How The Brain Progresses With Pd
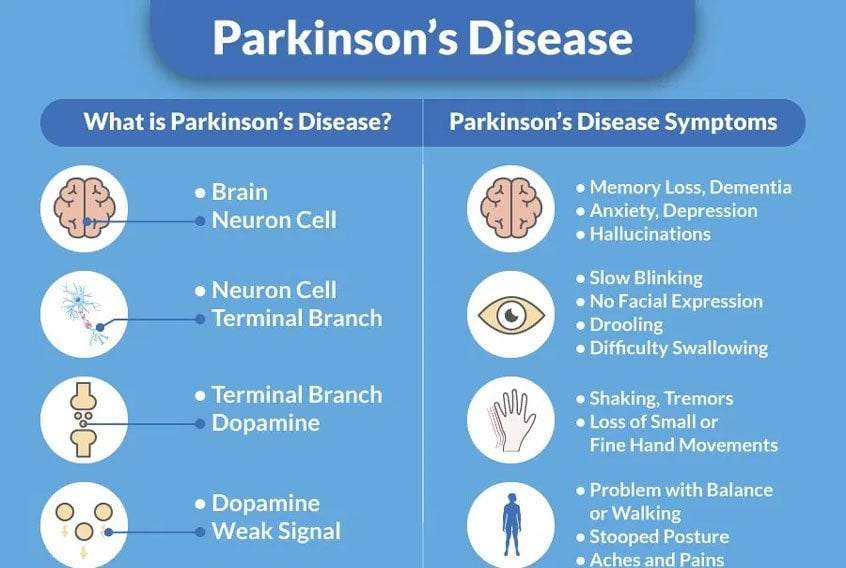
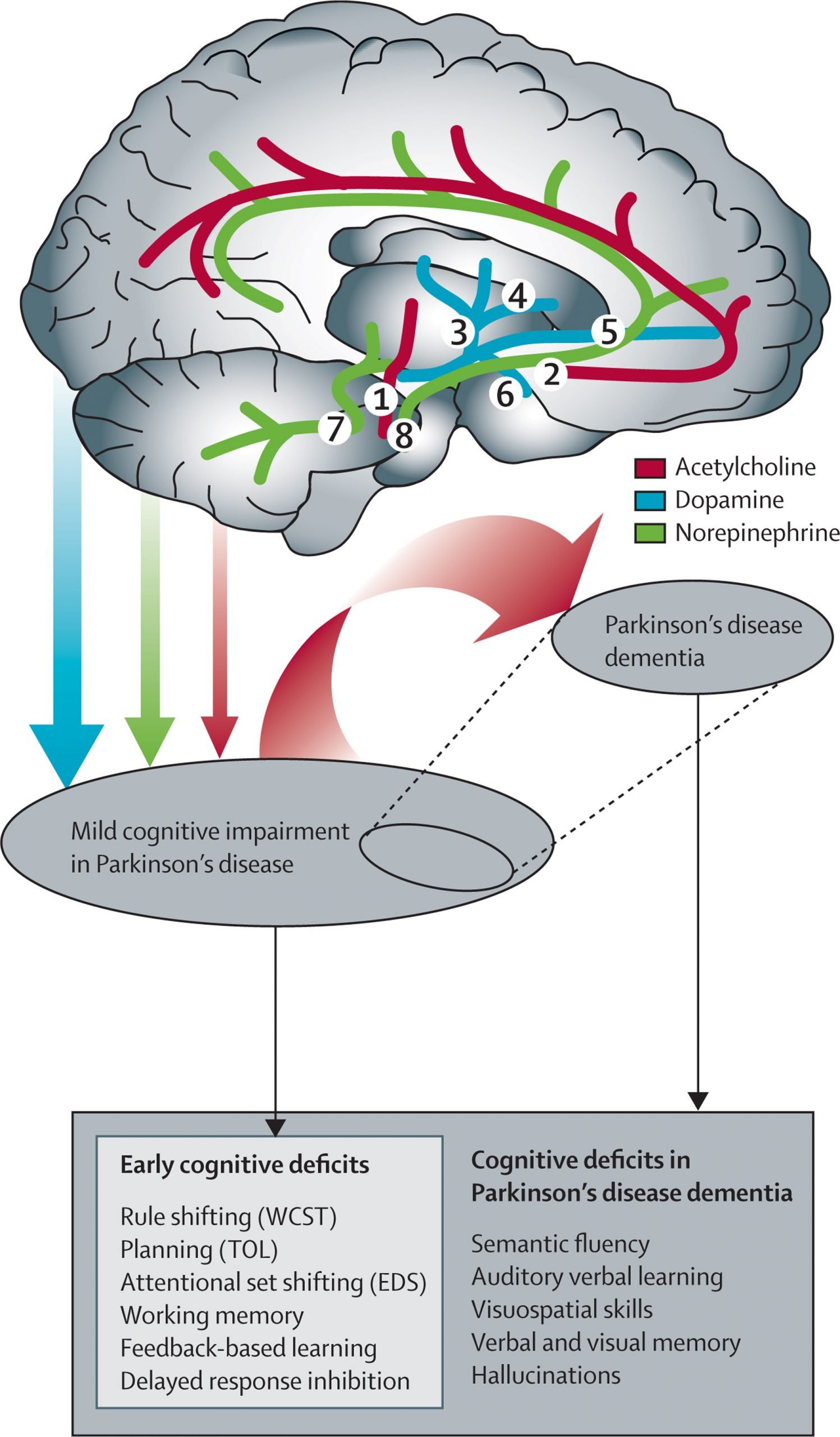
In this one-hour webinar movement disorder specialist Yasar Torres-Yaghi shared how the pathology of Parkinson’s disease begins in the gut before progressing to the brain. As the pathology expands throughout the brain it affects more neurotransnitters than just dopamine causing both motor and non-motor symptoms. Dr. Torres-Yaghi shares a widely used cognitive evaluation tool before answering questions about communicating well with your neurologist and advocating for the care you need.
Dealing With Cognitive Impairments
In some circumstances medications can help to lessen cognitive symptoms. You should speak to your GP or specialist about the options available. There are also various other health professionals who can provide professional support for dealing with cognitive impairments.
Cognitive impairment can be a big challenge for family, friends and carers, as well as those with the symptoms. Some practical tips for dealing with the daily challenges of cognitive impairments include:
- Keep to a daily routine
- Try to use familiar objects and phrases
- Avoid unfamiliar environments
Nutritional Interventions: Can They Help Cognition In Pd
Good nutrition is essential for living well in general and with PD, not only playing a role in optimizing general health and motor strength but also potentially cognitive function. The relationship between nutrition and cognition is an area of growing interest to the PD community. In a large cross-sectional survey conducted by the Parkinson Alliance , 93% of participants reported that they believed that diet/nutrition was important in managing their PD symptoms. Yet, only 11% of participants reported that a healthcare professional offered specific dietary recommendations to them. The majority of participants who followed a specific diet designed their meal plans based on information obtained from self-help resources , family, and friends. Moreover, while 63% of respondents perceived themselves as eating a healthy diet most of the time, there is a lack of consensus as to what comprises a healthy diet for people with PD. Discussions regarding nutrition in PD have typically focused on topics such as protein and medication