Behaviors Seen In Parkinsons Disease Dementia
As dementia progresses, managing disorientation, confusion, agitation, and impulsivity can be a key component of care.
Some patients experience hallucinations or delusions as a complication of Parkinsons disease. These may be frightening and debilitating. Approximately 50 percent of those with the disease may experience them.
The best thing to do when giving care to someone experiencing hallucinations or delusions from Parkinsons disease dementia is to keep them calm and reduce their stress.
Take note of their symptoms and what they were doing before they exhibited signs of hallucinating and then let their doctor know.
This element of the disease can be particularly challenging for caregivers. Patients may become unable to care for themselves or be left alone.
Some ways to make caregiving easier include:
- sticking to a normal routine whenever possible
- being extra comforting after any medical procedures
- limiting distractions
- using curtains, nightlights, and clocks to help stick to a regular sleep schedule
- remembering that the behaviors are a factor of the disease and not the person
Children Near Airports May Be Exposed To Dangerous Levels Of Lead
A new paper in PNAS Nexus finds that children living near one California airport have higher lead levels in their blood. Since leaded gasoline is still used by piston-engine aircraft all around the United States, it appears children are still being exposed to toxic lead levels. This is despite policymakers’ efforts to reduce lead exposure since the 1970s.
Over the last four decades, the blood lead levels of children in the United States have declined significantly due to policies that removed lead from paint, plumbing, food cans, and automotive gasoline. Scientists generally agree that the phase-out of tetraethyl lead from automotive gasoline under provisions of the Clean Air Act of 1970 was the most effective of these policies.
But leaded gasoline hasn’t disappeared entirely. It remains a standard part of aviation gasoline and is used by an estimated 170,000 piston-engine aircraft nationwide. Today, the use of lead-formulated aviation gasoline accounts for as much as two-thirds of lead emissions in the United States.
The U.S. Environmental Protection Agency estimates that four million people reside within half a mile of an airport servicing piston-engine planes. About 600 elementary or secondary schools are located near such facilities.
More information:PNAS NexusJournal information:
What Is Aggressive Parkinsons Disease
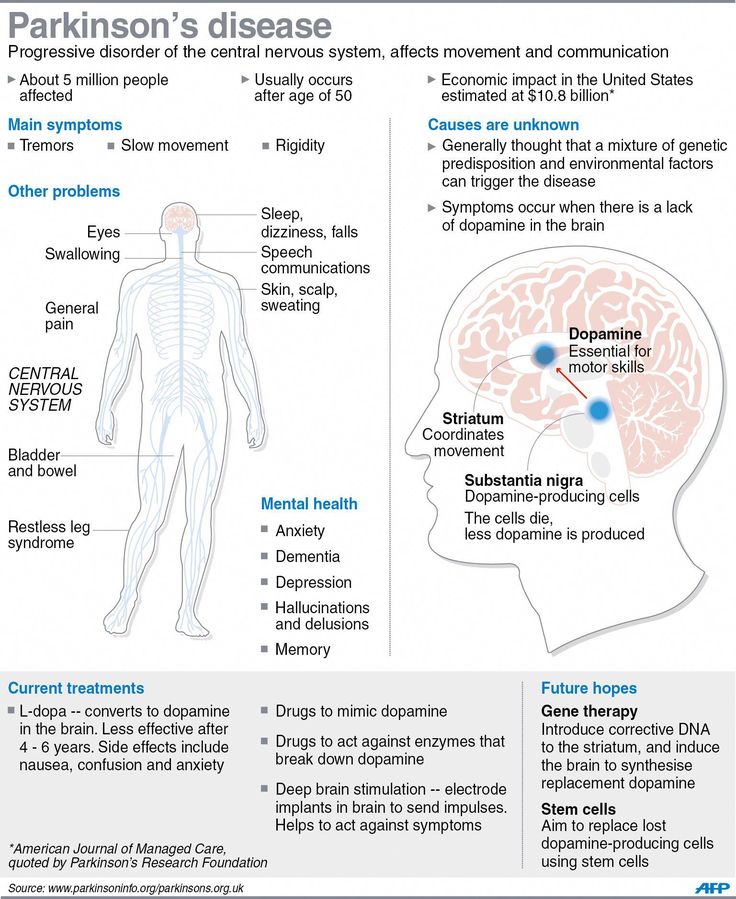
As written above, Parkinsons dementia aggression is that form of Parkinsons which makes the patient exhibit aggressive behavior. They vent out their aggression either verbally or physically, in the various forms that have been written above. Besides verbal and physical outbursts, PD Dementia patients are also prone to hallucinating caused by the medication administered. Hallucinations in PD Dementia patients primarily occur because of the effects of dopaminergic agents for motor symptoms.
