How Is Wpw Syndrome Treated
If youre diagnosed with WPW syndrome, you have several treatment options, depending on your symptoms. If youre diagnosed with WPW syndrome but dont have any symptoms, your doctor may recommend that you wait and continue follow-up appointments. If youre having symptoms, the treatment may include the following:
What Are The Symptoms Of Wpw
People may first experience symptoms at any age, from infancy through adult years.
Symptoms of WPW may include one or more of the following:
- Heart palpitations a sudden pounding, fluttering or
- Racing feeling in your chest
- Dizziness feeling lightheaded or faint
- Shortness of breath
- Rarely, cardiac arrest
Some people have WPW without any symptoms at all.
Recognition And Localization Of Accessory Pathways
When retrograde atrial activation during tachycardia occurs over an AP that connects the left atrium to the left ventricle, the earliest retrograde activity is recorded from a left atrial electrode . This is a left lateral pathway.
When retrograde atrial activation during tachycardia occurs over an AP that connects the right ventricle to the right atrium, the earliest retrograde atrial activity is generally recorded from a lateral right atrial electrode. This is a right ventricular free wall pathway.
Participation of a septal accessory pathway creates earliest retrograde atrial activation in the low-right atrium situated near the septum, anteriorly or posteriorly .
Retrograde atrial activation over the AP can be confirmed by inducing premature ventricular complexes during tachycardia to determine whether retrograde atrial excitation can occur from the ventricle at a time when the His bundle is refractory . Failure to advance the atrium when the His is refractory does not exclude an AP, particularly if far from the pacing site .
With entrainment pacing from the right ventricular apex, orthodromic reentrant tachycardia will return with a V-A-V response, typically with a short postpacing interval tachycardia cycle length difference if septal in origin. VA intervals remain fixed during SVT, and AV block cannot occur if the AV AP is critical to the circuit.
Don’t Miss: Adaptive Silverware For Parkinson’s
Deterrence And Patient Education
The dysrhythmias causing electrical abnormalities associated with WPW syndrome are a result of a congenital abnormality forming an accessory pathway. There is nothing that can be done to prevent WPW pattern. After WPW syndrome has manifested with the presentation of a tachyarrhythmia, an electrophysiologic study can be performed to map and assess risks of the accessory pathway, and catheter radiofrequency ablation of the pathway can be curative. For patients that this is not an option or preference, antiarrhythmic medications can be a reasonable alternative option.
Localization Of Accessory Pathways
The location of the AP can often be determined through analysis of the spatial direction of the delta wave in the 12-lead ECG by reviewing the maximally preexcited QRS complexes. A general rule is that Q waves point away from the earliest site of ventricular activation, which is typically the insertion point of the bypass tract. The most common locations for APs, in decreasing order of frequency, are the left free wall, the posteroseptal and right free wall, and finally the midseptal and anteroseptal regions of the heart.
Several algorithms are available to predict the location of the AP. These algorithms may not be totally accurate because maximal preexcitation is needed, and usually the QRS in WPW pattern is a fusion between AV node and AP depolarization , precordial lead placement may vary, as well as chest shape and size and heart shape, size, and location.
A practical concept is that a negative delta wave usually signals the location of the AP, as follows:
- A negative delta wave in a left-side lead such as I and aVL indicates a left-side AP
- A negative delta in a right-side lead such as V1 predicts a right-side AP
- An isoelectric delta in V1 predicts an anteroseptal AP
- A negative delta in the inferior leads indicates a posteroseptal AP
- A positive delta in the inferior leads predicts an anteroseptal AP
A more specific algorithm for location of the AP, based on the polarity of the delta wave or first 40 ms of the QRS, predicts the following AP locations:
Read Also: Parkinson’s Double Vision
What Are Wpw And Avrt
Preexcitation describes the situation in which impulses from the SA node or atrium reach the ventricle through an accessory pathway in addition to the AV node. WPW is a type of preexcitation syndrome in which there are ECG findings of an atrial-ventricular bypass tract and the patient demonstrates related tachydysrhythmias. The most common tachydysrhythmia seen in WPW is atrioventricular re-entrant tachycardia this is seen in 80% of patients with WPW and is what paramedics would most commonly be called for.