absorption, weight loss, dysphagia, and gastrointestinal issues. However, there are growing investigations of nutrients that may be associated with increased or decreased risk of PD. Increased consumption of dairy products and lower serum urate levels may be risk factors for PD, whereas high intake of fruits, vegetables, and fish or use of nicotine and caffeine may confer a lower risk of PD.,
Recommended Reading: Treatment For Parkinson’s Disease Usually Includes
Memory Difficulties In Parkinsons
The most common difficulty for people with PD is remembering information that has previously been learned. Memory has several different processes and types, and people with PD have trouble recalling information but their long-term memory function generally remains intact. Memory cues or choices can help people with PD to retrieve information from the brains long-term storage.3,4
Care Partners: Burden Assessment And Support
Care partners or caregivers are an invaluable healthcare resource. When caregivers are present, patients are less likely to move to nursing homes. Caregivers also improve participation rates and retention of people with PD in research studies, which helps advance the path towards finding more effective therapeutics. Furthermore, many clinical trials for PDD require a caregiver in the study inclusion criteria.
Informal caregivers are providers who supervise or assist with instrumental and/or basic activities of daily living without pay to someone who cannot do these activities independently due to cognitive, physical, or psychological impairment. However, caregivers provide much more than this formal definition states. They often provide medical care including administration of medications, emotional and social support, and advice on medical decision-making. About 90% of men and 80% of women with PD have caregivers during their physician visits, and most caregivers are spouses.
Despite existing therapeutic support and resources for caregivers, there are several challenges to overcome. These include sex disparities in caregiving and the substantial financial strain that can be associated with caregiving. Caregivers are frequently at the forefront of providing medical history and administering complicated medication regimens without formalized education or support.