Loss of dopamine neurons in the ventral tegmental area is one of the likeliest of all neuropathological causes as changes in serotonin and norepinephrine systems are not. For the uninitiated, the ventral tegmental area is the origin of the mesolimbic dopaminergic projection. Plenty of studies have gone into analyzing the cause behind the aggression in PD Dementia patients. Depression in PD Dementia patients has been identified due to changes in the medial frontal cortex and the anterior cingulate. Akinetic-rigid variants have been found in patients showing signs of major depression.
Recommended Reading: Activities For Elderly With Parkinson’s Disease
Management Of Dementia In Parkinsonism
There is some evidence that cholinesterase inhibitors may have antipsychotic properties for the management of behavioral symptoms in Parkinsonism. A number of open-label studies have documented the beneficial effects of donepezil and rivastigmine in the management of dementia in Parkinsonism. A large placebo-controlled study of rivastigmine found that the rivastigmine group had significant improvement of the neuropsychiatric symptoms than the control group and were less likely to develop hallucinations. Furthermore, patients who suffered from visual hallucination at the time of initiation of treatment benefited the most.
The management of psychosis in DLB is equally frustrating and only a prospective randomized study in this regard has been reported to date. Rivastigmine led to significant improvement in delusions, hallucinations, depression, and apathy and therefore, cholinesterase inhibitors are now recommended as the first line of management for this condition. Mementine has also been found useful in one small retrospective study. However, cholinesterase inhibitors can increase tremor in Parkinsonism by their procholinergic actions.
One of the major problems of management of psychosis and related problems in Parkinsonism is that stopping drugs often lead to worsening of symptoms. However, some trials show that patients can be switched from clozapine to quetiapine after stability has been earned, provided they responded earlier to the latter agent.
Parkinson’s Disease And Dementia
Parkinson’s disease and dementia are both progressive conditions that get worse over time. They are also both far more common among the older population:
What’s more, a person with Parkinson’s disease may have a higher chance of developing dementia at some stage. It’s thought that this happens in roughly half of all people with Parkinson’s. Results of studies that tracked patients over 10 years and eight years respectively suggest that dementia is diagnosed in between 30% and almost 80% of people with Parkinson’s.
Yet, it’s important to understand Parkinson’s and dementia as two different degenerative conditions:
- They don’t have the same primary causes or primary symptoms.
- It’s common to develop one without the other.
You May Like: First Stages Of Parkinson’s
Parkinsons And Lewy Body Disease
Lewy body disease occurs when there is an abnormal build-up of a protein called alphasynuclein in the brain. Depending on where the proteins accumulate, Lewy body disease can lead to impairments in movement, thinking and behaviour.
Lewy body disease includes three overlapping disorders:
- Dementia with Lewy bodies
- Parkinsons disease dementia
This overlap results in the disease being called a spectrum disease.
In people with Parkinsons a large number of Lewy bodies appear in an area of the brain known as the substantia nigra. This area of the brain is responsible for movement, so the Lewy bodies are likely to cause impairments in movement.
Some people may go on to develop dementia with Lewy bodies. In this form of the disease, the clumps of protein occur in the cortex . This part of the brain is responsible for many cognitive processes, so the Lewy bodies are likely to result in cognitive impairments like those described under the heading above. It can result in symptoms similar to those seen in Alzheimers.