Recall that there are three mechanisms for the development of cardiac dysrhythmias:
Pearls And Other Issues
Patients with atrial fibrillation and rapid ventricular response are often treated with amiodarone or procainamide. Procainamide and cardioversion are accepted treatments for conversion of tachycardia associated with Wolff Parkinson White syndrome . In acute AF associated with WPW syndrome, the use of IV amiodarone may potentially lead to ventricular fibrillation in some reports and thus should be avoided.
AV node blockers should be avoided in atrial fibrillation and atrial flutter with Wolff Parkinson White syndrome . In particular, avoid adenosine, diltiazem, verapamil, and other calcium channel blockers and beta-blockers. They can exacerbate the syndrome by blocking the heart’s normal electrical pathway and facilitating antegrade conduction via the accessory pathway.
An acutely presenting wide complex tachycardia should be assumed to be ventricular tachycardia if doubt remains about the etiology.
Read Also: Does Vitamin B12 Help Parkinson’s
Characteristic Features Of Wpw Syndrome
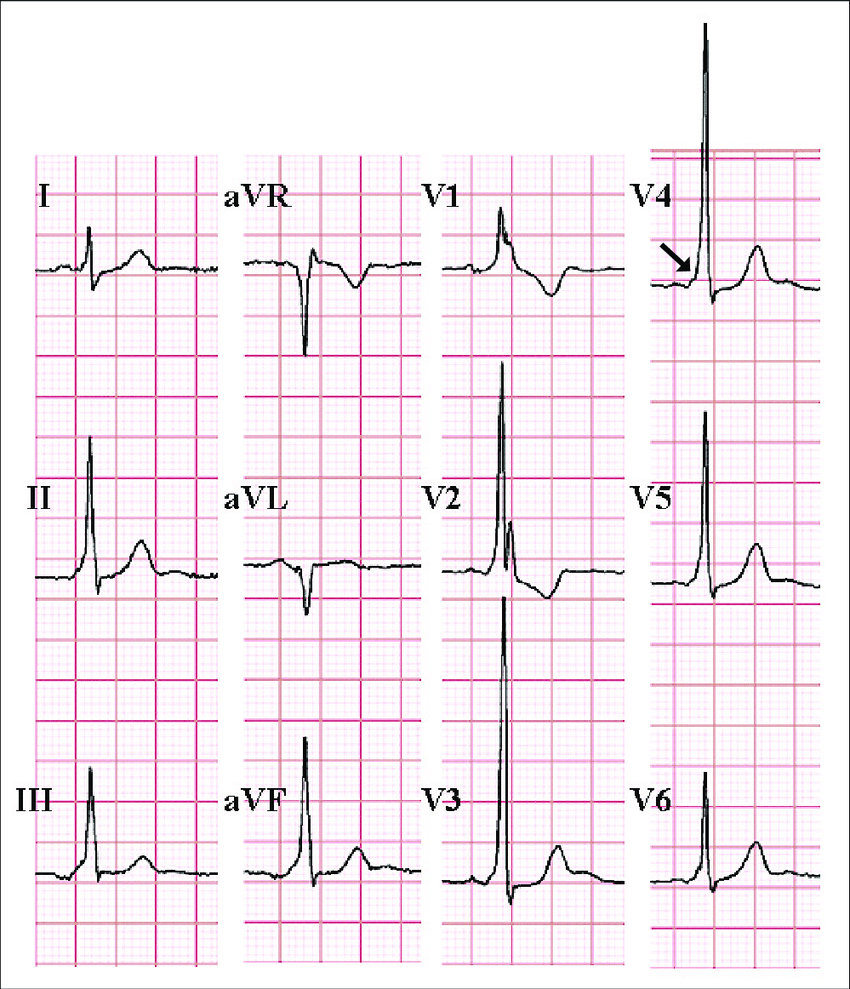
The classic ECG morphology of WPW syndrome is described as a shortened PR interval and a slurring and slow rise of the initial upstroke of the QRS complex , a widened QRS complex with a total duration greater than 0.12 seconds, and secondary repolarization changes reflected as ST segmentT wave changes that are generally directed opposite the major delta wave and QRS complex. In reality, the ECG morphology varies widely.
