Fecal Incontinence In Advanced Parkinsons Disease
Fecal incontinence is a very debilitating symptom that can occur in advanced PD and refers to the involuntary release of fecal matter.
Once again, fecal incontinence, especially if it is a new symptom, should be fully evaluated to determine if there is a cause unrelated to PD. Diseases of the gut such as inflammatory bowel disease or compression of the lower spine cord can be the reason.
If related to PD, there are typically two situations to consider. One possibility is that severe constipation with impacted bowel movement allows loose stool from higher up in the gastrointestinal tract to escape around the edges of the obstruction. In this situation, fecal incontinence could be a harbinger of bowel obstruction. Aggressive and continuous treatment of constipation can help avoid this potential scenario.
As with urinary incontinence, frequent and rapid exchange of dirtied incontinence products can keep skin intact and prevent infection.
Tips and Takeaways
Increased Risk Of Overactive Bladder In Patients With Idiopathic Parkinsons Disease: Insight From A Nationwide Population
-
Roles Conceptualization, Investigation, Methodology, Writing original draft
Affiliation Department of Neurology, China Medical University Hospital, China Medical University School of Medicine, Taichung, Taiwan
-
Affiliation Department of Neurology, China Medical University Hospital, China Medical University School of Medicine, Taichung, Taiwan
You May Like: Pfnca Wellness Programs
Prevalence Of Lower Urinary Tract Symptoms Urinary Incontinence And Retention In Parkinson’s Disease: A Systematic Review And Meta
1Department of Neurology, Center for Movement Disorders, Beijing Tiantan Hospital, Capital Medical University, Beijing, China
2China National Clinical Research Center for Neurological Diseases, Beijing, China
3Department of Neurology, Beijing Chaoyang Hospital, Capital Medical University, Beijing, China
Also Check: Treatments Available For Parkinson’s Disease
Difficulty Emptying The Bladder
- Some people with Parkinsons find it difficult to pass urine if the bladder fails to contract when required, or because the sphincter does not let urine out or a combination of the two. This is a result of reduced dopamine levels interfering with the efficiency of the bladder muscles and causing a residual amount of urine to be left in the bladder. This reduces the total amount the bladder can hold and creates a feeling of wanting to empty the bladder very often. Unfortunately, there is an increased risk of urinary infection if the bladder is not emptied completely.
- In some older people, constipation which is often associated with Parkinsons can result in faeces collecting in the rectum. This can result in difficulties in bladder emptying, which may be because of pressure on the urethra, or mediated by the nerves in the region. The bladder is then unable to empty and may continue distending, causing dribbling incontinence.
- Anticholinergic medications can also make emptying problems worse.
Urinary Issues In Advanced Parkinsons Disease
Urinary dysfunction and symptoms in PD are most commonly caused by overactivity of the detrusor muscle, or the muscle of the bladder, which contracts excessively despite the fact that it is not filled with urine. This causes an increased urge to urinate and/or an increased frequency of urination, which can be especially prominent at night. In advanced PD, this could culminate in urinary incontinence, or involuntary release of urine. Mobility issues which make getting to the bathroom slower and more cumbersome, compound the problem.
Always remember that people with advanced PD may have other medical problems that affect their urination such as an enlarged prostate. Make sure to have a complete evaluation before assuming that the problem is only related to PD. It is also essential to keep in mind that if changes in urination occur suddenly, there could be a urinary tract infection present.
Once other medical issues and urinary tract infection are ruled out, there are a number of approaches to the issue of urinary incontinence in a person with advanced PD:
Unfortunately, for some, the above available options may not be sufficient to effectively treat urinary incontinence in advanced PD. If this is the reality, it becomes extremely important to keep the skin dry with frequent changes of incontinence products to prevent skin breakdown and the potential development of skin infection.
Don’t Miss: Symptoms Of Parkinsons In Women
Evaluating And Treating Urinary Issues In Parkinson’s Disease Multiple System Atrophy And The Other Atypical Parkinsonism Disorders
In this hour-long webinar, neuro-urologist Ekene Enemchukwu, MD focuses on urinary incontinence, overactive bladder, urinary retention, and other urinary issues in PD, MSA, and the atypical parkinsonism disorders. Following the presentation, moderator Candy Welch, Brain Support Networks MSA caregiver support group leader, asks Dr. Enemchukwu many questions submitted by webinar participants.