What’s The Difference Between Memory Loss And Parkinson’s Dementia
Alzheimer’s disease and PDD can both affect a person’s memory, but not in the same way.
Generally speaking, PDD is not associated with the sort of memory loss that comes with Alzheimer’s disease. PDD doesn’t typically impact a person’s ability to absorb and store new memories or information the way Alzheimer’s does.
“You can learn , but it’s difficult to retrieve the information that you have in your brain,” Irene Litvan, MD, director of the Movement Disorder Center at the University of California, San Diego, told Health. “You may not know where the cassette is, but if somebody asks you, ‘Where were you when you lost it?’ You can say, ‘Oh, I was there.'”
That’s not to say PDD doesn’t affect memory. Some people with Parkinson’s dementia do indeed experience short- and long-term memory loss. They might forget how to perform simple tasks, such as how to run the dishwasher. And since Parkinson’s disease can affect people in different ways, there’s no way to tell whether someone with Parkinson’s disease will experience memory loss.
Read Also: Parkinson’s Disease Foundation Grants
How Can We Manage Hallucinations
It may not be necessary to treat all hallucinations of a person with PDD. Hallucinations are often harmless, and it is okay to allow them to happen, as long as they are not disruptive or upsetting to the person or surroundings. Sometimes, recognizing the hallucination and then switching the topic might be an efficient way of handling frustrations that occur because of a hallucination. If hallucinations need medical treatment, your provider may be able to discuss and suggest some options. However, many of the medications used to treat hallucinations may make movement symptoms worse.
How Can We Support The Sleep/wake Cycle Of Pdd
For people with PDD who are confused about the day-night cycle, some daily strategies can be helpful. At night, starting a lights out routine that happens at the same hour every day, where all curtains are closed and lights are turned off, can help the person understand that it is sleep time. During the day, opening the curtains, allowing the person with PDD to spend as much time in the daylight as possible, avoiding naps, and organizing stimulating activities, can be helpful. Having lots of calendars and clocks in every room might also help a person with PDD be less confused about the time of day.
You May Like: Occupational Therapy For Parkinsons Disease
Do You Die From Pd Dementia
People with Parkinsons-related dementia often want to know how the disease can impact their lifespan. While people with Parkinsons can expect a similar lifespan to the general population, studies show both Parkinsons disease dementia and Lewy body dementia can shorten lifespan, generally due to medical complications from the disease, rather than the disease itself.
The Differences Between Parkinsons Dementia And Alzheimers Disease
The advanced cognitive changes that impact daily living in Alzheimers and Parkinsons are both types of dementia.
Parkinsons disease dementia can occur as Parkinsons advances, after several years of motor symptoms. Dementia with Lewy Bodies is diagnosed when cognitive decline happens first, or when Parkinsons motor symptoms and cognitive decline occur and progress closely together.
Alzheimers, a fatal brain disease, causes declines in memory, thinking and reasoning skills. Physicians can diagnose Alzheimers. Visit the Alzheimers Association to learn the 10 signs of Alzheimers disease.
Parkinsons disease dementia tends to be less disabling than Alzheimers disease. People with Alzheimers disease have language difficulties earlier than people with Parkinsons, and they are unable to form new memories unlike in PD.