Also Check: Cleveland Clinic Parkinson’s Center Of Excellence
Other Reasons For Cognitive Symptoms
Besides PD, there are other important causes of cognitive dysfunction to keep in mind. Medical illnesses such as thyroid disease or vitamin B12 deficiency can cause cognitive symptoms. Urinary tract infections or pneumonia can acutely cause confusion or hallucinations. In these settings, the cognitive symptoms are generally reversible after the infection or medical condition is treated. One should be aware that some medications for pain or bladder problems may cause sedation/sleepiness or confusion, and, thereby, impair cognitive function.
Classification Issues And Prodromal Stages
The proposal that dementia prior to or simultaneous with motor symptoms can be included in the diagnostic criteria for PD, has reopened the long-standing debate on whether PDD and DLB should be considered the same disease,,,. A deeper understanding of the pathophysiological processes underlying these two synucleinopathies, such as the relative contribution of -amyloid and tau pathology in cortex and striatum, the extent of cortical Lewy pathology and -synuclein load in the hippocampus, the severity of neuronal loss in the substantia nigra, and cholinergic cell loss, is required to better understand the relationship between PD and DLB.
Although some risk factors for cognitive impairment have been identified,,, further research is needed to better identify any early evidence of cognitive impairment in genetic at-risk populations and in individuals with clinical features of prodromal PD to provide opportunities for prevention strategies and early precision therapy interventions.
Read Also: Utensils For Parkinson’s Patients
Understanding Thinking Changes In Parkinson’s Disease
In this 1-hour webinar listeners will learn key features of cognitive impairment in Parkinsons disease, including what symptoms may occur and why they may develop. Strategies for dealing with cognitive changes will be discussed, along with medications and potential research interventions in the field. An interdisciplinary approach regarding cognitive impairment in Parkinsons disease will be highlighted with the role of the movement disorders neurologist on the team.
Effects Of Exercise On Dendritic Spines
DA-depletion in the striatum leads to the loss of dendritic spines on striatal medium spiny neurons in both animal models and in PD. These morphological changes reflect the loss of synapses and hence reduction in neurotransmission not only in PD but a wide spectrum of brain disorders including Alzheimers disease and Fragile-X syndrome . Spine loss occurs predominantly on DA-D2R-containing MSNs of the indirect pathway, reflecting the dysfunction in neurotransmission in this circuitry , .
While an important question in exercise yet to be fully addressed in PD and its animal models, studies in healthy rodents subjected to different exercise paradigms have demonstrated experience-dependent increases in dendritic spine density in a number of regions including the hippocampus and cerebellum , . One hypothesis to be explored in models of PD is that exercise can reverse dendritic spine loss in DA-D2R containing striatal neurons.
You May Like: Which Part Of The Brain Is Affected By Parkinson’s Disease
Biomarkers Of Cognitive Decline
Many of the pathologies associated with cognitive impairment can be identified in vivo using a variety of imaging and blood-based or CSF-based markers. These biomarkers can be used to provide an increased understanding of the mechanisms underlying cognitive impairment in PD and, from a clinical perspective, can identify patients with an increased risk of early and rapid cognitive decline.
One of the first identified predictive markers was temporo-parietal atrophy on MRI , confirmed in many subsequent studies. In addition, basal forebrain atrophy observed using MRI is also associated with cognitive impairment in PD,. Hypometabolism in the medial frontal and parietal regions using FDG-PET is associated with a decline in executive and memory function. More recent MRI techniques, such as diffusion tensor imaging, also hold promise as biomarkers of cognitive function. For example, increased radial and axial diffusivity in the thalamus observed using diffusion tensor imaging was associated with a decline in MoCA scores.
Exercise And Blood Flow
Exercise increases blood flow in the healthy brain in a wide range of animal species undergoing various exercise regimens , . Thus exercise may facilitate neuroplasticity by influencing the vasculature of the central nervous system through angiogenesis and altered blood brain barrier permeability. The delivery of peripheral signaling molecules originating from muscle or adipose tissue including insulin, angiogenic factors such as vascular endothelial growth factor , hypoxia mediated factors such as hypoxia-induced factor 1 , leptin, and neurotrophic factors including BDNF can be promoted.
