What Is The Self
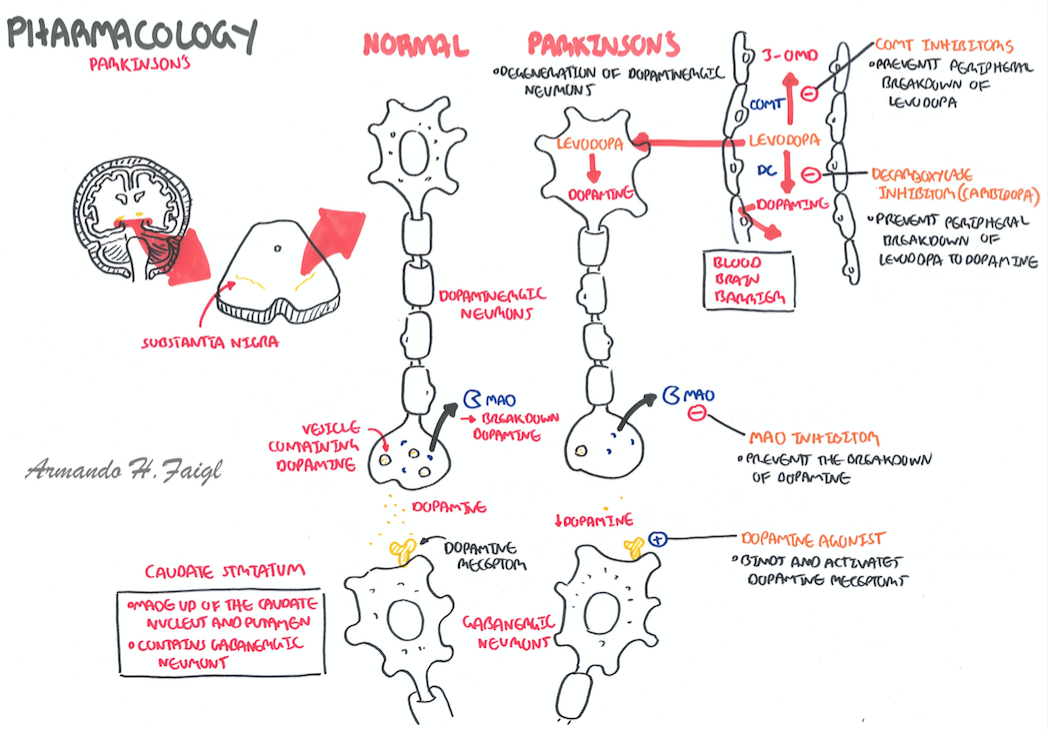
Protein in the diet may affect the absorption of levodopa, the major medication used to treat Parkinson’s disease. Fluctuations in the level of levodopa may worsen some behavioral and cognitive symptoms. A low-protein diet may reduce fluctuations in dopamine levels. In some patients with these fluctuations, dietary changes can improve symptoms. However, it is important to ensure that the person is getting adequate calories and other nutrients.
People with Parkinson’s disease should remain as active as possible. Physical therapy helps the person maintain mobility.
In general, people with Parkinson’s disease plus dementia should no longer drive vehicles. Movement problems may prevent quick reactions in hazardous driving situations. Certain medications, especially those given to treat symptoms of dementia, may make them less alert. However, this should be determined on an individual basis and in compliance with the laws of the state.
