Colm Was Diagnosed With Parkinson’s Around 3 Years Ago And Experiences 4 Different Types Of Pain Related To The Condition
The 4 different types of pain I experience all affect my muscles and joints. This includes sudden-onset joint pain typically a frozen shoulder, or pain when I bend an elbow or knee. It usually lasts between 6-8 weeks and will usually go away for a week or 2, only to reappear in another joint. It greatly restricts my movement and its constant nature can be frustrating.
I also have issues with leg cramps and dystonia, which I frequently experience when waking in the morning, or when moving between different ground surfaces. The cramps are very severe with sudden onset, but slowly wear off after some minutes.
My Parkinson’s has worsened certain pre-existing conditions, including back problems, which were caused by a childhood injury. This has caused me painful episodes throughout my life, but my Parkinson’s seems to have exacerbated this to the point where I’m totally incapacitated with pain and stiffness.
As a carer, I have no option but to try and carry on with my normal duties…I find it helps to wake about 2 hours earlier than normal to take my medication.
I keep an armchair and some dressing aids in my bedroom, as a bout of very severe back pain makes getting in and out of bed or dressing myself difficult.
I also experience muscle stiffness and inflexibility, which cause me pain due to over-exertion. This happens if I don’t take regular breaks throughout the day. As a carer myself for 3 disabled family members, this can prove very difficult.
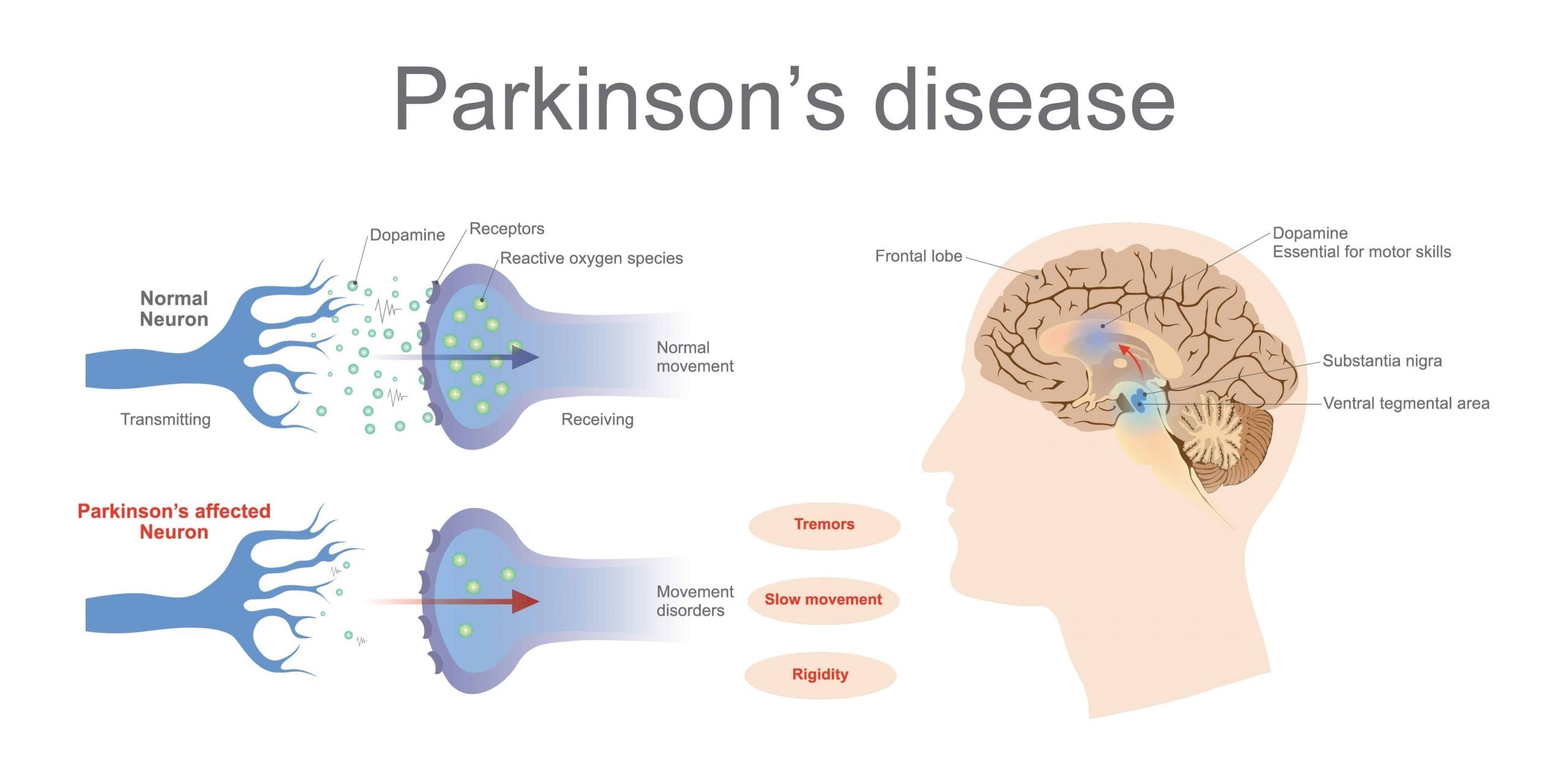
What Are The Symptoms Of Parkinsons Disease
Symptoms of Parkinsons disease and the rate of decline vary widely from person to person. The most common symptoms include:
Other symptoms include:
- Speech/vocal changes: Speech may be quick, become slurred or be soft in tone. You may hesitate before speaking. The pitch of your voice may become unchanged .
- Handwriting changes: You handwriting may become smaller and more difficult to read.
- Depression and anxiety.
- Sleeping disturbances including disrupted sleep, acting out your dreams, and restless leg syndrome.
- Pain, lack of interest , fatigue, change in weight, vision changes.
- Low blood pressure.
Fibromyalgia Vs Lupus Differences In Symptoms Pain Causes And Treatment
Fibromyalgia and lupus are two conditions that can cause pain, but its important to recognize the many significant differences between the two. Systemic lupus erythematosus , or lupus, is an autoimmune systemic disorder, which affects the joints, skin, and practically any organ in the body. Fibromyalgia affects the muscles causing pain, tender points, and extreme fatigue, and can contribute to anxiety or depression.
