Can Parkinson’s Disease Disrupt Sleep
An expert looks at whether there is an association between Parkinson’s and sleep apnea, and gives tips to get better sleep.
Lisa Shulman, MD, FAAN, responds:
Studies do not show that sleep apnea is any more common in people with Parkinson’s disease than in those without it. However, other sleep disturbances are associated with the condition.
Symptoms Can Disrupt Sleep
Many people with Parkinson’s disease wake up at night and have trouble getting back to sleep. Symptoms such as rigidity and slowness, for example, make it difficult to change position in bed. Tremors, which disappear during sleep, often recur when people wake up and may keep them from falling back to sleep. The need to urinate frequently, another symptom of Parkinson’s disease, also disrupts sleep. And a sleep disturbance called rapid eye movement sleep behavior disorder, in which people act out vivid dreams or nightmares by thrashing around or calling out while asleep, is associated with, and is sometimes a precursor to, Parkinson’s disease. The disorder contributes to poor quality of sleep. On top of that, aging itself can contribute to less sound sleep.
Naps and Medications May Interfere
Fatigue is a common symptom of the disease and a common side effect of some medications, which may cause people to nap more during the day. But daytime napping can also make it harder to sleep at night, creating a recurring cycle of fatigue. To counter this, try to balance rest periods with regular daytime activity.
How Can Caregivers Support Their Loved Ones
Caring for someone who sees, hears, or believes things that arent real can be very difficult. Try to be as patient and calm as you can.
Avoid arguing with the person. If they still have insight, gently explain that what theyre seeing isnt real. Tell anyone who cares for or visits your loved one what to expect, and how to respond.
Stay in close contact with the persons doctor. If their symptoms dont improve, ask whether they need a medication adjustment.
Check whether the person needs hearing aids or glasses. Poor hearing or vision can sometimes lead to hallucinations. It can also help to turn on bright lights at night, to prevent the shadows that may trigger visual illusions.
Secure any dangerous objects, and keep pathways in the home clear to prevent falls and injuries. If you ever feel like the person is a risk to themselves or others, call their doctor.
Risk Factors For Psychosis
Not everyone with Parkinsons will develop hallucinations or delusions, but there are several things can increase your risk:
- Dementia or impaired memory
- Depression: Individuals suffering from depression and PD are at a greater risk. In addition, severe depression alone can cause psychosis.
- Sleep disorders, such as vivid dreaming. Individuals commonly report vivid dreaming prior to the onset of psychosis. Other associated sleep disturbances include REM sleep disorder and general insomnia.
- Impaired vision
1Department of Neurology, Northwestern University Feinberg School of Medicine, Chicago, Illinois, USA.
2German Center for Neurodegenerative Diseases , Munich, Germany.
3Metabolic Biochemistry, Biomedical Center , Faculty of Medicine, Ludwig Maximilians University, Munich, Germany.
4Munich Cluster for Systems Neurology , Munich, Germany.
5Department of Chemistry, Chemistry of Life Processes Institute, Center for Molecular Innovation and Drug Discovery, and Center for Developmental Therapeutics, Northwestern University, Evanston, Illinois, USA.
6Parkinsons Disease Center, Department of Neurodegenerative Science, Van Andel Institute, Grand Rapids, Michigan, USA.
Address correspondence to: Dimitri Krainc, Northwestern University Feinberg School of Medicine, 303 East Chicago Avenue, Ward 12-140, Chicago, Illinois 60611, USA. Phone: 312.503.3936 Email: .
LFB and JZ contributed equally to this work.
Find articles byBurbulla, L.in: |PubMed |
Read Also: Diseases Similar To Parkinsons
Are There Alternative Therapies For Essential Tremor
Currently, there is no evidence that alternative treatments are beneficial in treating Essential Tremor. Patients who have tremors that worsen with emotional stress may find relaxation therapies helpful at temporarily easing symptoms.
Some herbal supplements may make tremor worse. Always consult your doctor before trying any alternative therapy.
Show Sources
Reviewanxiety: An Ignored Aspect Of Parkinsons Disease Lacking Attention
Anxiety is a neuropsychiatric complication of Parkinsons disease .
-
Anxiety has been given less attention while treating PD.
-
Management of anxiety is crucial to improve quality of life of the affected patients.
-
Use of complementary based medicines could be beneficial.
-
Alternative approaches will lead to novel therapeutic treatment for PD and various complications associated with it.