Depending on the location of the AP in relation to the sinus node and the relative transmission characteristics of the AP and the AV node, the morphology of the ECG may vary from a classic presentation, termed manifest preexcitation, to near normal.
In some cases, the electrical impulses arrival at the ventricles occurs slightly earlier through the AP , creating preexcitation.
The QRS interval is widened because the ventricles are initially activated via the AP, which lies outside the normal conducting system, producing an early, albeit relatively slow, initial propagation of depolarization forces through the ventricular tissue. This produces the delta wave. The delta wave makes the QRS appear wider than expected and the PR interval somewhat shortened. This is known as a manifest AP because it is easily identifiable on ECG.
An AP that does not manifest on ECG is revealed when the rate exceeds the refractory period of the AV node. This has been described as a latent AP. A latent AP can conduct both antegrade and retrograde transmissions.
Orthodromic Tachycardia With Concealed Accessory Pathway
Some APs are unable to conduct in an antegrade fashion. These are called concealed APs, because “manifest” preexcitation is a delta wave that is visible on a surface 12-lead ECG. They account for about 30% of all SVTs induced on EPS.
Although no evidence of the pathway is present during sinus rhythm , orthodromic tachycardias can occur. Orthodromic tachycardia may also occur when there are two or more accessory connections, and in that case, the retrograde conduction may occur through the AV node, through one of the accessory connections, or through both.
This type of SVT may be difficult to distinguish from the usual AV nodal reentrant tachycardia on a standard surface ECG. In adults, if the heart rate is higher than 200 bpm or a retrograde P wave is visible in the ST segment , a concealed AP-mediated orthodromic reentrant tachycardia may be the diagnosis. However, this determination is most accurately made with electrophysiologic studies , or if SVT terminates with a single PVC. Other differentiating factors include the following :
Also Check: On-off Phenomenon
Mill Hill Ave Command: Can You Give Adenosine To A
· 2) Second, there was a concern in the past that a certain percentage of wide-complex tachycardia were actually WPW with antidromic conduction, and so the advice was to avoid adenosine. The rationale was that since the bypass tract was capable of retrograde conduction, shutting down the AV node could expose the ventricles to potentially unregulated pacing.
Serotonin Syndrome : Symptoms Causes &
Serotonin syndrome, also known as serotonin toxicity, is a potentially life-threatening condition resulting from having too much serotonin in your body. Learn about serotonin syndrome symptoms, the medications that can cause the condition, and how it can beWebMDWebMD Better information. Better health.Treatment of atrial flutter · After atrial fibrillation, atrial flutter is the most important and most common atrial tachyarrhythmia. Although it was first described 80 years ago, techniques for its diagnosis and management have changed little for decades. The diagnosis rested almost entirely with the 12 lead ECG, and treatment options included only the use of a digitalis compound to slow and control the ventricular
Recommended Reading: What Is The Best Mucuna Pruriens For Parkinsons
Also Check: On Off Phenomenon
Definition Of Wpw Syndrome3
-
Symptoms suggestive of recurrent tachycardias in addition to the following ECG characteristics
-
Shortened P-R interval of < 0.12 s
-
Slurred slow rising onset to QRS known as the delta wave
-
A prolonged QRS complex > 0.11 s
The most frequently encountered tachycardia in WPW syndrome is an atrioventricular re-entrant tachycardia . The arrhythmia uses the AVN and accessory pathway to form a re-entry circuit triggered by an appropriately timed ectopic. This re-entry circuit maybe classified as either orthodromic or antidromic depending on whether the ventricles are activated via the normal conduction system or the accessory pathway. Orthodromic AVRTs account for most tachycardias in WPW syndrome . Conduction occurs down the AVN and retrogradely up the accessory pathway producing a narrow complex tachycardia . The QRS morphology is normal during the arrhythmia because ventricular activation has occurred through the normal pathway. The rate is usually between 140 and 250 beats per minute . Inverted P waves may be visible deforming the ST segment indicating that atrial depolarisation occurs later than ventricular depolarisation. In a patient with a narrow complex tachycardia the presence of such late P waves is frequently the only ECG evidence that the patient has an accessory pathway rather than a much more common atrioventricular nonre-entrant tachycardia .