Both lupus and fibromyalgia are difficult to diagnose, and many patients with fibromyalgia are often wrongly diagnosed with lupus and vice versa. Furthermore, the two diseases can actually overlap one another, and there is a higher risk of rheumatic disease in fibromyalgia patients.
Fibromyalgia affects roughly two percent of the population and women are more likely to develop fibromyalgia than men. Estimates of lupus cases in the U.S. are 161,000 with definite lupus and 322,000 with definite or probable lupus. Like fibromyalgia, lupus often affects women more than men, too.
Also Check: Judy Woodruff Health Problems
Pain In Parkinsons Disease
Parkinsons patients suffer from the same pain other people have, often amplified by the motor dysfunction, but they also have additional pain problems unique to PD. Lower back pain and back of he neck pain are most common. Strengthening exercises or stretching may be helpful. Identifying the cause of the pain is essential in treating the pain. Treatments include physical therapy, medications, and alternative therapies like Reiki, acupuncture and massage.
Mechanisms That Contribute To Persistent Pain In Pd

As the field progresses psychophysical testing has the potential to advance our understanding of persistent pain in PD by elucidating the mechanisms which underlie pain in PD, and in doing so, identifying subgroups of patients with susceptibility to developing persistent pain while assisting in the development and monitoring of personalised pain management strategies for these patients.
Don’t Miss: Weighted Silverware
Is Accurately Targeted Treatment Possible
Single targeted surgery enables Parkinsons Syndrome Sufferers to be precisely treated with the minimum of damage to tissues, reduced patient risk and enhanced long-term outcome and more essentially without the use of General Anaesthesia. This treatment, which is called Foraminoplasty because it is carried out in the gaps or Foramen between the vertebrae, allows the nerve to thoroughly liberated and the overriding joints or pointed fracture margins to be removed. This is only possible by the use of Endoscopic Minimally Invasive Spine Surgery where the full length of the exiting nerve can be explored and the points of irritation clearly demonstrated. In the breadth of presentations arising from Degenerative Disc Disease and Failed Back Surgery or Failed Chronic Pain management, Endoscopic Lumbar Decompression & Foraminoplasty achieved a successful enduring positive outcome in 80% of cases.