Also Check: Foods Not To Eat With Parkinson’s Disease
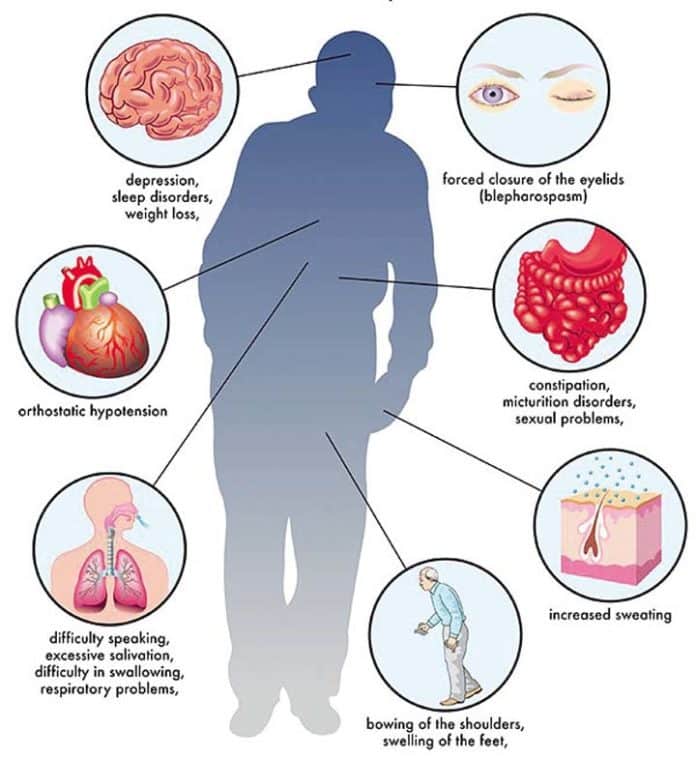
Signs And Symptoms Of Parkinson’s Disease
The primary symptoms of Parkinsons disease are:
Tremors or shaking often occur in the hands, fingers, forearms, feet, mouth, or chin. Typically, the tremor appears when your limbs are at rest as opposed to when youre moving. Some people notice that their tremor is exacerbated by stress and excitement.
Slowed movement . You may find that your ability to move freely and spontaneously is reduced or slowed down. Repetitive movements can be especially difficult, causing problems with everyday tasks like buttoning a shirt, brushing your teeth, or cutting food. You may start to walk with short, shuffling steps, or your feet may start to drag.
Rigidity, or muscle stiffness, may occur in any part of your body . This can limit your range of motion and cause muscle pain that gets worse when you move.
Poor balance, or the tendency to be unstable when standing upright, is one of the most important signs of Parkinsons. It happens because of the loss of reflexes needed for maintaining posture. Some people develop a tendency to sway backwards when standing or turning, which can result in backwards falls.
Tip : Whatand Howyou Eat Can Make A Difference
Theres no specific Parkinsons disease diet, but by adjusting your eating habits, you can help protect your brain. Diets that are good for your heart tend to also be good for brain health. Eating habits such as those promoted in the Mediterranean diet can help reduce inflammation, protect neurons, and promote better communication between brain cells.
Primarily, its important to eat plenty of fruit and vegetables, cut down on sugary foods and refined carbs, reduce fried and processed foods, and boost your intake of healthy fats and home-cooked meals. High protein meals may also help to benefit your brain chemistry.
Recommended Reading: Herbal Remedy For Parkinson’s Disease
What Is Parkinson’s Disease Dementia
Parkinsons disease dementia is a brain disorder that occurs in somebut not allpeople living with Parkinsons disease. The brain cell damage caused by the disease can lead to a loss of memory and other cognitive functions such as problem solving and speed of thinking. These changes in thinking and behavior can impact your daily living, independence, and relationships.
In those who do develop Parkinsons disease dementia, there is at least one yearand usually 10 to 15 yearsbetween the Parkinsons diagnosis and the onset of dementia. According to estimates by the Alzheimers Association, 50% or more of people with Parkinson’s disease eventually experience dementia, although there are a number of risk factors that impact the likelihood of developing symptoms:
- Parkinsons patients who experience hallucinations, excessive daytime sleepiness, and more severe motor control problems are at higher risk for dementia.
- Dementia is more common in people who are older at onset of Parkinsons.
- Dementia is a bigger risk factor in non-tremor predominant Parkinsons.
- Overwhelming stress, cardiovascular disease, and adverse reactions to the Parkinson’s disease drug levodopa can also indicate an increased risk for developing dementia.
- Dementia is relatively rare in people who develop Parkinsons before age 50, no matter how long they have had the disease.
Robin Was Very Aware That He Was Losing His Mind And There Was Nothing He Could Do About It
Schneider added: Robin was very aware that he was losing his mind and there was nothing he could do about it.