Don’t Miss: Wearable Technology For Parkinson Disease
Cognitive Decline In Parkinsons Disease: A Subgroup Of Extreme Decliners Revealed By A Data
- 1Neuro-Huvud Halscentrum, Region Västerbotten Hospital, Umeå, Sweden
- 2Umeå Center for Functional Brain Imaging, Umeå, Sweden
- 3Department of Integrative Medical Biology, Umeå University, Umeå, Sweden
- 4Department of Statistics, Umeå School of Business, Economics and Statistics, Umeå, Sweden
- 5Center for Demographic and Ageing Research, Umeå, Sweden
- 6Department of Radiation Sciences, Umeå University, Umeå, Sweden
- 7The Munich Center for the Economics of Aging, Max Planck Institute for Social Law and Social Policy, Munich, Germany
Social Cognition And Cognitive Decline In Patients With Parkinsons Disease
Published online by Cambridge University Press: 27 November 2020
- Laura Alonso-Recio*
- Affiliation:Departamento de Psicología, Facultad de Ciencias de la Salud y la Educación, Universidad a Distancia de Madrid, Madrid, Spain
- Fernando Carvajal
- Affiliation:Departamento de Psicología Biológica y de la Salud, Facultad de Psicología, Universidad Autónoma de Madrid, Madrid, Spain
- Carlos Merino
- Affiliation:Departamento de Psicología Biológica y de la Salud, Facultad de Psicología, Universidad Autónoma de Madrid, Madrid, Spain
- Juan Manuel Serrano
- Affiliation:Departamento de Psicología Biológica y de la Salud, Facultad de Psicología, Universidad Autónoma de Madrid, Madrid, Spain
- *
- Correspondence and reprint requests to: Laura Alonso-Recio, Departamento de Psicología, Facultad de Ciencias de la Salud y la Educación, Universidad a Distancia de Madrid. Camino de la Fonda, 20, 28400 Collado Villalba, Madrid, Spain. Tel.: +34 918561699 . Email:
Read Also: Parkinson’s Disease And Driving
Cognitive Impairment In Parkinsons Disease
Cognitive impairment is a common non-motor symptom of Parkinsons disease and causes significant disability to patients and burdens for caregivers. Similar to motor symptoms, the characteristics of cognitive impairment in Parkinsons disease can be quite variable, both in terms of what cognitive domains are impaired and the timing of onset and rate of progression.
Prevalence And Natural History Of Pd Dementia: Near
Clinical features of cognitive impairment in PD involve a wide range of cognitive domains, including executive function, visuospatial reasoning, memory, and language function, and can include additional features including visual hallucinations, paranoia, and fluctuations in attention. PD is often marked primarily by visuospatial and executive deficits, in contrast to Alzheimer disease , where memory impairment predominates. Cognitive impairment in PD encompasses a spectrum of severity from relatively mild symptoms to end-stage dementia. Despite the controversy surrounding the nomenclature and clinical significance of the term mild cognitive impairment , careful characterization of early symptoms is needed for both research and clinical purposes, and formal criteria for diagnosis of MCI in PD have been established.
Overall prevalence of PD-associated dementia is approximately 25%30% of total PD cases, and increases dramatically with advancing age. While some patients with PD survive a decade or more before developing dementia, others experience cognitive impairment shortly after, or concurrent with the onset of motor symptoms, leading to the arbitrary distinction of patients who develop dementia within 1 year of parkinsonism as having dementia with Lewy bodies .
Also Check: How To Care For Someone With Parkinson’s Disease
Psychiatric & Cognitive Complications In Parkinsons
Depression, anxiety, cognitive decline, psychosis and impulse control can be common in people with Parkinsons. They affect quality of life for both people with Parkinsons and care partners. In this webinar Dr Daniel Weintraub discusses these issues, the correlation between mood, motor function and Levodopa levels, and more. Registration is required, but it is free.
Biomarkers: An Ongoing Quest For Molecular Fingerprints
PD remains a clinical diagnosis, with only one commercially available biomarker approved to distinguish PD from essential tremor, although the value of this biomarker compared to longitudinal follow-up with a movement disorders specialist is unclear. Neurologists, even experienced movement disorders specialists, are frequently inaccurate in distinguishing idiopathic PD from other parkinsonian syndromes, especially early in the disease course. Predicting the risk and timing of dementia in patients with PD is equally challenging and is complicated by the heterogeneity of molecular neuropathology observed in PDD cases when autopsy examination is used as a gold standard. While multiple studies support a direct relationship between the presence of cortical Lewy pathology and cognitive impairment, some patients with PDD have very few cortical Lewy bodies., Conversely, extensive cortical Lewy pathology is occasionally seen in cognitively normal patients with PD and even individuals without PD., These observations suggest that -synuclein is not solely responsible for cognitive impairment in PD. Multiple studies have documented the presence of concomitant -amyloid in approximately 60% of patients with PD with dementia, as well as tau pathology in a smaller subset, underscoring the need for accurate biomarkers to define molecular disease signatures prior to autopsy, ideally in presymptomatic or early symptomatic phases.