Q Which Pharmacotherapies Are Best For Treating Pain In Pd
Dr. Fleisher: The first step is to make sure that Parkinsons medications are optimized. For example, dystonic or musculoskeletal pain may be caused by Parkinsons motor symptoms when dopamine levels are too low. If the patient is able to keep a pain diary, it may show a clear pattern of pain occurring the hour before each dose or before specific doses, suggesting the need to either increase the dosage preceding the pain episode, increase the frequency of medication dosing, or use adjunctive dopaminergic therapies to achieve more steady dopamine levels throughout the day.
In addition, optimal management of comorbidities that may contribute to pain is needed. The choice of pain medication depends on the pain type.
The first lines of treatment for musculoskeletal pain can be heat and cold packs and nonsteroidal anti-inflammatory drugs alone or in combination with acetaminophen.
For dystonic pain, adjustment of dopaminergic medications is particularly critical however, if dystonia consistently occurs in 1 particular body part, botulinum toxin injections also can be helpful. The goal of botulinum toxin injection is to weaken the muscle enough to stop the abnormal contractions and twisting, but the patient may lose function in the body part as a result . Thus, patient counseling is important to manage expectations.
Don’t Miss: Judy Woodruff Parkinson’s
Upper Cervical Specific Chiropractic And Fibromyalgia
For these reasons, it makes sense that upper cervical specific chiropractors have found success in helping fibromyalgia patients. In some case studies, patients have even become symptom-free. Whether you are dealing with chronic pain, fatigue, eye problems, migraines, headaches, sensory sensitivities, or any other fibromyalgia symptoms, this may be the natural solution youve been looking for.
If you are living with fibromyalgia, especially if you have a history of head or neck injuries that may have caused a misalignment, please contact an upper cervical practitioner in your area. Remember that the accident does not have to be recent because these small subluxations can work under the surface for years to cause symptoms. The search feature on this website can help you to locate one of our preferred doctors in your area. We hope this is the first step that puts you on the path to better overall health and well-being.
to schedule a consultation today.
Painful Symptoms Of Parkinsons Disease
Pain can sometimes be an early symptom of PD. For example, a person may complain of a painful shoulder and be diagnosed with an orthopedic condition such as a frozen shoulder, only to develop a rest tremor on that side at a later point. The painful shoulder was in fact not a frozen shoulder after all, but rather pain due to the rigidity of PD. Now of course, sometimes a frozen shoulder is really just a frozen shoulder, so theres no need to jump to conclusions when you are experiencing pain. Not every ache and pain is a sign of PD, but it is important for you to educate yourself, be aware of the possible connections, and be proactive about seeking medical attention for any notable pain you are experiencing.
If you have PD and develop pain, it is important to first bring this to the attention of your doctor. The pain may be related to your PD, or the pain may be due to a common problem such as arthritis which is exacerbated by your PD. However, in some cases, it may be a symptom of a more serious medical problem. So do not assume that the pain is related to your PD before getting an appropriate medical workup.
Recommended Reading: Fitflop Shoes For Parkinson’s
What Are The Different Stages Of Parkinsons Disease
Each person with Parkinsons disease experiences symptoms in in their own unique way. Not everyone experiences all symptoms of Parkinsons disease. You may not experience symptoms in the same order as others. Some people may have mild symptoms others may have intense symptoms. How quickly symptoms worsen also varies from individual to individual and is difficult to impossible to predict at the outset.
In general, the disease progresses from early stage to mid-stage to mid-late-stage to advanced stage. This is what typically occurs during each of these stages:
Early stage
Early symptoms of Parkinsons disease are usually mild and typically occur slowly and do not interfere with daily activities. Sometimes early symptoms are not easy to detect or you may think early symptoms are simply normal signs of aging. You may have fatigue or a general sense of uneasiness. You may feel a slight tremor or have difficulty standing.
Often, a family member or friend notices some of the subtle signs before you do. They may notice things like body stiffness or lack of normal movement slow or small handwriting, lack of expression in your face, or difficulty getting out of a chair.
