Management Of Psychosis In Parkinson Disease
Sam Adler, MDPsychiatric Times
For some patients with Parkinson disease, the neuropsychiatric complications are a greater source of morbidity than the motor dysfunction. This article focuses on the management of psychosis in Parkinson disease.
The diagnosis of Parkinson disease is based on the observation of a constellation of motor abnormalities and the exclusion of other secondary causes of parkinsonism. The disease is classified as a movement disorder, but for many patients with PD the motor problems are only the tip of the iceberg. A host of neuropsychiatric disorders are intrinsic to PD or occur as a complication of the dopaminergic therapies or anticholinergic medications used to treat the motor symptoms . For some patients with PD, the neuropsychiatric complications are a greater source of morbidity than the motor dysfunction.1,2
The neuropsychiatric disorders associated with dopaminergic therapies are important to recognize, because they are at least partially iatrogenic and can often be successfully managed by adjustment of the patients PD medications. This article focuses on the management of psychosis in PD-a problem with significant morbidity. Psychosis in PD and Parkinson-related disorders is an independent predictor for the need for institutionalization and increased mortality.
Susceptibility to psychosis
Pros and cons of pharmacological treatment
Fluctuating motor symptom responses
You May Like: Weed Killer Linked To Parkinsons
Do Hallucinations Go Away
Some visual hallucinations are so mild they might not even register on a conscious level, Dr. Ramdhani says. For instance, you may see a shadow thats not there, or glimpse something in your peripheral vision that clears when you turn your head. For some people, those may go away on their own, especially with a change in medication. In more advanced stages, though, these hallucinations may occur along with delusions, which means a false belieflike thinking your spouse isnt your real partner. Dr. Ramdhani says this can happen due to cognitive impairment, such as dementia.
Management Of Visual Hallucinations In Pd
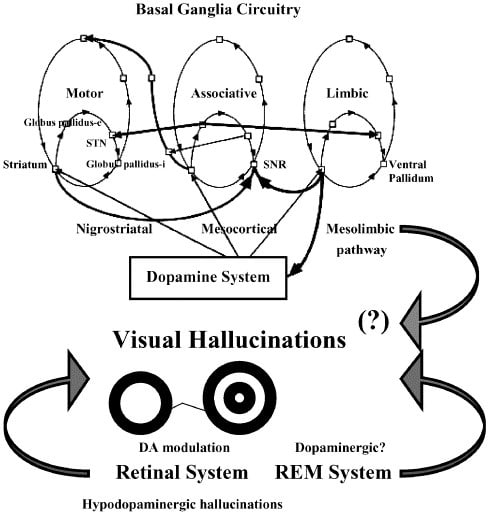
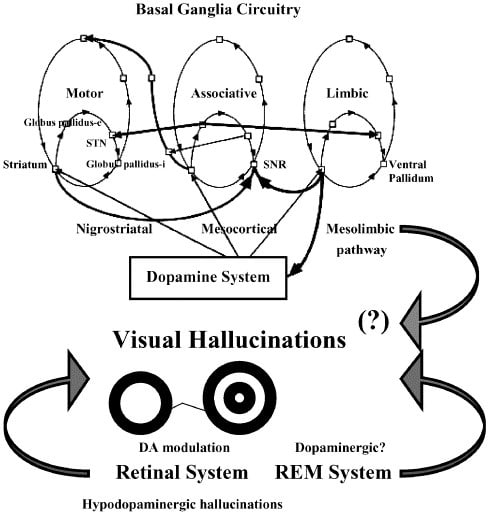
Understanding the complex interactions between neurotransmitter systems in the context of neurodegeneration secondary to PD assists in efforts to treat psychotic symptoms as they arise. Management is complex and varies between patients. The first consideration should most obviously be prevention. When these symptoms occur acutely, systemic illness should be considered and treated. When symptoms persist, an increasing array of treatment options are available and can be tailored to the individual patient. A treatment algorithm is presented in .
FIGURE 1. Management flow chart for visual hallucinations in Parkinsons diseasea
a COMT=catechol-O-methyltransferase.
Recommended Reading: Cleveland Clinic Parkinson’s Center Of Excellence
Risk Factors For Parkinsons Psychosis
Understanding the risk factors for hallucinations and delusions can help you recognize symptoms of Parkinsons psychosis. The following factors may increase the likelihood of experiencing hallucinations and delusions:
- Advancing cognitive impairment, including worsening memory loss
- History of depression
- Sleep disorders and sleep disturbances
- Changes to medications
- Worsening medical conditions outside of Parkinsons
We have noticed that when my father had delusions, its been when his general health is not good, or when he has been in the hospital for PD-related issues, a MyParkinsonsTeam member commented.
