Rem Sleep Behavior Disorder
One very common sleep disturbance is REM Sleep Behavior Disorder, otherwise known as RBD. RBD is characterized by people acting out vivid dreams, including talking, jumping out of bed, kicking, biting, etc., even though the person is often unaware of it. About 50% of people with Parkinsons report RBD as one of their symptoms, but even more strikingly, 80% of people with RBD will develop a neurodegenerative disorder within 10 years, making it a highly effective predictor. Several studies of prodromal Parkinsons indicate that sleep issues, especially RBD, are strong measures of conversion to movement disorders. There are a variety of ways to deal with RBD, including taking medication. However, environmental treatments like adjusting your sleeping space, getting separate beds or introducing a sleep barrier can also be helpful for both for the person with RBD and the bed partner.
Sleep Disorders And Parkinsons Disease
Are You At Risk?
Better to not jump the gunpoor sleep habits, restlessness, sleep deprivation can occur due to several reasons. According to the CDC, most people experience difficulty sleeping at some point in their lives almost 30 percent of U.S. adults get 6 or less hours of sleep per night. Some feel refreshed after only 6 or 7 hours, however, most adults need about 8 hours of sleep every night to feel rested.
What are the reasons for sleep disorders? Many can have reasonable explanations ranging from age, stress, lifestyle choices, over stimulation prior to bedtime, medications, menopause, sleep apnea, restless leg syndrome and even depression.
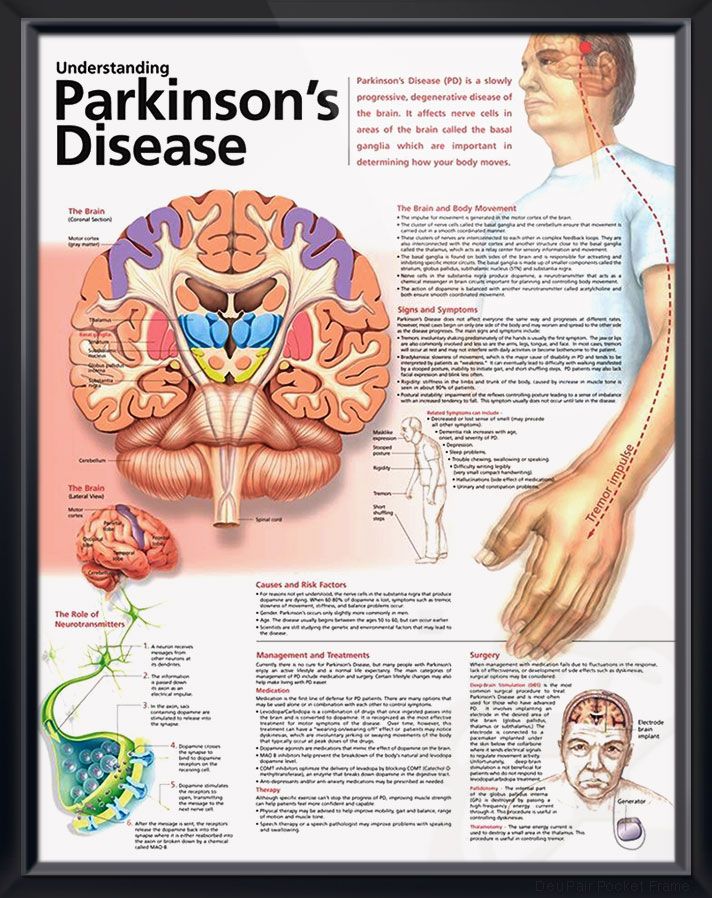
There are, however, certain signs that may indicate a more serious condition, such as the early stages of Parkinsons disease. Although there are other signs of PD, such as involuntary shaking of parts of the body, hand tremors, slow movements, stiffness and inflexible muscles, sleep disorders can also be an indicator that this disease is present.
So, why does this happen? According to a recent study, individuals who have disturbed sleephitting, punching, shouting, having nightmares, jerking and twitching, could indicate the early stages of Parkinsons disease. This is caused by inflammation in the brain there is a lack of dopamine in the brain and the brain stops producing the dopamine because the group of nerve cells that produce it ceases to work.
Why Do Parkinsons Patients Have Trouble Sleeping
Despite having daytime tremors, Parkinsons patients do not shake in their sleep. However, both Parkinsons disease itself and the medications used to treat it can give rise to a number of sleep problems that lead to insomnia and excessive daytime sleepiness.
Patients with motor symptoms may have trouble adjusting sleeping positions to get comfortable. Others may experience distressing nocturnal hallucinations when trying to fall asleep. These may be a result of medications or cognitive impairment.
In turn, excessive daytime sleepiness may occur as a consequence of sleeping poorly at night. It may also be triggered by medications. Parkinsons patients who suffer from EDS may be at a higher risk of accidents and unable to safely carry out activities such as operating a motor vehicle.