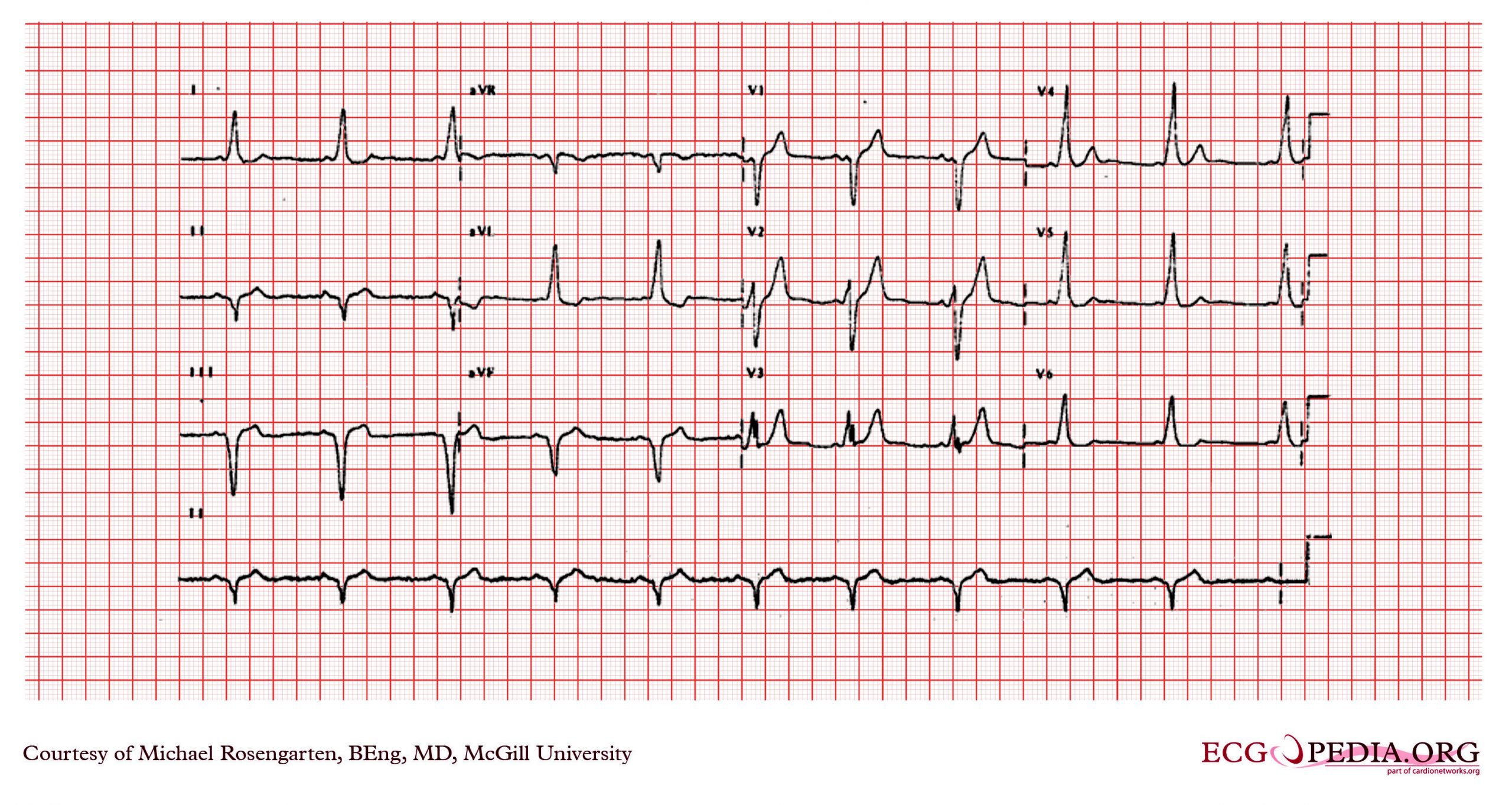
Figure 6
BCT with delta wave.