YOU MAY ALSO LIKE
Is Dementia A Symptom Of Both
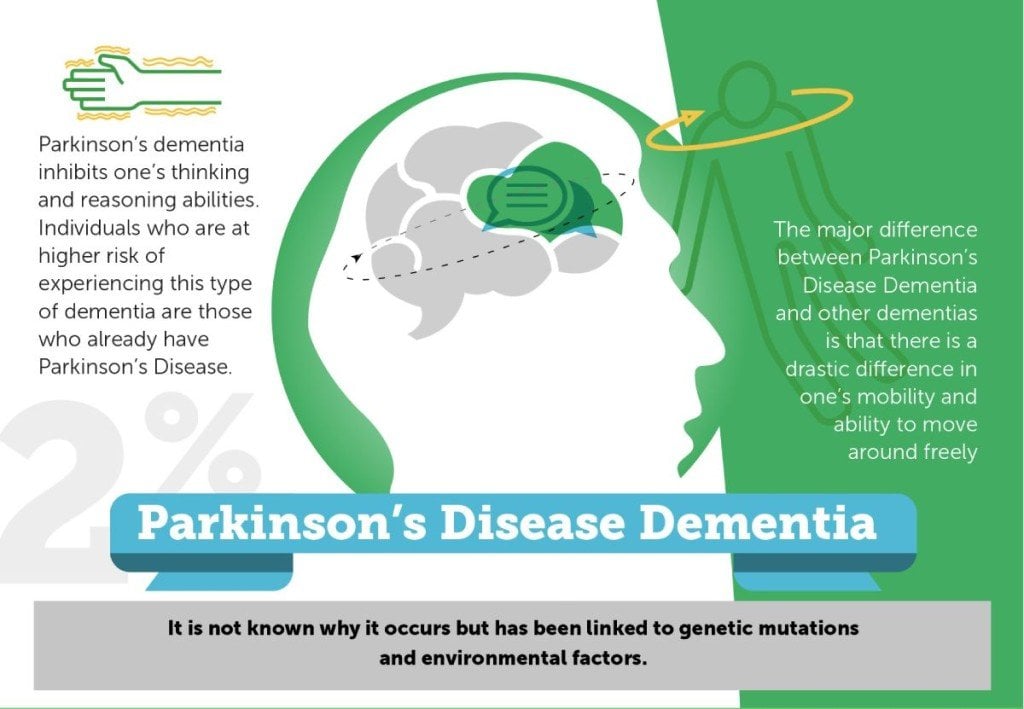
One of the biggest similarities between PD and LBD is dementia. Some studies have found that approximately 78 percent of PD patients will eventually develop dementia.4 More specifically, almost half of Parkinsons patients will develop a certain type of dementia called Parkinsons Dementia, usually 10-15 years after their initial PD diagnosis.3 People with Parkinsons Dementia commonly experience poor memory and concentration, slowed thinking, confusion, depression, emotional changes, delusions, and visual hallucinations.
Parkinsons dementia is different than LBD, mainly in which symptoms occur first . Patients with Parkinsons Dementia will first show Parkinsons motor symptoms, followed by dementia many years after diagnosis. Conversely, LBD patients will first show dementia symptoms and may show motor symptoms later.3
Dementia Outcomes According To Baseline Cognitive And Psychiatric Variables
Of those diagnosed with dementia, 11 were diagnosed according to Level 2 MDS criteria, and 16 according to Level 1 criteria. Patients destined to develop dementia were older at baseline and more often male . As expected, those with baseline MCI had increased dementia risk . The prevalence of MCI at baseline in the dementia-converted group was 81.5% compared with 32% in the nondementia group. A baseline history of visual hallucinations , visual illusions , subjective cognitive complaints , thought disorders , and depression also predicted dementia development. Higher apathy scores were observed in the dementia group than in the nonconverted group .
Recommended Reading: Medicinal Plants For Parkinson’s Disease
Rem Sleep Behavior Disorder An Early Symptom Of Parkinsons Disease
Research suggests thatREM sleep behavior disorder is an early symptom of Parkinsons disease. The findings suggest that nearly half of those with RBD will go on to develop Parkinsons disease. The study also added that nearly every person with RBD will go on to develop a neurological disorder.
Co-author of the study, Dr. Michael Howell, said, If you get this disorder and live long enough, you will almost certainly get Parkinsons disease or a condition similar to it its an early warning sign.
The main symptom of RBD is acting out dreams when the person should normally be in a paralyzed state. Researchers believe that individuals with RBD have a brain-stem malfunction, which allows for the movement to take place.