Don’t Miss: Leg Weakness Parkinson’s Disease
Latent Class Analysis Identifies A Sub
Fitting of a MLCLMM to the cognitive data suggested that longitudinal cognitive decline in the patient sample was best described by two latent groups ). The two-class solution split the sample into one larger subgroup with 90% of the PD participants and one smaller subgroup, with 10% of the participants . The worse-fitting three-and four-class solutions further divided the larger group but retained the smaller subgroup.
Table 2. Number of follow-up visits by class, in percent.
Plotting of the mean performance scores for each cognitive domain, timepoint, and both classes in Figures 1AC shows that the smaller patient class was characterized by performance deficits within 1SD of the larger class at baseline but then showed rapid linear decline over time.
Figure 1. Mean performance at each timepoint by class and cognitive domain. Fitted lines are for a linear model regressing time against cognitive performance for each class.
Fitting linear mixed effects models with fixed effects of time, class, and time*class in the patients confirmed significant effects of class and a highly significant time*class interaction for each cognitive domain . HC were added as a single control group after confirming with a separate multivariate latent class mixed model that cognitive decline across domains was best described as one group for HC , loglik=2296.67, and 37 parameters).
Table 3. Baseline characteristics of PD patients by class and healthy controls.
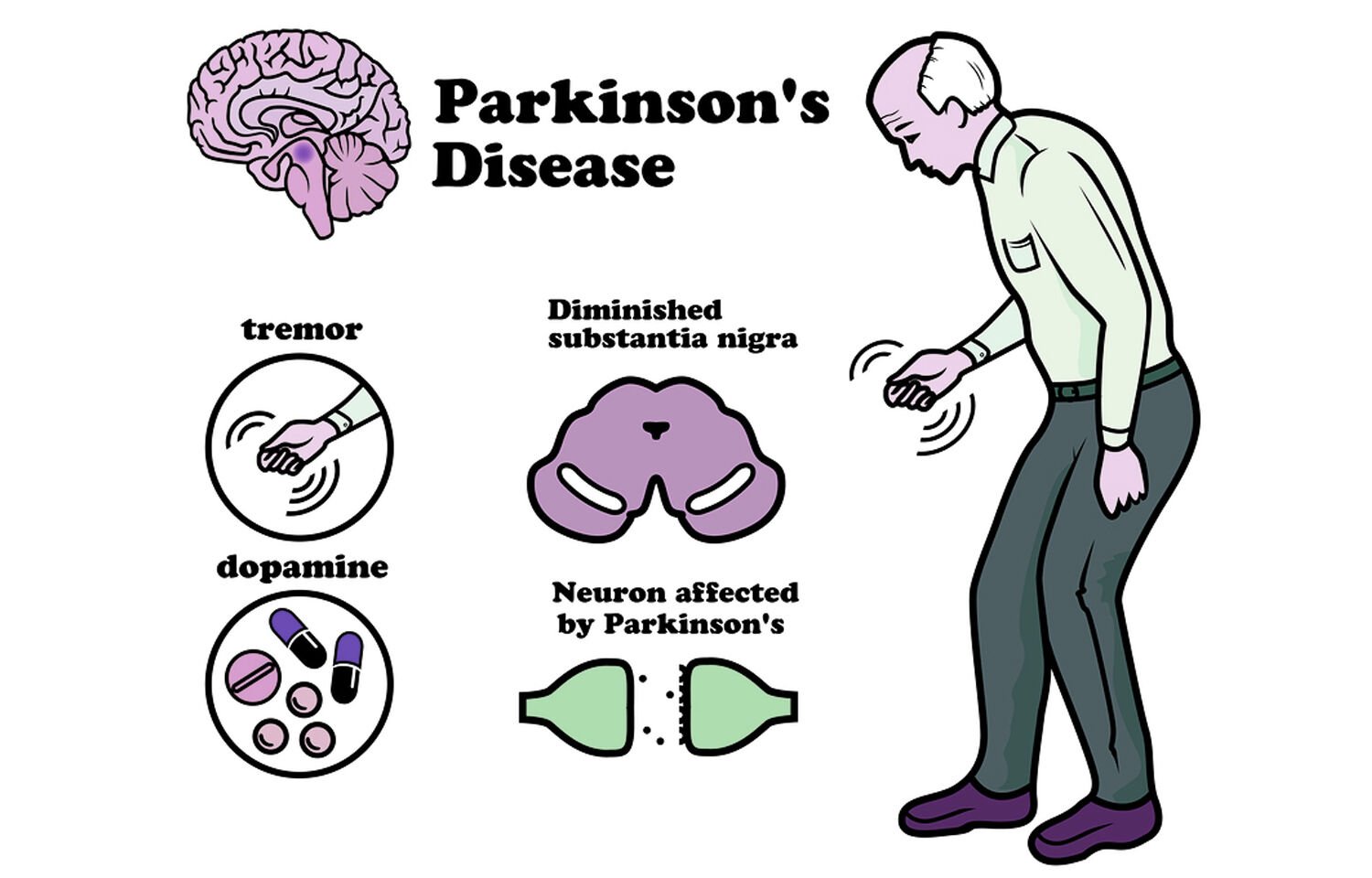
Introduction And The Motor Problem In Parkinsons Disease
Parkinsons disease is a progressive neurodegenerative disorder that is characterized by the loss of dopamine due to the degeneration of substantia nigra pars compacta dopaminergic neurons. Characteristic features of PD include motor and cognitive impairment , as well as mood disorders. In healthy individuals, motor performance is dependent on the interaction between unconscious and volitional control of movement , . Conversely, in PD, the early and preferential loss of DA in the dorsal basal ganglia leads to diminished automatic and increased cognitive control of motor movements. Consequently, individuals with PD must handle and sustain a larger cognitive load to execute either motor or cognitive tasks, . DA replacement therapy alleviates some motor features of PD, but with less beneficial effects observed on cognitive function . In the last decade there is mounting evidence for the role of exercise in improving motor performance that may include facilitating both the cognitive and automatic control of movement.
You May Like: All About Parkinson’s Disease