Since insomnia frequently goes hand-in-hand with anxiety and depression, it may be a contributing factor to sleep problems in people with Parkinsons disease. For that reason, doctors often look for mental health disorders in people with Parkinsons disease who have sleep problems.
Don’t Miss: Mri Findings In Parkinson’s Disease
Parkinsons Disease And Sleep
Reviewed by David Rye, MD, and Mark Mahowald, MD. Published by the National Sleep Foundation
This web article offers a detailed description of Parkinsons disease and the challenges it presents to restorative rest and recuperation. Some suggestions are included for improving sleep and the environment around sleeping.
Spend Time Outside During The Day
Take advantage of the sunlight when its out in the daytime. Consider spending time outdoors for exercise. Simple walking or running can contribute to your daily exercise quota, but avoid heavy exercises and activities after 8:00 PM.
Your goal for spending time outdoors is to get enough light. You could invest in a light therapy box for artificial light if you have trouble going outdoors. Such tools are available at drug stores.
Read Also: Parkinson’s And Immune System
What Does The Research Show
Dr. Daniel Kripke of the University of California, San Diego researched connections between sleeping pills and disease/mortality risk. He found that people who took sleeping pills were 4.6 times more likely to die than those not taking sleeping pills in a 2.5-year period. In the same time period, he found that people taking more than 132 pills per year were 5.3 times more likely to die, and people taking just 18 pills per year were still 3.6 times more likely to die. Further, sleeping pills cause higher rates of infection, increased risk of car accidents , high fall rates and higher heart disease and stroke rates. These statistics are not meant to tell you to stop taking your prescribed medication. Rather, they should encourage you to consider whether a pharmacological solution is best for you. If you are interested in alternative ways to improve your sleep, keep reading for tips on better sleep hygiene and speak to your health care professional to make the changes you see fit.
Parkinsons can manifest in many different non-motor symptoms, and sleep issues are very common. Poor sleep is a hallmark of Parkinsons and is a pre-motor symptom. Sleep disturbances are also the most commonly reported non-motor symptom. Quality of sleep is a keystone of Parkinsons, since if you dont sleep well enough, you cant manage your other symptoms effectively.
Circadian Rhythm Sleep Disorders
Circadian rhythm sleep disorders potentially influence daytime and nocturnal dysfunctions. It is common to find that PD patients go to bed and wake up very early therefore, a phase advance may occur . Advanced sleep phase is usually associated with older age and characterized by involuntary sleep and waking times that are generally more than 3 h earlier than usual sleep times. For patients with PD, both age-related changes and brain damage can provoke circadian rhythm sleep abnormalities. This relationship deserves more careful clarification, although it is complex. For instance, a slower absorption rate of levodopa during nighttime, possibly related to delayed gastric emptying, has been reported in PD patients . In agreement with this example, it has been documented that phase advance in PD is possibly influenced not only by age but also by dopaminergic therapy and disease severity . Given the complexity of this issue, an abnormal pattern of daily activities and associated comorbidities, such as depressive symptoms and daytime sleepiness, could also influence circadian rhythms . Thus, the analysis of this complex issue must take all of these variables into careful consideration.
Read Also: Are You Born With Parkinson’s
Develop A Bedtime Routine
Your bedtime routine should help you prepare for bed. So be sure to follow it every evening. Essential tasks that every bedtime routine must have include:
- Having a Light Snack: Eat only light snacks if you get hungry before bed. Heavy meals before going to bed are unhealthy and can result in weight gain. Also, avoid snacks that might contain stimulant ingredients like alcohol and caffeine.
- Taking a Warm Bath: Bathing in warm water before bed may improve sleep quality. However, be sure not to spend too much time in the bath as it may wake up your body.
- Go to the Toilet: Be sure to finish your business in the bathroom before bed. Minimize your liquid intake at least three hours before bedtime to help avoid nocturia.
- Brush Your Teeth: Brushing your teeth right before bed helps prevent dental problems, including cavities and decay. Although it is indirectly related to better sleep, having this step in a bedtime routine is helpful.
What Didnt Work For Me But Might Work For Others
My Parkinson’s Nurse first tried swapping out the sleeping drug that the doctor would no longer prescribe for pharmaceutical melatonin. This didn’t work for me and made my insomnia even worse. However, I was anxious about it, because there are contra-indications for long term use in PD. Some theories of PD even assert that it is not just a shortage of dopamine which is the issue, but the resulting imbalance between dopamine and melatonin .
Whenever we look at other hormones and neurotransmitters in people with PD , the balances with dopamine are always off. It appears that it is more the relative levels between various biochemicals which are causal, rather than the absolute levels of any one individual chemical. The old-fashioned “dopamine producing cell death” narrative was naïve.