Questionnaires used in a clinical setting can help assess the risk of developing hallucinations or delusions, or establish that they are occuring. These include:
- PD nonmotor symptom scale
- Parkinson Psychosis Questionnaire
- Scale for Evaluation of Neuropsychiatric Disorders in Parkinsons Disease
Individuals with Parkinsons or their caregivers can speak with a neurologist to understand if any of these tools would be helpful in their particular situation.
What To Do About Parkinsons Hallucinations
Hallucinations or other signs of Parkinsons psychosis should be discussed with a doctor. Depending on the cause and severity of hallucinations, the person may or may not need treatment. If an infection is the cause, it should be treated accordingly. A doctor may want to change or reduce the dosage of any medications that could cause hallucinations to stop Parkinsons psychosis.
In mild cases of hallucinations, the person may be aware that the images are not real. In these cases, if the hallucinations are not causing any distress, pharmaceutical treatment may not be necessary. Sometimes improved lighting in darkened or shadowy areas may help reduce occurrences.
Sometimes the person may not realize he or she is hallucinating. In these cases, especially if the hallucinations are severe and disturbing, a doctor may recommend adjustments to the persons current Parkinsons medications. However, this could potentially worsen movement-related Parkinsons symptoms. If these symptoms affect the persons quality of life, a doctor may instead recommend antipsychotic drugs, particularly clozapine or quetiapine, which typically help reduce hallucinations without affecting other Parkinsons symptoms.
Recommended Reading: Parkinson’s Getting Out Of Chair
Selfcare For The Person With Parkinsons
- Join a Parkinsons support group if you dont already belong to one. Talk about your experiences, ask for help if you need it and share whats worked and not worked for you.
- Offer to have coffee with someone you know has been newly diagnosed and offer them support and encouragement.
- Make time to exercise and get out in nature every day.
- Communicate frequently with your doctors and discuss the possibility of tweaking your medications if your symptoms become worse.
- Rest when you need it.
- Plan a day trip or a vacation and get away from your normal surroundings.
- Take control where you can and keep authoring your own story.
- Practice meditation or yoga or tai chi to relax and calm your mind.
- Start a new project that youre excited to work on every day.
- Communicate with your care partners and let them know how they can best help you.
Managing Hallucinations And Delusions
Get medical advice. In mild cases simple monitoring may be all that is required. In more severe cases changes in medications may be necessary.Rule out other causes such as eyesight issues or infections.Talk to your family and or carers to help them understand how you are feeling. It can help them to be more patient and supportive with you too.Try not to worry.Reassure yourself that these symptoms may be a side effect of Parkinsons medication.Seek counselling. People with Parkinsons, carers and family members may need support, counselling and specific advice. Medicare covers 6 – 12 sessions with a psychologist to provide a range of strategies to help.
Support for you
Don’t Miss: Ot Interventions For Parkinson’s Disease
How Are They Treated
Your medical team should be aware of non-motor issues, just like your physical symptoms. Internists, neurologists, and psychiatrists together can help determine the right course for each person.
There are antipsychotic medications that are safe and can help to reduce the symptoms of Parkinson’s disease psychosis, but there are even more antipsychotics that are contraindicated for PD.
Let a medical provider know you have Parkinson’s when seeking emergency care or treatment for something by doctors who are not a part of your regular medical team.
There is only one drug, pimavanserin, approved in 2016 by the FDA specifically for PD. It has a mechanism of action that doesn’t block dopamine. This has made it a safer drug for people with Parkinson’s.2
Two other medications, quetiapine and clozapine, that have been used for a longer time, are also considered safe for treating hallucinations and delusions in people with PD.2
Predictive Factors And Pathophysiology
Minor hallucinations/illusions
Patients with isolated minor hallucinations/illusions differed from patients without hallucinations only by the presence of more depressive symptoms on the CES-D rating scale, suggesting that depressive symptoms are a facilitating factor. Indeed, depression may sometimes trigger or aggravate hallucinations associated with deafness or ocular pathology . However, when we analysed depression according to CES-D cut-off scores, the difference between the Parkinson’s disease patients with minor hallucinations/illusions and those with no hallucinations was not significant. Interestingly, hallucinations involving the deceased spouse have been reported in up to half of widowed persons, with a higher frequency in the elderly . In the present study, the `presence’ was that of a deceased relative in only three cases bereavement cannot therefore explain the bulk of the cases.