You May Like: Does Vitamin B12 Help Parkinson’s
Overview Of Pdp Management
Physical Versus Emotional Control:The intertwining pathophysiology of psychosis and PD through dopaminergic pathways presents healthcare professionals and patients with the unfortunate choice between physical and emotional stability. Dopaminergic agents that treat the symptoms of PD and maintain physical control are predominately associated with the triggering of psychosis symptoms through D2-receptor activation.9,11 This swing to emotional instability could be broadly treated in one of two ways. One option is to stop the anti-PD agent however, this is not feasible for most patients because physical instability and motor symptoms would return. Alternatively, an antipsychotic could be added, but nearly all typical and atypical antipsychotics work via D2-receptor antagonism, potentially tipping the scale toward physical instability. Accordingly, methods used in practice involve dose reduction of offending agents, as tolerated, or the use of an atypical antipsychotic with low D2-receptor affinity.9,11
Managing Anxiety And Depression In Parkinsons Disease
A combination of medication and other therapies can help ease non-motor symptoms affecting those with Parkinsons disease.
Most people think of Parkinsons disease as marked only by tremors, muscular rigidity and slow, imprecise movements, but Parkinsons is more than a movement disorder.
Most people with Parkinsons also have quite a few non-motor symptoms, such as anxiety, depression and psychosis. Many of these symptoms may have started before the Parkinsons disease became obvious.
The effects are widespread. Several years ago, a large clinical study of more than 1,000 people with Parkinsons disease of various durations demonstrated that only 1.4 percent of the participants did not report any non-motor symptoms.In other words, 98.6 percent of the study participants had some form of NMS. Psychiatric symptoms accounted for 60 percent, while visual hallucinations that could have signified psychosis were present in about 35 percent of patients.
Thats why taking action is important. If you or a loved one has had a new diagnosis of Parkinsons disease, we recommend an immediate evaluation for depression, mood and cognitive problems. Frequent monitoring should also be done throughout the course of the disease.
Here are some of the common symptoms and treatment methods for Parkinsons patients with depression and dementia:
You May Like: Voice Amplifiers For Parkinson’s
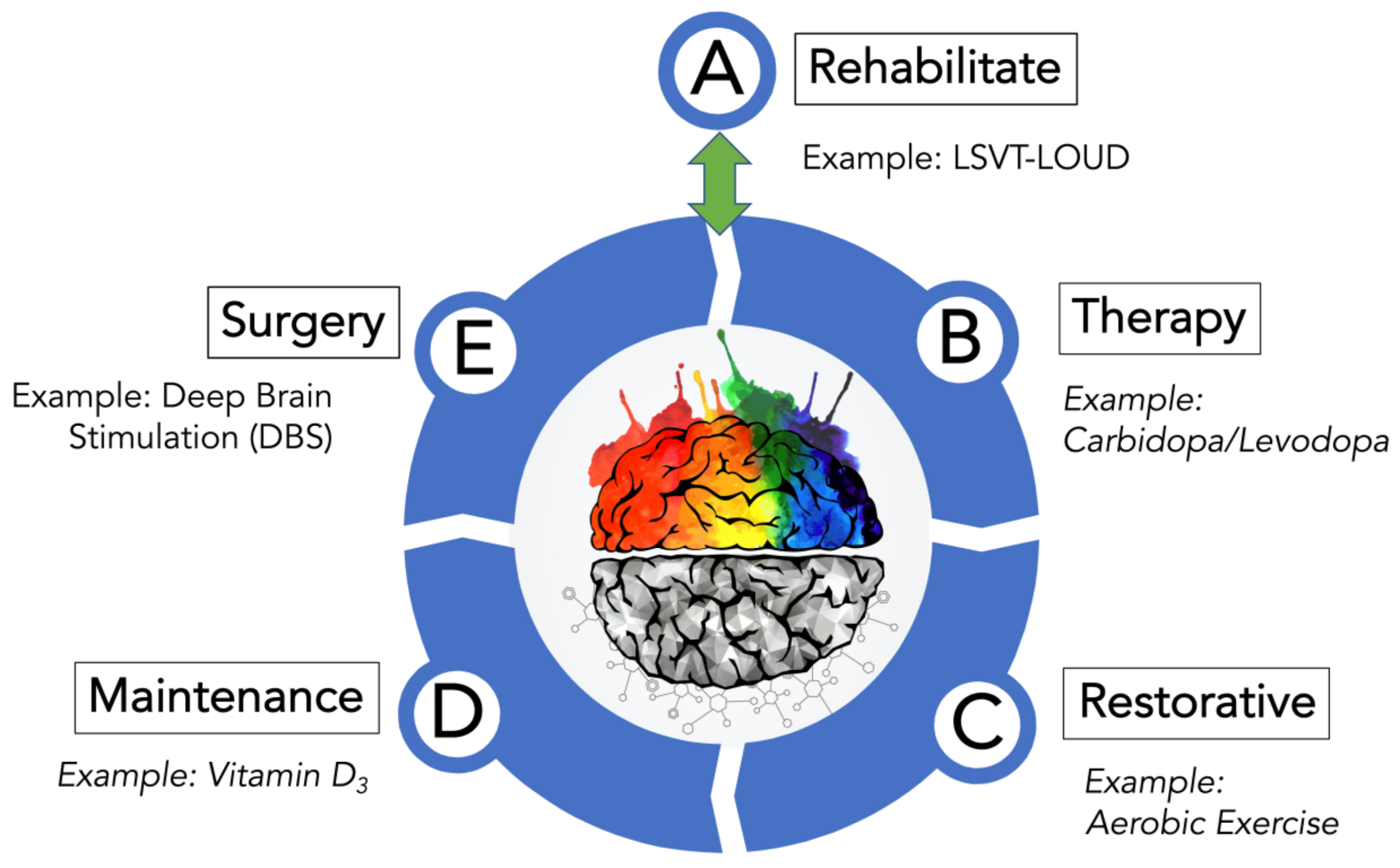
Pharmacological Management Of Motor Symptoms