Indeed, a light therapy protocol developed by a clinic in Australia for PD, which has demonstrated real life long term symptom reduction , works by attacking melatonin when it is at its peak value, thus bringing balance back to dopamine and melatonin levels.
Furthermore, Dr Andrew Huberman also expresses qualms about melatonin as a long term solution, as it reduces levels of sex hormones.
Indeed, I discovered something interesting along the way. Taking the passion flower tincture reduced my pain and rigidity! I later found out that passion flower is a weak MAO inhibitor, and hence slows the break down of dopamine, works like the PD drug Rasagiline.
You May Like: What Are Some Symptoms Of Parkinson’s Disease
Cause And Effect Of Parkinsons Disease And Sleep
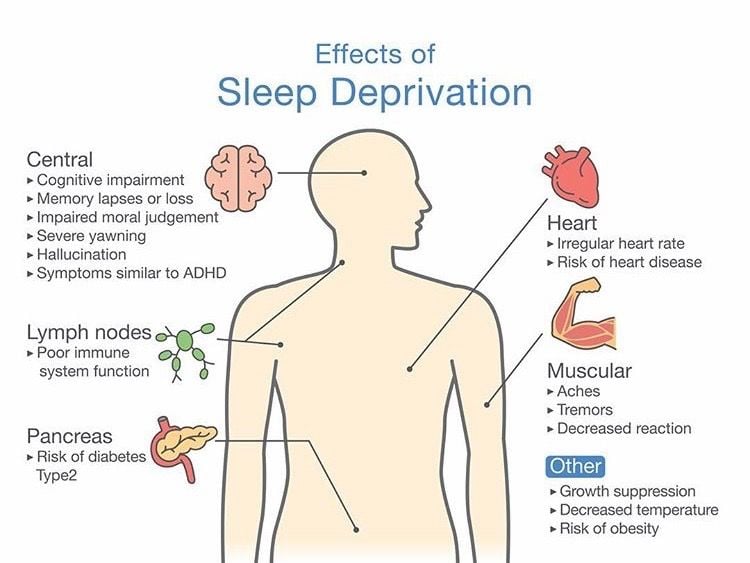
PD and poor sleep have a bidirectional relationship. However, It remains unclear whether PD symptoms cause poor sleep or the other way around. Sleep deprivation increases the chances of developing oxidative stress, which negatively affects the brain and is linked to PD.
Poor sleep quality may serve as an early sign of PD. Understanding how sleep disorders may cause a person to develop Parkinsonian symptoms can help experts diagnose the disease better. Usually, doctors diagnose PD when a patient displays motor symptoms. However, by then, they have already incurred brain cell damage.
As such, longitudinal research into the relationship between Parkinsons disease and sleep quality remains ongoing. Understanding the connection would help doctors screen patients, for risk of developing the disease, thus allowing them to delay the onset as much as possible.
Promotion Of Oxidative Stress
The accumulation of reactive oxygen species following cellular redox imbalance leads to mitochondrial dysfunction and oxidative stress in the brain. These processes are also thought to play important roles in the pathogenesis of PD, independent of the effects of aggregation and deposition of misfolded proteins in the CNS . Data collected from preclinical PD patients indicates that they exhibit an elevated level of cellular oxidative stress, which occurs prior to significant neuronal loss . Mounting evidence from both in vitro and in vivo studies indicates that redox imbalance is a contributor to the cascade underlying dopaminergic neurodegeneration moreover, strategies to restore redox homeostasis reverse this neurodegenerative process . Excessive accumulation of ROS is thought to adversely affect the chemical modification and oxidation of DNA, lipids, and proteins at the molecular level and contribute to apoptosis, cytoplasmic cell death, and autophagic cell death at the cellular level . Damage to mitochondria, especially inhibition of the electron transport chain leading to chronic production of ROS, has also been observed in the SN of PD patients . In addition, electron transport chain inefficiency caused by chronic administration of the complex I inhibitor rotenone was shown to be an important contributing factor to the aggregation of proteinaceous inclusions resembling Lewy bodies, as well as to degeneration of the SN in animal models .
You May Like: Tce Exposure And Parkinson’s
Sleep Benefit And Positive Effect Of Sleep Deprivation In Patients With Pd
The complex interaction of sleep and motor function is reflected in two interesting phenomena: sleep benefit, i.e. the experience of an improvement of motor function upon awakening , and a positive effect of sleep deprivation on motor function .
Sleep benefit was first described based on patients reports, and systematically evaluated in large cohorts of patients with PD with contrasting results. Some groups reported this phenomenon to be common in a subgroup of PD patients with specific clinical characteristics, e.g. with longer disease duration and younger age at onset of disease . This phenomenon has been reported to be so relevant to allow PD patients with sleep benefit to skip or delay medication . A study systematic evaluating motor state a night before sleep and in the morning upon awakening reported a slight motor improvement in the morning in patients with sleep benefit, without polysomnographic differences between the two groups . Another study using PSG reported shorter total sleep times and longer sleep latencies in PD patients reporting sleep benefit .