Jacqueline Cannon said of her fathers condition: He always used to say to me, Im losing my mind. We say to people that LBD is not just about memory. Its about the other symptoms that go with it, especially the hallucinations.
In the spotlight
Like Parkinsons disease there is currently no cure for LBD, and a need to raise awareness the case of Robin Williams will no doubt help. Dedicated research centres do already exist, such as the leading Biomedical Research Unit in Lewy Body Dementia at Newcastle University.
Professor Ian McKeith, president of the Lewy Body Society, believes there is cause for hope however. In a piece published by The Conversation, he wrote: Therapeutic trials have been few and far between in LBD because of a combination of a lack of compounds to test, a pre-occupation with targeting Alzheimers and a reluctance of regulatory bodies to recognise LBD. All of these are now changing and LBD is increasingly viewed as a malleable and commercially-viable target.
You May Like: Physiotherapy Management For Parkinsons Disease Ppt
Recommended Reading: Parkinson’s And Walking Problems
Advice For Carers Family And Friends
Living with or caring for someone with Parkinsons disease dementia can be challenging. Sometimes help and support will be relied on heavily but there will be times when it will be better to step back and allow the person with dementia to do things for themselves. This balance will be difficult to judge at first, but with time and patience new routines and approaches to day-to-day living can be established.
It is important to encourage, stimulate and help the person with dementia, but remember too that rest is important.
Tips For Care Partners
- Offer help only when asked.
- Prompt the person for example, instead of asking, Did anyone call? ask, Did Linda call?
- Say the name of the person and make eye contact when speaking to gain and hold attention.
- Put reminder notes and lists in a prominent place.
- Keep things in routine places.
- To ensure medications are taken on time, provide a dispenser, perhaps with a built-in alarm.
- Use photos on cell phone contact entries to prompt face-name association.
- If the person is searching for a word, provide a cue, such as, the word you are looking for probably begins with d.
- Do not finish the sentences of a person who needs more time to put them together.
- When presenting the person with a list of actions, first verbalize them, then write them down.
- Ask questions to moderate the conversation pace and allow catch up and reinforcement.
Page reviewed by Dr. Kathryn P Moore, Movement Disorders neurologist at Duke Health, a Parkinson’s Foundation Center of Excellence.
You May Like: Weed Killer That Causes Parkinson’s Disease
Do Parkinsons Patients Get Violent
Parkinsons disease Dementia or PD Dementia can make a patient very aggressive. Parkinsons Dementia Aggression germinating from Parkinsons disease Dementia can lead patients to behave erratically, experience sudden anger outbursts, feel constantly irritated, and always be in a state of restlessness.
Also Check: Parkinsons Leaning To One Side
Things You Should Know About The Link Between Parkinsons And Dementia
Both Parkinsons disease and dementia were ravaging the brain and behavior of actor Robin Williams before his death, but at the time, he didnt realize he had the latter.
Despite the fact that the signs of this combination can be confusing, the double diagnosis of Parkinsons and dementia impacts a large number of people. Of the one million people who have Parkinsons in the U.S., 50 to 80 percent may have dementiaeither as a result of Parkinsons pathology, or separately.
Robin Williams widow, Susan, wrote an editorial published in Neurology that was addressed to neurologists after his death. In it, she shared what it was like seeing her husband experience both Parkinsons disease and Lewy body dementia firsthand.
My hope is that it will help you understand your patients along with their spouses and caregivers a little more, Susan wrote.
Williams was first diagnosed with Parkinsons disease, which at first seemed to provide some answers for his out-of-character symptoms.
But it wasnt until after his death that an autopsy revealed he had been in the later stages of Lewy body dementiaa common form of dementia characterized by deposits of Lewy body proteins in the brain, which can impact physical movement, mood, memory and behavior.
I will never know the true depth of his suffering, nor just how hard he was fighting, Susan wrote. But from where I stood, I saw the bravest man in the world playing the hardest role of his life.
Don’t Miss: Tai Chi Exercises For Parkinson’s Disease