The Parkinsons UK audit identified medicines management as a main area for improvement in PD services, as a third of patients feel that they are not given enough information when starting a new medicine . People with PD have a higher rate of emergency hospital admission than the general population and are also twice as likely to stay in hospital studies suggest that medicines management plays a part in extended lengths of stay.
The inpatient management of PD was previously covered in the learning article Considerations for the inpatient management of Parkinsons disease.
There is no cure for PD and no drug treatments have been proven to impact disease progression. Management is therefore symptomatic. Treatments to manage motor symptoms work by increasing dopaminergic activity. This is broadly achieved by three mechanisms:
Anticholinergics, such as benztropine and trihexyphenidyl, are not routinely prescribed in idiopathic PD but may be introduced for the management of tremor when dopaminergic medications are not effective. However, they should be avoided in the elderly population as they can cause hallucinations and confusion.
Levodopa therapy
Catechol-O-methyl transferase inhibitors
Glutamate antagonists
Dopamine agonists
Monoamine oxidase B inhibitors
Types Of Anxiety Disorders Found In Parkinson’s Disease
Generalised anxiety disorder, panic disorder, social phobia, phobic disorder, agoraphobia, obsessive-compulsive disorder, and anxiety disorder not otherwise specified have all been identified in patients with Parkinson’s disease . The diagnoses in the patients with Parkinson’s disease appear to be clustered in the panic disorder, phobic disorder, and generalised anxiety disorder areas.
Box 1: Anxiety disorders found in Parkinson’s disease
-
Generalised anxiety disorder
Recommended Reading: Yopd Life Expectancy
Us Food And Drug Administrationapproved Agents For Pdp: Pimavanserin
Pimavanserin is a 5-HT2A inverse agonist indicated for the treatment of hallucinations and delusions associated with PDP.25 Pimavanserin binds preferentially to the 5-HT2A receptor and, to a lesser extent, to the 5-HT2C receptors, and has low binding affinity to alpha, dopamine D2, histamine, muscarinic, and other serotonin receptors.26 The pharmacologic rationale for the efficacy of pimavanserin in PDP is based on investigations demonstrating that overstimulation of postsynaptic 5-HT neurons contributes to psychotic symptoms in PD. Serotonin 5-HT2A receptors exhibit baseline activity.27,28 In other words, 5-HT2A receptors spontaneously signal to produce and regulate cellular postsynaptic activity. Pimavanserin binds to 5-HT2A receptors and blocks the receptor and reduces the spontaneous baseline activity.28 This property of binding to the receptor and reducing spontaneous baseline activity is referred to as inverse agonism.