Mid stage
Mid-late stage
Standing and walking are becoming more difficult and may require assistance with a walker. You may need full time help to continue to live at home.
Advanced stage
Fact: Although Fibromyalgia Is More Common Among Women It Affects Men And Children As Well
Twice as many women as men suffer from the condition. No one knows exactly why.
Women are more likely to develop chronic illnesses that overlap like migraines, irritable bowel syndrome and pain disorders, says Goldenberg. Researchers suspect that estrogen and other hormones may play a part, but so far no one has found clear biological reasons why women may be more susceptible. We do know that women are more likely to complain of conditions and to go to physicians earlier than men do, he says.
Among children, it turns out, what used to be thought of as growing pains may in fact be undiagnosed fibromyalgia.
Also Check: Does Vitamin B12 Help Parkinson’s
General Aspects Of Pain Treatment In Pd
Despite the high prevalence of pain in PD, literature data suggest that only up to a maximum of 50% of PD patients receive at least some type of pain therapy .
Still, the fundament of pain therapy should be an optimized dopaminergic treatment which can improve pain related to insufficient dopaminergic supply such as akinesia and/or rigidity , pain due to dopaminergic over-supply such as dyskinesia and/or dystonia , or central pain that is dopamine-sensitive . This concept was reported to be effective in about 30% of PD patients . A standardized levodopa test can be helpful to decide whether the pain is dopaminergic responsive or not, but any result of this short-term effect must always be interpreted with caution so that the long-term assessment of pain under dopaminergic therapy over several weeks remains essential .
A systematic review and meta-analysis including databases from January 2014 until February 2018 investigated the efficacy of a variety of novel, complimentary, and conventional treatments for pain in PD and found the greatest reduction in pain for safinamide, followed by cannabinoids and opioids, multidisciplinary team care, COMT-inhibitors, and electrical and Chinese therapies, while the weakest effects were obtained for dopaminergic agonists and miscellaneous therapies . Table 1 gives an overview of larger randomized controlled trials of antiparkinsonian drugs and opioids assessing the effect on pain in PD patients.
Table 1
Fig.1
Managing Pain In Parkinson’s
This article summarizes the incidence, types, and causes of reported pain in Parkinson’s Disease . A table of recommendations on how to involve patients with Parkinson’s in their own pain management is provided, along with approaches to pain assessment. Finally, there is a discussion of pain management principles in PD, including optimization of dopaminergic medications, use of analgesics, and innovative treatments for pain management .
Also Check: Does Sam Waterston Have Parkinsons
Interested In Parkinsons Disease Research Sign Up For Our Forums And Join The Conversation
A total of 97 Parkinsons patients at a mean age of 67.7 years, including 60 men, and 97 individuals used as controls at a mean age of 67.5 years, including six men, without the disorder or other neuromuscular diseases, filled out a questionnaire on the intensity of local lumbar back pain. The intensity of leg radicular pain caused by inflammation and/or injury to a spinal nerve root was quantified by the visual analogue scale a continuous scale used to measure pain intensity.
In addition, the participants permanent functional disability was assessed via the Oswestry Low Back Pain Disability Questionnaire a self-completed questionnaire that includes 10 different topics: intensity of pain, lifting, ability to care for oneself, ability to walk, ability to sit, sexual function, ability to stand, social life, sleep quality, and ability to travel.
Patients were further asked to describe the painful sensation they experience as pricking, tingling, burning, paresthesia often described as feelings of pins and needles, or numbness or other.
The team also assessed Parkinsons duration, medications being used, severity of motor symptoms as assessed by the Unified Parkinsons disease rating scale part III and the Hoehn and Yahr stage, which is a system used to assess symptom progression.
According to the ODI results, minimal disability was reported by 43.8% of Parkinsons patients, moderate disability by 27.5%, severe disability by 22.5%, and crippled by 6.3%.
How Is Pain Treated For People With Parkinsons
No matter the cause, pain is often complex. When a person with Parkinsons experiences intense pain, especially in combination with other symptoms of Parkinsons, managing it can be challenging. There are, however, several ways you can adjust your medication regimen, exercise schedule, and lifestyle to reduce your pain and improve your quality of life.