Dopaminergic agents and other treatments
In the present study, non-hallucinators were more likely to be on anticholinergics or selegiline than patients with hallucinations. A similar paradoxical, negative association between anticholinergics and hallucinations was found by Sanchez-Ramos and colleagues . This reflects the recommendation whereby the use of these drugs in patients with cognitive impairment is avoided because of the well-known risk of cognitive worsening and/or hallucinations in this population.
Cognitive impairment
Sleepwake disturbances
Motor status
Depression
Recommended Reading: Signs Of Parkinson Disease Early Symptoms
Tips For Living With Hallucinations
It is important for people with PD to talk about hallucinations with their family and care team these are manageable and can be troublesome if not treated. Discuss all possible symptoms with your doctor, no matter how minor, rare or bizarre you may think they are.
What Are The Symptoms Of Psychosis
Two of the most prominent symptoms are hallucinations and delusions.7 Hallucinations involve seeing, hearing, experiencing or sensing things that are not really there. Delusions are false beliefs that are not based in reality. In describing symptoms of Parkinsons disease psychosis, patients may use such common terms as: seeing things, paranoia, flashbacks, nightmares, false beliefs, or not being in touch with reality.8
You May Like: Drinking And Parkinson’s Disease
Demystifying Hallucinations Night Terrors And Dementia In Parkinsons
This two-hour webinar includes extensive discussion about hallucinations, delusions, illusions and other examples of Parkinsons psychosis in Parkinson’s. Presenters: Rohit Dhall, MD, MSPH and Vergilio Gerald H. Evidente, Director, Movement Disorders Center of Arizona in Scottsdale. Pay particular attention to Dr. Rohit Dhalls description of the causes of PD psychosis as well as treatment options and what to discuss with your movement disorder specialist. Dr. Evidente gives a clear description on differences in PD dementia, Alzheimer’s and other dementias.
What Are The Treatment Options For Parkinsons Psychosis
Because Parkinsons drugs can cause psychosis, your doctor will likely start by taking you off your medications, one at a time, or adjusting the dose. Changing your medication may make your movement symptoms worse.
Your doctor will keep adjusting your medication. The goal is to get you to a dose that improves your movement without causing hallucinations and delusions.
If changing your medication doesnt work, the next step is to go on an antipsychotic medication. These drugs prevent psychosis symptoms by altering levels of chemicals in your brain.
Older antipsychotic drugs can make Parkinsons movement symptoms worse. Newer drugs, called atypical antipsychotics, are less likely to affect your movement. These drugs are off-label, meaning theyre not approved to treat Parkinsons specifically. They include:
In 2016, the Food and Drug Administration approved pimavanserin . Its the first drug designed specifically to treat Parkinsons disease psychosis. Nuplazid reduces the number of hallucinations and delusions without affecting movement.
Nuplazid and other newer antipsychotic drugs do carry a black box warning. They can increase the risk of death in older people who have psychosis related to dementia. Your doctor will consider this and other risks before prescribing one of these drugs.
Read Also: Speech Devices For Parkinson’s
Parkinsons Disease Psychosis: Hallucinations Delusions And Paranoia
As part of Parkinsons Disease and its treatment, hallucinations, illusions, delusions, suspiciousness and paranoid behaviors occur in over 50% of patients. In this 1-hour webinar Dr. Christopher Goetz suggests lifestyle changes, medication adjustments and a recently FDA approved drug to specifically treat psychosis in Parkinsons Disease.
Bringing Light To Darker Side Of Parkinsons
Often the hardest part of Parkinsons disease psychosis is the fear of the unknown. As a person with Parkinsons, you may worry about having hallucinations and/or delusions and not being able to do anything about it. As a care partner, you may worry that you wont be able to help your person with Parkinsons feel safe if something does happen.
The good news is you now have information on what Parkinsons disease psychosis is the risk factors to look out for biological and environmental triggers that can bring them on and how to manage them if they show up.
But what about the emotional toll these types of symptoms can place on you over the long-term as the person with Parkinsons or as a care partner?
The diagnosis of a chronic illness in and of itself requires a lot of adjustments. When you add something like Parkinsons disease psychosis into the mix, its important that you also add another level of self-care to your everyday life.
Also Check: Sinemet Dosage For Parkinson’s
How Can I Help My Loved One
Your loved ones hallucination episodes are certainly disturbing, but they are usually harmless. Unlike hallucinations caused by other neurodegenerative diseases, hallucinations associated with Parkinsons disease are most often benign.
