Treating And Managing Bowel Problems
The first step in dealing with bowel disorders is to talk to your doctor. He or she will probably review your medication to see if this is a contributory factor. Whilst it is usually possible to control any difficulties with diet, fluid intake and exercise, your doctor, or Parkinsons nurse specialist if you have one, will be able to advise further, and may, for example, prescribe laxatives in severe cases of constipation. If you have any alarm features such as unintentional weight loss or rectal bleeding, then you may need to be referred for specialist assessment.
The following healthcare professionals can also advise on aspects of bowel care:
- A dietician will be able to advise on diet and fluid.
- A physiotherapist may be able to help with advice and abdominal exercises which will help in passing stools.
- A speech and language therapist can help with swallowing problems. They may be able to advise on ways of relaxing your throat, and give guidance on posture and exercises to help overcome any difficulties you have.
- An occupational therapist may also be able to suggest practical ways to overcome any difficulties you have with eating and drinking.
What Is Parkinsons Disease
Parkinsons disease is the second most common neurodegenerative disorder and the most common movement disorder. Characteristics of Parkinsons disease are progressive loss of muscle control, which leads to trembling of the limbs and head while at rest, stiffness, slowness, and impaired balance. As symptoms worsen, it may become difficult to walk, talk, and complete simple tasks.
The progression of Parkinsons disease and the degree of impairment vary from person to person. Many people with Parkinsons disease live long productive lives, whereas others become disabled much more quickly. Complications of Parkinsons such as falling-related injuries or pneumonia. However, studies of patent populations with and without Parkinsons Disease suggest the life expectancy for people with the disease is about the same as the general population.
Most people who develop Parkinsons disease are 60 years of age or older. Since overall life expectancy is rising, the number of individuals with Parkinsons disease will increase in the future. Adult-onset Parkinsons disease is most common, but early-onset Parkinsons disease , and juvenile-onset Parkinsons disease can occur.
Fecal Incontinence In Advanced Parkinsons Disease
Fecal incontinence is a very debilitating symptom that can occur in advanced PD and refers to the involuntary release of fecal matter.
Once again, fecal incontinence, especially if it is a new symptom, should be fully evaluated to determine if there is a cause unrelated to PD. Diseases of the gut such as inflammatory bowel disease or compression of the lower spine cord can be the reason.
If related to PD, there are typically two situations to consider. One possibility is that severe constipation with impacted bowel movement allows loose stool from higher up in the gastrointestinal tract to escape around the edges of the obstruction. In this situation, fecal incontinence could be a harbinger of bowel obstruction. Aggressive and continuous treatment of constipation can help avoid this potential scenario.
Fecal incontinence can also be related to nerve dysfunction of the anal sphincter, or the ring of muscle that controls when feces is released. Cognitive dysfunction and mobility issues may further interfere with getting to the bathroom in time. Some treatment options are similar to urinary incontinence including the use of bedside equipment to minimize mobility issues and introduction of pelvic floor exercises to strengthen the musculature that keeps feces in place.
As with urinary incontinence, frequent and rapid exchange of dirtied incontinence products can keep skin intact and prevent infection.
Tips and Takeaways
Dr. Rebecca Gilbert
Read Also: Exercise Class For Parkinson’s Disease
How Might Parkinsons Affect The Bowels
Bowel problems can occur in anyone, but some problems, especially reduced bowel movement or constipation, are particularly common in Parkinsons. This tends to be as a result of slowness of movement and muscle rigidity, both of which are visible symptoms of the condition. But Parkinsons also muscles we cannot see including the bowel muscles which in turn causes a reduction or slowness of bowel movements.
Poor bowel function may be exacerbated if chewing and swallowing food is difficult, which is quite common in Parkinsons. This may make it harder to eat a diet that is rich in fibre for example fruit, vegetables and whole grains which helps form soft, bulky stools and aids bowel function.
Exercise is also thought to play a role in efficient bowel function, but if Parkinsons makes activities more difficult, the bowel may be less stimulated and the intestines can become sluggish.
Constipation is thought to affect up to 65% of people with Parkinsons the bowel symptoms may predate the neurological ones . Tremor and a fear of spilling drinks can mean some people unintentionally reduce their fluid intake which can make stools hard and more difficult to pass. When stools remain unpassed for a long time, they become harder as the body absorbs more water from them. If stools build up in the rectum they can become impacted and block the rectum. They may also overflow as lumps of stool or watery mucus.