Demographics And Clinical Variables
To identify early markers of different cognitive trajectories, a number of demographic, clinical variables and biomarkers were used to compare patient sub-groups at baseline . Demographics included age, sex, and education in years. To evaluate motor impairment in the patients, The Movement Disorders Society Unified Parkinsons Disease Rating Scale part III was used . A mean tremor score and a mean postural instability and gait difficulties score were calculated from the respective items. Scores for a tremor dominant subtype and an akinetic-rigid subtype were then calculated according to the criteria: If mean tremor score/PIGD score1.15, OR if PIGD score=0 and Tremor score> 0, then subject is TD. If ratio0.9, then subject is PIGD . As an indicator of disease stage/severity, the Hoehn and Yahr stage was included . Part II total score of the MDS-UPDRS was used as an additional indicator of motor problems in daily living. Disease duration was calculated as the number of months between diagnosis and enrolment into the study.
Prodromal Pd Phenotypes And Conversion
Recent evidence suggests that individuals with prodromal features of PD, such as hyposmia , REM sleep behaviour disorder and reduced dopamine transporter binding, may present with worse cognitive performance compared with people without any or with only one of these features,,. Interestingly, prodromal PD and DLB may overlap and it is not yet known how to distinguish between those who will develop PD versus those who will develop DLB. Of note, cognitive deficit has been recently defined as a new prodromal marker and has been included in the last update of the research criteria for prodromal PD.
Read Also: Parkinson’s Multiple System Atrophy
Mci And The Risk Of Pd Dementia
The two most common cognitive syndromes in patients with PD, PDD and PD-MCI, were operationally defined in diagnostic and assessment guidelines from the International Parkinson and Movement Disorder Society ,. In PDD, but not in PD-MCI, the cognitive deficits are severe enough to impair daily life , independently of the impairment ascribable to motor or autonomic symptoms.
Among PD patients without dementia, approximately 2530% have MCI, which is evident at the time of diagnosis in 1020% of patients. Presence of MCI is associated with a shorter time to progression to a dementia diagnosis, although considerable variability is observed, with some patients remaining stable and some even reverting to normal cognition. For example, in one study of patients with early PD, over 20% of those with MCI reverted to normal cognition after 1 year, although persistent MCI was associated with a much lower remission rate.