What Are The Symptoms Of Wolff
Symptoms occur only when the heart beats abnormally fast, so most of the time people have no symptoms. Episodes can start suddenly and last for a few seconds or several hours. They often happen during exercise. When symptoms do occur, they include rapid heartbeat, heart palpitations or heart fluttering, lightheadedness, chest pain, fatigue, fainting, dizziness, anxiety, loss of consciousness, and breathing problems. Sudden death can occur.
Also Check: Parkinson Bicycle Cleveland Clinic
Risk Assessment And Need For Ablation
If AF is induced during either an intraesophageal or an EPS, the shortest RR interval between two consecutive preexcited QRSs is measured. If the interval is less than 220 ms, then the risk of sudden death due to VF is believed to be high. Specifically, according to one study, the most discriminating predictor of VF in patients with WPW syndrome was the shortest RR interval during AF of 172 ± 23 ms . Those patients were considered to be at high risk for developing VF and sudden death should AF occur.
A study of asymptomatic children with WPW pattern who underwent EPS for risk stratification reported that a high proportion of subjects experienced sustained AVRT, AF, or both, with the shortest RR between two consecutive preexcited QRSs being 230-250 ms . The authors concluded that those results may be indicative of the necessity of RF ablation in all asymptomatic individuals with WPW pattern.
Are There Different Types Of Accessory Pathways
Lown, B. The syndrome of short P-R interval, normal QRS complex and paroxysmal rapid heart action. Circulation. vol. 5. 1952 May. pp. 693-706.
James, TN. Morphology of the human atrioventricular node, with remarks pertinent to its electrophysiology. Am Heart J. vol. 62. 1961. pp. 756-71.
Lev, M, Leffler, WB, Langendorf, R. Anatomic findings in a case of ventricular preexcitation terminating in complete atrioventricular block. Circulation. vol. 34. 1966. pp. 718-33.
Murdock, CJ, Leitch, JW, Teo, WS. Characteristics of accessory pathways exhibiting decremental conduction. Am J Cardiol. vol. 67. 1991. pp. 506-10.
Ross, DL, Uther, JB. Diagnosis of concealed accessory pathways in supraventricular tachycardia. Pacing Clin Electrophysiol. vol. 7. 1984. pp. 1069-85.
Anderson, RH, Becker, AE, Brechenmacher, C. Ventricular pre-excitation: a proposed nomenclature for its substrates. Eur J Cardiol. vol. 3. 1975. pp. 27-36.
Mahaim, I, Benatt, A. Nouvelles recherches sur les connections superieures de la branche du faisceau de His-Tawara avec cloison interventriculaire. Cardiologia. vol. 1. 1937. pp. 61
Also Check: Similar To Parkinsons
Atrial Fibrillation And Wpw
Patients with Wolff-Parkinson-White syndrome have an accessory pathway or a bypass tract that connects the electrical system of the atria directly to the ventricles, thereby allowing conduction to avoid passing through the AV node.
In normal individuals, when the sinus node creates an action potential it must pass through the AV node to get to the ventricles. When an accessory pathway is present, the sinus node action potential can pass through the bypass tract before the AV node, which causes the ventricles to become depolarized quickly. This is termed pre-excitation and results in a shortened PR interval on the ECG.