Patients with RBD report that movement can range from small hand gestures to violent acts, such as punching or kicking.
To determine if RBD contributes to Parkinsons disease the research team went through over 500 studies published between 1986 and 2014. What they found was 81 to 90 percent of RBD patients went on to develop a neurological disorder.
Parkinsons is caused by the breakdown of certain proteins in neurons that produce dopamine. The protein breakdown is of alpha-synuclein, and RBD is believed to result from the early stages of alpha-synuclein breaking down.
Why Is Proper Follow
A person with Parkinsons disease is supposed to go for regular checkups to his health care professional for the following reasons-
Treatment Progress: The check-ups help the health care professionals to check if the treatment procedure is working or not and also provides an insight about the necessary adjustments to be made.
Detecting New Issues- Regular follow-ups help in detection of new problems with cognition, behavior or mood which might need special treatment.
Planning the Care- The follow-ups provide a platform for caregivers to discuss the problems with respect to the patients care.
Presence of Dementia: It can also be known if the patient is susceptible to dementia with the help of regular checkups.
Dementia: It may happen so that the person with Parkinsons disease developing dementia may not be able to take care of himself or take decisions about his healthcare. Thus, caregivers should be extra careful and follow the regular follow-ups with the doctor.
Also Check: What Foods Should Be Avoided When Taking Levodopa
Medications To Help Treat Parkinsons Disease Psychosis
Your doctor might consider prescribing an antipsychotic drug if reducing your PD medication doesnt help manage this side effect.
Antipsychotic drugs should be used with extreme caution in people with PD. They may cause serious side effects and can even make hallucinations and delusions worse.
Common antipsychotic drugs like olanzapine might improve hallucinations, but they often result in worsening PD motor symptoms.
Clozapine and quetiapine are two other antipsychotic drugs that doctors often prescribe at low doses to treat PD psychosis. However, there are concerns about their safety and effectiveness.
In 2016, the approved the first medication specifically for use in PD psychosis: pimavanserin .
In clinical studies , pimavanserin was shown to decrease the frequency and severity of hallucinations and delusions without worsening the primary motor symptoms of PD.
The medication shouldnt be used in people with dementia-related psychosis due to an increased risk of death.
Psychosis symptoms caused by delirium may improve once the underlying condition is treated.
There are several reasons someone with PD might experience delusions or hallucinations.
Neuropsychological And Behavioral Assessment
All the enrolled patients, at baseline and follow-up, underwent a comprehensive neuropsychological assessment when in on state. Neuropsychological evaluations were performed by neurologists with a specific expertise in neuropsychology and dementia, and the same rater performed both baseline and follow-up assessments.
Patients underwent a Level I MDS criteria evaluation of global cognition using the following tests: the Mini Mental State Examination , the Montreal Cognitive Assessment , and the Frontal Assessment Battery .
According to MDS Level II criteria , two tests for cognitive domains have been performed. The memory domain has been assessed with the Reys Auditory Verbal Learning Test and the Prose recall test with a delayed recall condition the attention domain with the Stroop color-word test and the Trail Making Test part A the executive function domain with the Verbal fluency letter test and the Colored Ravens Progressive Matrices the visuo-spatial function domain with the Clock drawing test and the Copy of figures lastly, the language domain has been assessed with the Aachener Aphasie Test-Naming item and the short version of the Token test .
For each test, details regarding administration procedures and Italian normative data for score adjustment were used. Neuropsychological performances were considered as impaired when the subject scored 2 standard deviation below normality cut-off values.
Don’t Miss: Does Vitamin B12 Help Parkinson’s
Not Everyone With Parkinsons Will Develop Dementia
Despite the fact that the pathology of Parkinsons disease can trigger the development of different types of dementia, not everyone with Parkinsons will develop dementia. About 30 percent of people with Parkinsons will actually not develop dementia at all, as stated by the National Parkinson Foundation.
However, the vast majority of people with Parkinsons may experience some form of cognitive impairment over time, the foundation says.