Thanks For Signing Up
We are proud to have you as a part of our community. To ensure you receive the latest Parkinsons news, research updates and more, please check your email for a message from us. If you do not see our email, it may be in your spam folder. Just mark as not spam and you should receive our emails as expected.
Recommended Reading: How To Help A Urinary Tract Infection
You May Like: Does Parkinson Cause High Blood Pressure
What Is Parkinsons Disease
Parkinsons disease is a progressive neurological disorder that affects how your muscles move. In the beginning stages, it can be easy to miss the early signs and symptoms of Parkinsons disease. The most common ones include:
- Tremors, usually starting with the fingers or hand
- A noticeable change in handwriting
- Walking is slower, movement is stiffer
- Stiff, rigid muscles
The symptoms of urinary retention are not always obvious but may include
- Hesitancy really having to strain to pass urine
- Strong feelings of urgency and frequency and when passing urine only a small amount comes out
- A urinary stream that is very weak and intermittent
Whilst your bladder is not emptying properly there is a risk that the residual urine in the bladder will become infected. This could cause further complications and problems if it isnt removed regularly. It is important to seek help if you experience any of the above symptoms.
It is a good idea to keep a record of your bladder activity in a bladder diary for a few days before your appointment with your doctor or nurse.
Your Doctor or Healthcare Professional may recommend the following tests:
Recommended Reading: Cialis And Parkinsons Disease
Urinary Problems In Parkinsons Disease
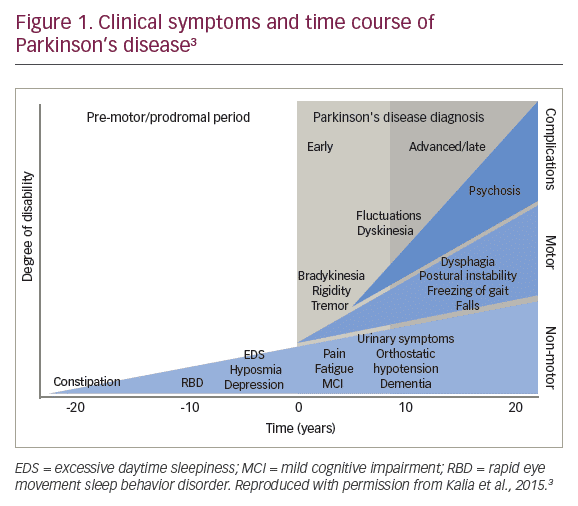
Parkinsons disease has many features that have little or nothing to do with movement. Among these non-motor symptoms are problems with the autonomic nervous system the part of the nervous system that controls automatic bodily functions, such as heart rate, blood pressure, sweating, sexual function and both gastrointestinal and urinary function. These symptoms are often among the most serious and complex issues faced by people with PD.
Unlike bowel dysfunction , which often occurs before Parkinsons movement symptoms, urinary dysfunction is not typically a problem until the later stages of the disease.
Recommended Reading: Parkinsons Double Vision
You May Like: All Symptoms Of Parkinson’s Disease
Make Changes To Diet & Lifestyle
- Healthy and balanced diet means a happy bladder and bowels!
- A diet rich in veggies and fruits always helps with clean living.
- I have found that a diet rich in organic foods with less processed foods helps too.
- We get dehydrated easily! Drink fluids! Gatorade and water are great!!
- Alcohol, soda, and caffeine can irritate the bladder, so I try to drink those sparingly.
Reduced Functional Bladder Capacity At Night
Functional bladder capacity is diminished if the bladder wall compliance is reduced, the detrusor is involuntarily contracting , or if the bladder has incompletely emptied following a void. All three of these are known to occur in PD. Nocturia results whenever the urine volume produced at night exceeds the functional bladder capacity. Urodynamic evidence for detrusor overactivity has been reported in 45% to 93% of PD patients, , and correlates with scores in overactive bladder questionnaires. In urodynamic studies, 81.0% had storage disorder, 54.8% had abnormalities of storage and voiding, whereas 19.0% had only a voiding disorder.,
A likely mechanism for DO in PD is disruption of the dopamine D1-GABAergic direct pathway and its GABAergic collateral to the micturition circuit,, resulting in loss of inhibition of the micturition reflex and OAB. Severity of OAB symptoms has been shown to correlate with impairments observed on urodynamic testing and dopaminergic deficiency observed in dopamine transporter scans.,
You May Like: Physical Therapy Exercises For Parkinson’s Disease
The Pathophysiology Of Voiding Dysfunction In Parkinsons Disease
The hypothesis most widely accepted is that in healthy individuals basal ganglia output has an overall inhibitory effect on the micturition reflex.In PD animal modelsdepletion of dopaminergic neurones induces overactive bladder, and D1 receptor agonists produce inhibition of the micturition reflex in a dose-dependent manner while D2 receptor stimulation facilitates micturition. In PD degeneration of dopaminergic neurons in the substantia nigra leads to detrusor hyperactivity, through an inability to activate the D1-mediated tonic inhibition. A parallel mechanism may be that in PD, the inhibitory dopaminergic neurons originating in the substantia nigra may be more damaged than the excitatorydopaminergic neurons originating in the VTA, thereby inducing urgency and frequency.