The US Food and Drug Administrationapproved labels for pimavanserin and all antipsychotics contain a boxed warning stating elderly patients with dementia-related psychosis treated with antipsychotic drugs are at an increased risk of death.31 However, it is important to note that if the psychotic symptoms are related to the underlying PD, pimavanserin can be used in patients with concurrent dementia.
Identifying Psychosis Diagnosis And Antipsychotics
The purpose of this study was to identify the incidence of new cases of antipsychotic use to treat psychosis in the first year after PD diagnosis. To be considered an antipsychotic user, first, a patient was required to have a new Read Code of psychosis diagnosis that appeared in the data after the diagnosis of PD diagnosis. Additionally, the Read Code for antipsychotics must have appeared after the diagnosis of psychosis and within the first year after PD diagnosis. Appendix 2 lists drugs considered antipsychotics and their drug classes .
Also Check: Adaptive Silverware For Parkinson’s
Side Effects Of Mysoline
Mysoline may cause unwanted side effects in the short term however, these side effects diminish with longer use. Side effects of Mysoline may include:
- Difficulty walking
- Fatigue
Serious complications with the drug are rare but could include blood cell and bone marrow problems. Your health care provider will check your blood counts every six to 12 months to screen for these problems. Mysoline has a drug interaction with phenobarbital, so the drugs should not be taken together.
Before taking Mysoline, be sure to tell your doctor if you:
In addition, you should avoid alcoholic beverages while taking Mysoline. Do not stop taking the drug suddenly or switch brands without first consulting with your health care provider.
Diagnosis Of Dip And The Role Of Dat Imaging
The clinical diagnostic criteria for DIP are defined as 1) the presence of parkinsonism, 2) no history of parkinsonism before the use of the offending drug, and 3) onset of parkinsonian symptoms during use of the offending drug. Since asymmetrical rest tremors are common in many DIP patients and symptoms persist or progress after cessation of the offending drug, patients clinically diagnosed with DIP may include individuals in the preclinical stage of PD whose symptoms were unmasked by the drug.,,,
DATs are presynaptic proteins in the membrane on terminals of dopaminergic neurons. They take up dopamine from the synaptic cleft projections that extend from the substantia nigra to the striatum. These transporters control dopaminergic transmission by spatial and temporal buffering, rendering the molecule an imaging target in diseases affecting the dopaminergic nigrostriatal pathway. Single-photon-emission computed tomography and positron-emission tomography scans are available using several DAT ligands., SPECT radioligands include 123I-N-3-fluoropropyl-2-carbomethoxy-3-nortropane , 123I-ioflupane, DaTSCAN, and 123I-2-carbomethoxy-3-tropane . PET scans may be superior to SPECT for imaging DATs, in that the lower energy of positrons provides higher resolution, resulting in better image quality with widespread clinical applications. However, most DAT imaging studies, including those in patients with DIP, have utilized SPECT.,-
Also Check: On Off Phenomenon
Therapies For Urinary Symptoms
Parkinsons patients often have to urinate more urgently and more frequently, a situation that can lead to incontinence. Drugs that relax the muscles of the bladder can relieve the symptoms. They include Ditropan , Detrol , Flomax , and Myrbetriq .
Parkinsons News Today is strictly a news and information website about the disease. It does not provide medical advice, diagnosis or treatment. This content is not intended to be a substitute for professional medical advice, diagnosis, or treatment. Always seek the advice of your physician or another qualified health provider with any questions you may have regarding a medical condition. Never disregard professional medical advice or delay in seeking it because of something you have read on this website.
Other Reasons To Avoid Benzodiazepines
Even if thats so, there are other reasons for older people to avoid benzodiazepines. In 2012, the American Geriatrics Society added benzodiazepines to their list of inappropriate medications for treating insomnia, agitation, or delirium. That decision was made primarily because common side-effects of benzodiazepinesconfusion and clouded thinkingoften have disastrous consequences, including falls, fractures, and auto accidents.
Even short-acting benzodiazepines pack a bigger punch in older people. As the bodys metabolism slows with age, drugs take longer to clear. And because benzodiazepines are stored in body fat, they can continue to produce effects days after people stop taking them.
Although these medications are taken to help people get a good nights rest, they can have the opposite effect. When theyre taken over time, they can actually interfere with normal sleep, says Dr. Fabiny. The quest to sleep through the night can lead to prescriptions for higher doses or longer-lasting benzodiazepinesand even greater side effects.