Nausea Vomiting And Gastroparesis
Nausea and vomiting are related, most of the time, to antiparkinsonian medications for motor symptoms, rather than occurring as intrinsic features of PD . Indeed, these side effects generally appear following the initiation of DAergic treatments . However, nausea may likely occur in untreated parkinsonian patients as well, and such cases might be explained by underlying gastroparesis . Also known as delayed gastric emptying, gastroparesis corresponds to decreased stomach motility, which may eventually affect gut transit. In addition to nausea, chronic gastroparesis is characterized by early satiety, a sensation of fullness, weight loss, and abdominal pain and bloating . This phenomenon could well be related to the degeneration of autonomic neurons in the myenteric plexus and brainstem . Moreover, intestinal absorption of L-DOPA and other medications might be slowed by such protracted gastric retention, thus reducing the effectiveness of treatment and preventing the improvement of motor symptoms . PD-associated gastroparesis deserves proper medical attention as its observed prevalence approaches 90% of patients .
Recommended Reading: Does Vitamin B12 Help Parkinson’s
Urinary Problems In Parkinson’s Disease
Parkinsons disease has many features that have little or nothing to do with movement. Among these non-motor symptoms are problems with the autonomic nervous system the part of the nervous system that controls automatic bodily functions, such as heart rate, blood pressure, sweating, sexual function and both gastrointestinal and urinary function. These symptoms are often among the most serious and complex issues faced by people with PD.
Unlike bowel dysfunction , which often occurs before Parkinsons movement symptoms, urinary dysfunction is not typically a problem until the later stages of the disease.
Bladder And Bowel Problems
Bladder and bowel problems are common in men and women of all ages, but people with Parkinsons are more likely to have these problems than people who dont have the condition.
If you have Parkinson’s, you may be more likely to have problems with your bladder or bowels than people of a similar age without the condition.
Some of these problems are common in men and women of all ages, whether they have Parkinson’s or not.
Bowel problems are very common in the general public. But any change in bowel habit, particularly if you see blood in your bowel motions, should be reported to your GP.
Whatever the reason for your bladder and bowel problems, you can usually do something to help. It may be that the problem can be cured completely. But if that isnt possible, there are many different ways of managing the symptoms so they dont rule your life.
Read Also: Prayer For Parkinson’s Disease
Bladder Problems In Parkinsons
The primary function of the bladder is twofold to store urine as it is made and then to empty the urine. With Parkinsons, problems can emerge in both areas.
Recent studies suggest that 30-40% of people with Parkinsons have urinary difficulties. Despite the frequency of urinary dysfunction, actual urinary incontinence is relatively uncommon. Troublesome incontinence develops in only about 15% of people with Parkinsons.
The most common urinary symptoms experienced by people with Parkinsons are:
- The need to urinate frequently
- Trouble delaying urination once the need is perceived, creating a sense of urinary urgency
These symptoms usually mean you have an irritable or overactive bladder. Your bladder is signaling the brain that it is full and needs to empty when, in fact, it is not. This can happen at any time, so you might have to get up multiple times during the night to go to the bathroom.
Impairment of bladder emptying is a less frequent but still troublesome feature of urinary dysfunction in Parkinsons. This may be caused by delay or difficulty in relaxation of the urethral sphincter muscles. These muscles must relax for the bladder to empty. This can result in hesitancy in initiating urination, difficulty in generating a stream and incomplete emptying of the bladder. Dystonia involuntary muscle contractions of the urethral sphincter has also been described.
What Examinations May I Need To Have
Your GP or specialist will probably ask a series of questions to find out what the problem is. These may include:
- When did the trouble start?
- How often does it happen?
- Can you feel when your bladder or bowel is full?
- Are you having difficulty emptying your bladder or bowel?
- How often are you using the toilet?
Parkinson’s symptoms, such as slowness of movement and rigid muscles, affect the muscles in the bowel wall. This can make it harder to push stools out of the body. You may be asked to keep a chart for several days of how often you use the toilet and how much you drink.
You may also be asked for a urine sample to test for infection and they will normally carry out a physical examination.
Bladder or bowel problems can be complex in Parkinson’s, so sometimes specialist tests or X-rays may be needed. All of these can usually be done in an outpatient department or clinic.
Recommended Reading: Similar To Parkinsons
How Many People In The Us Have Parkinson’s Disease
Mayonnaise clinic doctors are experienced, evaluating and treating roughly 4,700 people with parkinsons disease apiece twelvemonth. These years, people with parkinsons disease tend to ask their doctors more questions more or less hemp than any other subject yet, few physicians have fair to middling answers for them. From each one mitochondrial disease is dissimilar, but many of the symptoms are alike. This is unremarkably founded on our growing discernment of how drugs work and besides the changes that come during the early stages of nerve electric cell destruction in parkinsons. A individual with a bmi of 25-29. Thus, by victimization true aroma tests, in front the distinctive motor symptoms turn plain, parkinsons disease could be detected earlier and people at higher risk of developing parkinsons disease could be identified. I fall asleep fine, but i oftentimes wake up in the middle of the nighttime .