The combination of WPW and atrial fibrillation can potentially be fatal, especially if AV blocking agents are given . The medical treatment is procainamide, although electrical cardioversion is reasonable, especially if hemodynamically unstable.
In patients with WPW and atrial fibrillation, the erratic atrial action potentials can conduct through the accessory pathway very quickly . Therefore, WPW patients who develop atrial fibrillation have higher ventricular rates than those without WPW. If an AV blocking agent is given, fewer atrial action potentials will pass through the AV node and more will pass through the accessory pathway, paradoxically increasing the ventricular rate potentially causing ventricular fibrillation which is a fatal, hemodynamically unstable rhythm. Procainamide or electrical cardioversion is recommended in these situations.
Which Congenital Heart Disease Is Associated With Pre
Left ventricular pre-excitation was recorded in 18 cases: 8 in the lateral zone, 5 in the anterior paraseptal and 5 in the posterior paraseptal zones. WPW and congenital heart disease: Out of 20 cases of Ebsteins anomaly, 5 cases of WPW were observed: 4 right posterior and 1 right lateral pre-excitations.
You May Like: Pfnca Wellness Programs
How Can We Tell The Location Of The Ap Based On The Superficial 12
The ECG hallmark of an antegradely conducting AP is the delta wave along with a shorter than usual PR interval and a widened QRS complex. Conversely, the presence of retrograde conduction only in an AP will not be apparent on a surface ECG during sinus rhythm . Whereas ECG during ORT has a normal QRS complex with retrogradely conducting P wave after the completion of the QRS complex in the ST segment or early in the T wave, the QRS during ART is fully preexcited.
Numerous algorithms have been described to localize the site of the AP using the axis of the delta wave and QRS morphology. The location of the AP along the AV ring is classified variously into five or ten regions, which can be broadly divided into those on the left and the right of the AV groove. Distribution along these lines is not homogenous. Some 46% to 60% of the pathways are found on the left free wall space. Nearly 25% are within the posteroseptal and midseptal spaces, 15% to 20% in the right free wall space, and 2% in the anteroseptal space.
The positive predictive value of these algorithms is better when the delta wave polarity is included and when algorithms involve fewer than six locations. Two simple algorithms that include both the delta wave axis and the QRS axis are shown . For the purpose of localization of the APs, delta wave is defined as the first 20 ms of the earliest QRS deflection.
Dont Miss: Signs Of Parkinsons Disease
What Are The Effects Of This Problem On My Child’s Health
The information about supraventricular tachycardia applies to children with WPW. In babies, the problem resolves on its own about 50% of the time.
Rarely, WPW can cause sudden cardiac death. This can occur only if 1) the extra pathway can conduct an electrical signal very quickly from the atria to ventricles and 2) the person has an arrhythmia called atrial flutter/fibrillation. In atrial fibrillation/flutter, the upper chambers of the heart beat very fast, from 300 to 600 beats per minute. If the pathway can conduct very rapidly to the lower chambers , it could result in a life-threatening heart rhythm called ventricular fibrillation. In patients without WPW, the ventricles are protected from the fast atrial rates by the AV-node since is can only conducts a fraction of the signals . Sudden cardiac death from WPW is extremely rare in the first few years of life.
Read Also: Parkinson Silverware
What Causes Wpw Syndrome
When the heart beats, its muscular walls contract to force blood out and around the body. They then relax, allowing the heart to fill with blood again. This is controlled by electrical signals.
In WPW syndrome, there’s an extra electrical connection in the heart, which allows electrical signals to bypass the usual route and form a short circuit. This means the signals travel round and round in a loop, causing episodes where the heart beats very fast.
The extra electrical connection is caused by a strand of heart muscle that grows while the unborn baby is developing in the womb.
It’s not clear exactly why this happens. It just seems to occur randomly in some babies, although rare cases have been found to run in families.