If you are a caregiver for an older person, you may want to check the medicine cabinet. If you find benzodiazepine, you might want to discuss it with him or her, or with a doctor.
If you take a benzodiazepine, keep in mind that these drugs are designed for short-term use. If youve been using them regularly for more than a few weeks, know that withdrawal symptoms can be powerful. Consider talking to your doctor about alternatives.
You May Like: Cleveland Clinic Parkinson’s Bicycle Study 2017
Pimavanserin Versus Quetiapine For The Treatment Of Psychosis In Parkinsons Disease And Dementia With Lewy Bodies
Compared pimavanserin to quetiapine in the treatment of Lewy body-related psychosis.
-
Used time to discontinuation analysis as a real-world, pragmatic, primary outcome.
-
Found lower early and higher late discontinuation of pimavanserin compared to quetiapine.
-
Pimavanserin may be more clinically useful at promptly managing psychosis.
-
Patients may continue quetiapine long-term for secondary, delayed benefits.
You May Like: What Are The Complications Of Parkinsons Disease
Whats Hot In Pd: As A New Drug Gains Fda Approval For Parkinsons Disease Psychosis Should We Fear Using It
This week the FDA approved the drug Pimavanserin for the treatment of Parkinsons disease psychosis. There has been a critical, unmet need for development of better drugs to address hallucinations and psychosis in the setting of Parkinsons disease. We have learned over many years that typical high potency neuroleptic antipsychotic drugs may improve hallucinations but do so at the cost of worsening Parkinsons disease motor symptoms and are associated with an increased mortality. We have changed our treatment strategy to address hallucinations in Parkinsons disease by using agents that will not worsen the common motor symptoms . We routinely choose quetiapine or clozapine instead of the classical dopamine blocking drugs. There are, however, shortcomings with these two drugs. Quetiapine has not been shown effective across several randomized Parkinsons disease clinical trials, but many Parkinson experts believe it is moderately helpful, particularly in the setting of mild hallucinations. Clozapine has been shown to be highly efficacious, but it requires weekly blood monitoring to check for a potentially life-threatening side effect called agranulocytosis where the drug attacks the bone marrow. The inconvenience and discomfort of blood draws have limited the penetration of this therapy.
Selected References:
Okun, MS. 10 Breakthrough Therapies in Parkinsons Disease. Books4Patients. 2015 .
Okun, MS. Should We Fear Antipsychotics in Parkinsons Disease Patients? 2015.
Read Also: Similar To Parkinsons
What Treatments Are Available For Parkinsons Psychosis
Your doctor may first reduce or change the PD medication youre taking to see whether that reduces psychosis symptoms. This is about finding a balance.
People with PD may need higher doses of dopamine medication to help manage motor symptoms. But dopamine activity shouldnt be increased so much that it results in hallucinations and delusions. Your doctor will work with you to find that balance.
Parkinsons Treatment For Non
A hallmark of Parkinsons is movement problems, but the disease has many non-movement symptoms as well.
A lot of the medications that address the non-movement problems are not specific for Parkinsons. Because a wide array of such medications is available, Parkinsons patients need to discuss with their doctor what treatments are best for them. One reason these discussions are necessary is that some treatments for non-movement problems can interact with Parkinsons medications.
Read Also: On-off Phenomenon
Lack Of Treatment Alternatives
The researchers examined Department of Veterans Affairs patient records from fiscal year 2008, comparing the rates of antipsychotic drug prescriptions among two groups: 2,597 patients with Parkinsons disease and psychosis with and without dementia and 6,907 patients with dementia and psychosis but without Parkinsons disease 97.3% of the patients studied were men.
More men are diagnosed with Parkinsons, and men are more likely to develop dementia, says Weintraub.
An estimated 60% of Parkinsons patients will experience some form of psychosis during their illness, according to the study. Weintraub and colleagues found that half of all patients with Parkinsons and psychosis were treated with antipsychotic medications.
Perhaps their most striking finding was that overall prescription rates had not decreased compared to 2002, despite the black box warning that was issued in 2005. To Fernandez, the reason is simple: doctors have few options to offer.
This study is very important because it highlights the problem that clinicians face, says Fernandez. The problem is its not very easy to treat, and few patients will be completely treated.
Weintraub agrees that treatment choices are quite limited, but he hopes that his study will encourage doctors to make greater use of clozapine and to be more conservative in prescribing other antipsychotics.