Medications
There are various kinds of medications used to treat pain, especially for people with Parkinsons. In a recent webinar, Dr. Janis Miyasaki described how physicians approach pharmacological treatment of pain for people with Parkinsons:
The principle is to start with what is called the pain ladder. You always start with the least intensive, least side effect-giving treatment.Janis Miyasaki, MD
Step one
The first step of the pain ladder is hot and cold treatments along with stretching and flexibility exercises. People who experience rigidity and stiffness can sometimes alleviate pain using heating pads to loosen their muscles, then improve mobility by stretching, then address any residual pain with ice packs.
Step two
Step three
Step four
Step five
Other medical interventions
Don’t Miss: Sam Waterston Tremor
Q Are There Any Alternative Therapies That Are Effective For Pain In Pd
Dr. Fleisher: Although alternative therapies may be helpful, there is little evidence-based research to support their use. Certainly massage therapy, anecdotally, seems to be helpful for managing pain. Small studies suggest that acupuncture might improve sleep in patients with PD, but data on the effects on pain in PD is lacking. Larger, more well-controlled and reproducible studies of these therapies are needed.
Patients frequently ask about the effects of medical marijuana in managing PD, including pain symptoms. Several studies have looked at efficacy of marijuana in PD and have found that it probably is ineffective for most PD symptoms.11 However, we just dont have enough evidence to know for sure. The most rigorous study of medical marijuana in PD showed a trend toward worsening tremor.11,12
For most people, stress and anxiety worsen tremor, and anything that relieves anxiety will improve tremor. Thus, modalities such as yoga, meditation, and mindfulness training will improve tremor. Similarly, medical marijuana may improve tremor in certain people by temporarily reducing anxiety and stress, but the evidence has not borne this out yet.
Incidence And Prevalence Of Pd General Pain And Pd
Estimates of PD prevalence and incidence have provided conflicting estimates. In Europe, the annual incidence estimates range from 5/100,000 to 346/100,000. Approximately 60,000 Americans are diagnosed with PD each year. The challenges involved with differential diagnoses and other forms of Parkinsonism, as well as the long time course from initial PD-like symptoms to a correct diagnosis, are likely responsible for the discrepancy in numbers.
The reported prevalence of pain in PD and PD-related pain also varies between studies. In 2008, Negre-Pages et al estimated the prevalence of chronic pain in PD to be > 60%. PD pain is often reported as heterogeneous in its clinical presentation, with a disabling effect on quality of life assessments. In 1998, the Swedish Parkinson Association reported on a survey of nonmotor symptoms comprising almost 1,000 PD respondents, revealing that pain was more common in females than males . However, general pain is also common in the population, with 18%19% in a general adult population according to the prevalence data.,
In early-stage PD, pain is rated as one of the most troublesome NMS, and it seems to affect the side of the body that was initially worst impacted by motor symptoms of the disease .
Recommended Reading: Parkinson’s Double Vision
Pain In Restless Legs Syndrome And Pd
PD patients who receive increasing dopaminergic doses over their disease course could show an increased prevalence of restless legs syndrome . First, for the treatment of painful RLS, the compensation of iron deficiency, defined as an iron storage value of less than 5075g/l, is recommended . Iron should be applied preferentially intravenously, because efficacy of oral application has not been adequately evaluated and iron given orally can deteriorate constipation and interacts gastrointestinally with levodopa and COMT inhibitors . Of note, drugs that potentially reinforce RLS such as mirtazapine, SSRI or neuroleptics, should be discontinued.
In general, painful RLS in PD should be treated according to the guidelines for idiopathic RLS recommending low-dose dopamine agonists before night-time as first choice treatment, gabapentine and pregabaline as second line options, and oycodone/naloxone as escalation therapy . In PD, the non-ergoline derivates pramipexole, ropinirole and rotigotine should be preferentially used. Because rotigotine has shown positive effects on PD-associated pain beyond the RLS, it might be preferentially used in painful RLS in PD patients .
Carbamazepine and valproic acid were considered likely efficacious in idiopathic RLS but are not suggested in PD due to potential side effects.