less common in PD, although it may be caused by akathisia, an extreme restlessness.1
The pain caused by PD can generally be classified by one of five causes:
You May Like: Voice Amplifiers For Parkinson’s
Sensory Acuity Kinesthesia And Dynamic Central Sensory Integration
Any type of physical activity optimally requires accurate sensation and perception of ones own position and movement , and both PD and LBP associate with impaired kinesthesia. People with PD exhibit impaired tactile sensation and impaired kinesthesia to detect limb position during active motion as well as to detect passive limb and trunk rotation . People with LBP exhibit impaired two-point discrimination and can be unable to kinesthetically perceive their lumbar trunk based on body image traces . In contrast to the global somatosensory impairment exhibited by people with PD, the impaired tactile discrimination of people with LBP appears to be isolated to the area of the LBP . Impaired lumbosacral repositioning accuracy has also been reported for people with LBP . Further, similar to the impaired detection of trunk motion exhibited by people with PD, people with LBP exhibit increased thresholds for detecting passive trunk flexion and lateral bending . Thus, although the extent of impairment may differ between people with PD versus LBP, both health conditions associate with impaired tactile acuity and kinesthesia.
Physiological Pathways Of Pain Relief
In the early 1960s, theories initially developed by Melzack and Wall were introduced. They proposed three features of afferent input that were signed for pain: the ongoing activity that precedes the stimulus, the stimulus-evolved activity, and the relative balance of activity in large versus small fibers. The concept of the gate control theory was introduced. Pain messages encounter nerve gates in the spinal cord that open or close depending upon a number of factors . When the gates are open, pain messages pass more easily and pain can be intense. When the gates are closed, pain messages are prevented from reaching the brain and may not even be experienced. Although the details of this process remain poorly understood, it can help to explain why various treatments are effective.
The existence of low-threshold mechanoreceptive C-tactile afferents was initially described by Vallbo et al. These afferents comprise a second anatomically and functionally distinct system that signals touch in human beings. The activation of these fibers is more closely related to limbic functions rather than cognitive and motor functions. Although rapid, accurate, and informative A touch acutely reflects the external world through cutaneous events in an exteroceptive manner, CT activation shares more characteristics with interceptive modalities. This slow, affective nature is likely to be involved in the maintenance of physical well-being.
Don’t Miss: Parkinson’s Bike Therapy
Neck Pain In Women Linked To Parkinson’s Disease
Is ongoing neck pain in women a possible sign of early Parkinson’s disease? Neck pain can accompany Parkinson’s disease, a condition characterized by tremors, stiffness, and bradykinesia but it is not a symptom of early-stage Parkinson’s disease.
There are many possible causes of neck pain, regardless of whether you’re a woman or a man. Neck pain is common, especially in older adults, and it can result from muscle strain, injury, arthritis, a more serious cause , and several different diseases.
If you have persistent neck pain, you should see your doctor, who can evaluate you to pinpoint the cause of the pain and determine how it should be treated. If it’s caused by your Parkinson’s disease, then treating your movement disorder may help reduce your neck pain.