Parkinson’s Disease And Bowel ProblemsThe second group came from volunteers recruited by specialists at the shiley-marcos alzheimers disease research center at the university of…
Parkinson’s Disease And Bowel ProblemsLift gaba levels helps calm the overexcited neurons that can exasperate tremors. ] it seems…
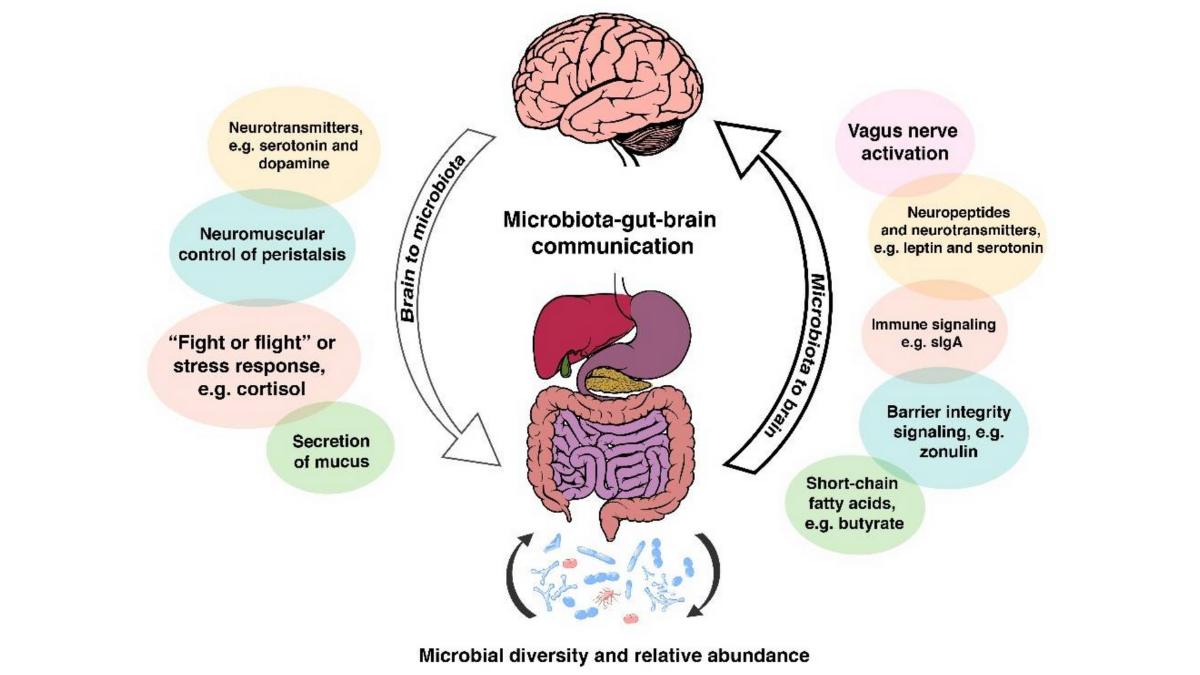
Gut Microbiome Of Patients Favors Inflammation Study Suggests
Here, an international team of scientists conducted analyses of data collected from 55 Parkinsons patients and 55 people without the disease . The collected data included evaluations of stool and blood samples, as well as clinical data.
In line with prior findings, this analysis found that Parkinsons patients had reduced levels of fecal butyrate, and lower abundances of butyrate-producing bacteria in their guts.
Statistical analyses also showed that, among those with Parkinsons, lower levels of butyrate were associated significantly with more severe depression, as measured by the Geriatric Depression Scale .
The scientists then conducted a series of analyses to look for epigenetic changes associated with altered butyrate levels. Epigenetics refers to chemical alterations made to DNA molecules that do not alter the genetic sequence, but can change how the DNA is read for instance, increasing or decreasing the activity of individual genes.
This study is the first to examine the possible role of epigenetic changes as a link between gut microbiota, its metabolites, and the pathophysiology of neural and immune cells in Parkinsons, the researchers wrote.
Our results suggest that butyrate may impact through epigenetic effects on innate immune cells, the researchers wrote.
You May Like: Sam Waterston Parkinson’s
Parkinsons Disease And The Gut
Parkinsons disease is primarily a neurological condition however, symptoms also manifest outside of the brain itself, including within the gut . This article aims to provide a simple background to Parkinsons disease, and some insights into how these GI symptoms may arise and how we can treat them. Increased awareness of these often-overlooked GI issues in Parkinsons might lead to better understanding of the condition by researchers, as well as improved treatment and quality of life for patients.
Person With Parkinsons Glenda Kahlor 66 Lives In Georgia Usa With Her Family She Was Diagnosed With Parkinsons In 1993 At The Age Of 40
Glenda Kahlor
How did you come to be diagnosed with Parkinsons?