However, other groups found no actual improvement in motor functioning in PD patients reporting sleep benefit , or only in a small percentage of them , or reported in those patients with PD experiencing sleep benefit no association with the previously reported clinical variables , maybe because of methodological issues.
Sleep Problems And Parkinson’s Disease
Sleep problems are a common among those with Parkinsons Disease . If you have Parkinson’s and experience poor sleep, it’s important to talk to your healthcare provider, as treating your sleep-related symptoms may improve your overall well-being.
The first step in dealing with your sleep problem is determining the root cause. If you have early or mid-stage PD, chances are your sleep problems involve at least one of the following: insomnia, excessive daytime sleepiness, restless or shaky leg movements at night, intense dreams associated with REM behavior disorder, or poor sleep due to depression. While you will need professional medical assistance to determine what’s causing your sleep problems, the following will help you understand what may be going on.
Read Also: How To Test For Parkinson’s
What Did Work For Me
At the same time as implementing the solutions below, I was already undertaking daily Block Therapy, the Safe and Sound Protocol sessions, and many breathing exercises, which have all been helping to lower, and continue lower, my pain and discomfort, my anxiety and my drug burden. I’m sure this has all also allowed me to sleep better in large part too. Also, even now, getting good rest still requires very strict adherence to sleep hygiene. For me this requires strictly no food or drink apart from water after 6 pm, no looking at computers or phone screens after 7:30 pm, being in bed for sleep before 10pm. In fact, according to the work of Dr Panda mentioned above, the time restricted eating in particular may have had a more significant impact on my sleep than I had realized.
What I’ve found really helped me start to resolve my total insomnia was the “Sleep RX” program of the Brain Tap app., which I first heard about in an episode of the Better Health Guy podcast. The app contains listening programs which consist of special combinations of guided meditations, hypnotherapy, tonal therapy and music. I started by listening to one of the half hour sessions mid-morning each day, after the first dose of PD medication has worn off, while I am in the âoffâ state. I quickly notice that the choice of the female voice worked better for me. After about a week, I found I was at least getting a couple of hours sleep a night.
Rem Sleep Behavioral Disorder
Rapid eye movement, or REM, sleep is a normal part of the sleep cycle when people dream. Usually the only part of the body that moves during REM is the eyes, thus the name.
- People with rapid eye movement sleep behavior disorder do not have the normal relaxation of the muscles during their dreams. Therefore, they act out their dreams during REM sleep.
- People with RBD may shout, kick their bed partner or grind their teeth. Sometimes, in moderate to severe RBD, people may have aggressive, violent behaviors, like getting out of bed and attacking their bed partner.
- About half of people with PD suffer from RBD. It may develop after or along with the disease, but in most cases, it precedes the PD diagnosis by five to 10 years.
RBD Treatment
- Consider making environmental adjustments to protect the person with RBD and bed partner from injury. This may include padding the floor, using bed rails or sleeping in separate rooms.
- Clonazepam has been shown in large case series to improve RBD in 80 to 90 percent of cases. The dose of clonazepam required is low, usually from 0.5 mg to 1.0 mg. The adverse effects of clonazepam include nocturnal confusion, daytime sedation, and exacerbation of obstructive sleep apnea, if present. It is in generic form and not expensive.
- Talk to your doctor about the over-the-counter sleep aid Melatonin. Doses up to 12 mg at night one hour before can improve RBD.
Recommended Reading: Can Thyroid Problems Cause Parkinson’s
What Causes These Issues
Several studies have investigated the causes of these sleep disturbances and have found that a combination of motor symptoms, iatrogenic issues, dysfunction of the autonomic nervous system and neurodegeneration come together to disrupt normal sleep patterns. In addition, certain medications can cause vivid dreams and nightmares, which become worse in conjunction with RBD. Some of these issues can also be caused by pain, muscle cramping, nocturia or non-Parkinsons causes like exercising too late in the day, drinking caffeine and alcohol or too much light in the bedroom. These symptoms can be addressed through certain lifestyle changes or in some cases by medications. However, before trying any of these methods, its important to talk to your doctor.
Unfortunately, while sleep disturbances are common symptoms of Parkinsons and can have severe impacts on quality of life, insufficient studies exist about treatments. Though many medications are in existence, they are not applicable across the board and often can have unfortunate side effects. More research is necessary to find better solutions, and your participation in clinical trials can be instrumental in working to find these solutions.
Sleep hygiene is the set of habits and behaviors that help you sleep well on a regular basis. Below, we offer some general and Parkinsons-specific sleep hygiene tips to hopefully help improve your sleep.