Papers Of Particular Interest Published Recently Have Been Highlighted As: Of Importance Of Major Importance
Other Formats
Don’t Miss: Parkinson’s Support Group Connecticut
Ui And Adverse Health Outcomes
The mean follow-up of time of the participants was nearly 8 years . We employed a Cox proportional hazards model adjusted for age, sex, and education to examine the association of baseline UI with incident parkinsonism. Baseline UI was associated with incident parkinsonism . Since we treated UI as a numerical scale, inspection of the hazard ratio suggests that an individual with severe incontinence , had about a 30% increased risk of developing parkinsonism as compared to an individual without incontinence.
Since the pathologic basis for parkinsonism in older adults with and without a clinical diagnosis of PD may vary , we repeated this analysis excluding 65 cases with a clinical diagnosis of PD. Baseline UI remained associated with incident parkinsonism . In a final model, adding terms for seven chronic health conditions and BMI did not attenuate the association of UI with incident parkinsonism .
In further analyses, we examined whether baseline UI was associated with other adverse health outcomes. Baseline UI was also associated with risk of death and incident ADL and mobility disability, but was not associated with incident MCI or AD dementia . These findings were unchanged when we controlled for seven chronic health conditions and BMI .
The Cross-Sectional and Longitudinal Associations of Baseline Urinary Incontinence and Global Cognition in Community-Dwelling Older Adults*
| Model Terms . |
|---|
Bladder Irrigation And Clean Catheterization
Bladder irrigation with various solutions such as aminoglycoside, glycosaminoglycans , povidone-iodine , chlorhexidine solution , and saline with acetylcysteine have been advocated as a management strategy for patients with indwelling catheters or those who require intermittent catheterizations . Although several studies have demonstrated the efficacy of bladder irrigation with various agents , gentamicin remains the best intravesical treatment that has shown efficacy in both the prevention and treatment of recurrent UTIs . Furthermore, the risk of developing antibiotic resistance and systemic adverse effects is low in patients treated with bladder irrigation with gentamicin .
You May Like: Side Effects Of Parkinson Disease Medicine
Whats Next For Those Suffering From Urinary Incontinence
I decided I did not want to add another medication to the medicine bag. I was trying to see if there was something I could do besides resigning myself to wearing pads or some other incontinence protection all the time. At 53 years old, I wanted to see if there was a way I could help myself.
Part 2 of this article will address my experiences. I plan to discuss what I lovingly refer to as PEE PEE PT physical therapy to help treat urinary incontinence.
Recommended Reading: On And Off Phenomenon
What’s Next For Those Suffering From Urinary Incontinence
I decided I did not want to add another medication to the medicine bag. I was trying to see if there was something I could do besides resigning myself to wearing pads or some other incontinence protection all the time. At 53 years old, I wanted to see if there was a way I could help myself.
Part 2 of this article will address my experiences. I plan to discuss what I lovingly refer to as “PEE PEE PT” – physical therapy to help treat urinary incontinence.
Read Also: Michael J Fox Cure For Parkinson’s
Treating And Managing Bladder Problems
It is important to discuss any bladder difficulties, including those listed below, with your doctor, even if this may appear embarrassing. Your doctor will then be able to properly assess and treat any problems, for example:
- inability or difficulty emptying the bladder even when it feels full
- significant, uncontrolled leakage of urine at any time
- unusually frequent urination
- an urgent, immediate need to urinate, or urine leaking if you do not immediately do so
- pain when urinating.
It may be helpful to write notes to discuss with your doctor, for example, the type of difficulties experienced, their frequency, when you first noticed a change, and your normal eating and drinking habits.
Bladder problems can occur for a number of reasons, so the first approach will be to eliminate causes other than Parkinsons, such as urinary infections and prostate problems in men.