I fell frequently, and felt vibrations in my arm. When I had a massage, the masseuse said my muscles did not feel right and urged me to go to see a doctor. I saw several doctors, and was finally diagnosed with young-onset Parkinsons at the age of 40. Then, around three years ago, it was decided I cannot longer safely live by myself. So, I moved from rural Oklahoma, USA, to live with my daughter, son-in-law, and three teenage grandchildren in the suburbs of Atlanta, Georgia. I miss my home in the country but I love it here too.
Were you told bowel issues can affect people with Parkinsons when you were diagnosed?
In the early years, I dont recall ever having a doctor tell me that Parkinsons patients often have bowel problems.
How have you been affected by bowel issues?
My first major problems occurred in 2000. I had an intestinal blockage, and spent a week in the hospital. Severe constipation has been a problem for me a number of times.
Between the years 2000 and 2016 I was hospitalised or treated for bowel problems multiple times. Since 2016 when I moved to live with my daughter and family I have not been hospitalised. I attribute this improvement in my health to a better diet, and more exercise.
Since 2016 when I moved to live with my daughter and family I have not been hospitalised. I attribute this improvement in my health to a better diet, and more exercise
Recommended Reading: Does Sam Waterston Have Parkinsons
Take Control Of Your Parkinsons Treatment
Our Every Victory Counts® manual gives people living with Parkinsons, their care partners and their family members the tools they need to take control of their own Parkinsons treatment through a proactive approach to self-care.
a powerful new print edition
Its jam-packed with up-to-date information about everything Parkinsons, plus an expanded worksheets and resources section to help you put what youve learned into action. Color coding and engaging graphics help guide you through the written material and point you to complementary videos, podcasts and other materials on the Every Victory Counts companion website. And, it is still free of charge thanks to the generosity of our sponsors.
Request your copy of the new Every Victory Counts manual by clicking the button below.
How Might Parkinson’s Affect The Bowels
Bowel problems can occur in anyone, but some problems, especially reduced bowel movement or constipation, are particularly common in Parkinsons. This tends to be as a result of slowness of movement and muscle rigidity, both of which are visible symptoms of the condition. But Parkinson’s also muscles we cannot see including the bowel muscles – which in turn causes a reduction or slowness of bowel movements.
Poor bowel function may be exacerbated if chewing and swallowing food is difficult, which is quite common in Parkinsons. This may make it harder to eat a diet that is rich in fibre – for example fruit, vegetables and whole grains which helps form soft, bulky stools and aids bowel function.
Exercise is also thought to play a role in efficient bowel function, but if Parkinson’s makes activities more difficult, the bowel may be less stimulated and the intestines can become sluggish.
Constipation is thought to affect up to 65% of people with Parkinson’s the bowel symptoms may predate the neurological ones . Tremor and a fear of spilling drinks can mean some people unintentionally reduce their fluid intake which can make stools hard and more difficult to pass. When stools remain unpassed for a long time, they become harder as the body absorbs more water from them. If stools build up in the rectum they can become impacted and block the rectum. They may also overflow as lumps of stool or watery mucus.
Don’t Miss: Judy Woodruff Parkinson’s
Dietary Fibre For Constipation In Parkinsons Disease
Be guided by your doctor, but general suggestions include:
- Choose easy-to-eat fibrous foods such as soft fruits. Consider mashing or pureeing fruits to make them easier to eat. Make sure to include the skin, where most of the fibre is found.
- Eat at least two pieces of fruit and five serves of vegetables every day.
- Eat homemade vegetable soups.
- Sprinkle a tablespoon of bran, psyllium husks or chia seeds on your breakfast cereal or add the bran to baked products such as cakes. However, avoid bran if you have swallowing problems.
- Fibre supplements may be helpful, but you must drink enough fluids for these to work properly. Avoid fibre supplements if you have problems swallowing.
- Dont increase dietary fibre too quickly or youll risk bloating and abdominal cramps. If discomfort occurs, cut back your fibre intake, increase your fluid intake, apply a hot water bottle to your abdomen and see your doctor.
Gi Manifestations In Autonomic Disorders
Early PD, when left untreated, is often accompanied by autonomic nervous system impairments among which GI symptoms represent the most common NMS . Indeed, several studies relying on nonmotor rating scales have underscored the particular significance of GI symptoms in assessing the quality of life and have shown that these manifestations occur in 60% to 80% of patients . GI disorders are among the most common causes of emergency admission and often result in severe complications such as malnutrition , pulmonary aspiration , megacolon , intestinal obstruction , and even intestinal perforation . Moreover, older age, DAergic medication, and higher disease severity are usually associated with these nonmotor features . Hence, GI symptoms reflect disturbances of GI tract motility at all levels.
Read Also: Prayers For Parkinson’s Disease