Not all hallucinations need to be treated. If they do not disrupt your loved ones daily life, there are ways to manage them well. It is still important to inform your neurologist for proper follow-up.
Talk to your loved one about their hallucinations. Together, determine what you can do when they are having a hallucination. This will help both of you be prepared and reassured when it happens.
If the hallucinations are severe, do not tell your loved one that the hallucinations are not real. This will only increase the disparity between reality and the hallucination. It may also create unnecessary conflict with your loved one who is convinced that they are hallucinating.
How Can Caregivers Support Their Loved Ones
Caring for someone who sees, hears, or believes things that arent real can be very difficult. Try to be as patient and calm as you can.
Avoid arguing with the person. If they still have insight, gently explain that what theyre seeing isnt real. Tell anyone who cares for or visits your loved one what to expect, and how to respond.
Stay in close contact with the persons doctor. If their symptoms dont improve, ask whether they need a medication adjustment.
Check whether the person needs hearing aids or glasses. Poor hearing or vision can sometimes lead to hallucinations. It can also help to turn on bright lights at night, to prevent the shadows that may trigger visual illusions.
Secure any dangerous objects, and keep pathways in the home clear to prevent falls and injuries. If you ever feel like the person is a risk to themselves or others, call their doctor.
Read Also: Acupressure Points For Parkinson’s Tremors
Phenomenology Of The Hallucinations
Minor hallucinations/illusions
We grouped together in this category three types of phenomena. The most frequent type was presence hallucinations . The patient had the vivid sensation of the presence of somebody either somewhere in the room or, less often, behind him or her. In all cases, the presence was that of a person, and in one case it was also occasionally the presence of an animal . In seven cases, the presence was that of a relative . In all the other cases the presence was unidentified. The presence hallucinations were commonly as vivid as a hallucinated scene and were described as a `perception’. For instance, one patient said: `the image is behind me’, a second said: `I see someone arriving I turn back but nobody is there’, a third said: `I take a look I don’t see anything, but it is engraved in my mind’, and another said: `I have the impression that my mother is always there, that she is about to come into sight’. The passage hallucinations consisted of brief visions of a person or an animal passing sideways. If an animal was seen, the species was almost invariably specified , and in two instances it was a dog previously owned by the patient. Illusions occurred in nine patients . In five cases the illusion consisted of the transformation of an object into an animal .
Case 1 .
Case 2 .
Formed visual hallucinations
Case 3
Auditory hallucinations
Case 4
I Had A Hallucination: What Next
Research has shown that for many people with PD who have them, hallucinations begin after a change in medication, more specifically, an increase in levodopa . Additional factors make a person more likely to experience hallucinations when medications are changed, such as other cognitive problems or memory issues, depression and sleep problems. Dementia|A term used to describe a group of brain disorders that cause a broad complex of symptoms such as disorientation, confusion, memory loss, impaired judgment and alterations in mood and personality.] also increases the risk of hallucinations and delusions when PD medications are changed. Dementia means cognitive changes whether in memory, judgment or attention that interfere with daily life.
One thing that does not affect the risk of hallucinations is your regular dose of levodopa. Rather, studies show that it is a change in dose an increase in a dose that has been stable that sets off hallucinations.
Tip: Experiencing a hallucination does not mean you are going crazy. Many people recognize that their hallucinations are not real. Do not react to these visions or sounds or engage them dismiss them. Bring up the topic with your doctor immediately.
Recommended Reading: Can Anxiety Cause Parkinson’s Disease
A Caregivers Guide To Parkinsons Disease Psychosis
While more than 50% of those taking carbidopa-levodopa may experience psychosis , medication management of these symptoms is a balancing act. First, families must bring psychotic behavior to the attention of your medical team. Medical causes of the behavior, like infection must be ruled out, followed by a review of medications and possible medication adjustments before a lifestyle changes and possible medications for treatment are added.
Hallucinations According To The Duration Of The Disease

We found that the prevalence of hallucinations of all types and of visual hallucinations in the 3 months preceding inclusion in the study increased with the duration of the disease. Moreover, the duration of Parkinsons disease was an independent predictor of visual hallucinations in the multivariate analysis. Other studies gave conflicting results on the relationship between hallucinations and disease duration. In a retrospective study of 100 patients, logistic regression analysis also showed an association between `psychosis and an increased duration of the disease . An association between the duration of the disease and the occurrence of hallucinations was also found by some investigators but not by others .
Table 1
Don’t Miss: Glutathione Injections For Parkinson’s