Dont Miss: Weighted Silverware
Parkinsons Disease And Your Bladder
Many diagnosed with Parkinsons disease experience urinary tract issues. A Michigan Medicine urologist discusses treatment options for patients to consider.
Anne Pelletier-Cameron, M.D., often jokes to her patients that shes a female plumber of the lower urinary tract. On a more professional note, however, shes a urologist in the Michigan Medicine Department of Urology.
In this role, Pelletier-Cameron treats patients with a variety of lower urinary tract symptoms. Some of her patients have been diagnosed with Parkinsons disease, a progressive nervous system disorder that impacts movement. But the breakdown of nerve cells that characterize Parkinsons disease can also cause non-movement symptoms, including bladder issues.
Half of all women and 17% of men will experience urinary incontinence, or the inability to hold urine, she says, noting that for Parkinsons disease patients, those numbers escalate.
Many of my PD patients end up having other bladder problems, including issues with urgency and frequency, says Pelletier-Cameron. Nocturia, or the need to urinate many times during the night, is also common, along with difficulty in emptying the bladder.
Pelletier-Cameron says the impact of bladder symptoms cant be ignored.
You May Like: Drugs Cause Parkinson’s Disease
Nasal Spray Provides Relief For Nocturia
One published study examined the effectiveness of AV002, a recently approved emulsified vasopressin nasal spray, in treating elderly patients with nocturia due to nocturnal polyuria. Benjamin M. Brucker, MD, associate professor in the Departments of Urology and Obstetrics and Gynecology, director of female pelvic medicine and reconstructive surgery and neurourology, and director of the female pelvic medicine fellowship program, reported results during a late-breaking session of the 2018 meeting of the American Urological Association and as part of a team at the International Continence Society 2018 annual meeting in Philadelphia.
Men and women with nocturia awaken multiple times during the night to urinate, interfering with sleep patterns and often triggering associated problems, such as cognitive decline, depression, and a weakened immune system. Although anticholinergics are currently the standard treatment, previous research by Dr. Brucker and his colleagues demonstrated that AV002 acts faster and is more effective.
The treatment paradigm were currently following isnt very effective as a medical community, we could be doing a better job with the management of these patientsand now we have the needed insight to effectively and safely get them the deep, restorative sleep they need.Benjamin M. Brucker, MD
Voiding Symptoms In Pd
The pooled prevalence of voiding symptoms was 24%. Prolongation was the most prevalent type of voiding symptoms in PD followed by the intermittency , urinary retention , dysuria , weak stream , and hesitancy . Some studies found that subclinical detrusor weakness during voiding may also occur in PD . These findings revealed that PD patients had both subclinical and clinical voiding symptoms. There was substantial heterogeneity in prevalence of voiding symptoms and its subtypes among studies. The source of heterogeneity could be the limited number of articles, diverse diagnostic tools and different characteristic of participants.
Urinary retention is the most disabling voiding symptoms and often used to differentiate Parkinson’s disease from multisystem atrophy. Previous studies have shown that the prevalence of urinary retention and large PVR was 43 and 14% in MSA and PVR volume 100 ml might be an effective indicator to differentiate PD from MSA . Unexplained voiding difficulties with PVR volume 100 ml was one of the core clinical features to identify the clinically established MSA . Furthermore, severe urinary retention in the first 5 year of disease is a red flag according to MDS clinical diagnostic criteria for PD.
Don’t Miss: Anxiety In Parkinson’s Disease
Problems Caused By Limited Mobility
Some people with Parkinsons might soil their underwear. This is because mobility problems can make it difficult to wipe after using the toilet. If this is the case, it might help to use wet wipes, a bidet, or an adapted bottom wiper. An occupational therapist or the Disabled Living Foundation can offer further advice.
Bowel problems are common. But you should tell your GP if there are any changes in your bowel habits, particularly if you see blood in your stool. Some problems are difficult to avoid, but there are things you can do to make them less likely to happen.
Read Also: Parkinson Bicycle Cleveland Clinic
Urinary Incontinence In Parkinsons Disease
The most common urinary difficulty experienced by people with PD is a frequent and urgent need to urinate. This may occur even when the bladder is not full. Recent research studies estimate approximately 27-39% of people with PD experience urinary difficulties, although urinary incontinence only develops in about 15% of those with PD. Bladder issues are more common in the later stages of PD.2
Read Also: Do Women Get Parkinson’s