Symptoms Of Parkinsons Disease Dementia
Signs and symptoms of Parkinsons disease dementia include:
- Mental inflexibility
- Short-term memory issues and memory loss
- Trouble with decision making
- Executive function difficulty
- Slow processing speed
- Inattention
- Visual processing difficulty
Non-motor symptoms that can be associated with PDD include:
- Psychosis :
- Hallucinations
- Delusions
Don’t Miss: Parkinson’s Bike Therapy
Autonomic And Constitutional Features
Autonomic dysfunction is a common clinical sign in LBD.20 Symptomatic orthostasis is probably the most serious manifestation of autonomic dysfunction, but other features include decreased or increased sweating, excessive salivation , seborrhea, heat intolerance, urinary dysfunction, constipation or obstipation, erectile dysfunction, impotence, and changes in libido. Interestingly, constipation may precede any cognitive or motor symptoms by more than a decade. Other constitutional features include anosmia and excessive daytime sleepiness.
Things You Should Know About The Link Between Parkinsons And Dementia
Both Parkinsons disease and dementia were ravaging the brain and behavior of actor Robin Williams before his death, but at the time, he didnt realize he had the latter.
Despite the fact that the signs of this combination can be confusing, the double diagnosis of Parkinsons and dementia impacts a large number of people. Of the one million people who have Parkinsons in the U.S., 50 to 80 percent may have dementiaeither as a result of Parkinsons pathology, or separately.
Robin Williams widow, Susan, wrote an editorial published in Neurology that was addressed to neurologists after his death. In it, she shared what it was like seeing her husband experience both Parkinsons disease and Lewy body dementia firsthand.
My hope is that it will help you understand your patients along with their spouses and caregivers a little more, Susan wrote.
Williams was first diagnosed with Parkinsons disease, which at first seemed to provide some answers for his out-of-character symptoms.
But it wasnt until after his death that an autopsy revealed he had been in the later stages of Lewy body dementiaa common form of dementia characterized by deposits of Lewy body proteins in the brain, which can impact physical movement, mood, memory and behavior.
I will never know the true depth of his suffering, nor just how hard he was fighting, Susan wrote. But from where I stood, I saw the bravest man in the world playing the hardest role of his life.
Don’t Miss: Prayers For Parkinson’s Disease
Improving Diagnosis With Composite Scores
A diagnostic challenge, particularly outside of expert centers, there are long delays in diagnosing LBD leading to significant burden. Although consensus criteria have excellent specificity, there is no standardized way to assess symptoms, reducing sensitivity. We developed the LB Composite Risk Score 21 from autopsy-verified cases to improve the ability to detect LBD in clinic and research populations .
Figure. Diagnostic Tools for Dementia With Lewy Bodies. The Lewy Body Composite Risk Score is a 10-item questionnaire to capture signs and symptoms associated with Lewy body pathology. A score of 3 or greater represents a high probability that Lewy bodies are contributing to cognitive decline . Comparison of MRI in Alzheimers disease and dementia with Lewy bodies demonstrates less cortical and hippocampal atrophy in DLB . Comparison of dopamine transporter single photon emission tomography in AD and DLB shows decreased dopamine uptake in the basal ganglia in DLB vs normal uptake in AD.
Wait So What Is Parkinsonism
Parkinsonism refers to the motor symptoms that are typically associated with PD, such as tremors, stiffness, and walking/balance problems. Both PD and LBD are forms of Parkinsonism, meaning that PD patients and LBD patients may experience these motor symptoms.2 Because the Parkinsonism motor symptoms of PD and LBD can be very similar, it can be difficult to differentiate between the two conditions.
Don’t Miss: Similar To Parkinsons
Neurochemical Deficits In Pdd
Degeneration of subcortical nuclei in PD leads to dopaminergic, cholinergic, noradrenergic, and serotoninergic deficits. Of them, cholinergic deficits due to degeneration of the nucleus basalis of Meynert have been the most involved in PDD. In early neuropathological studies, PDD patients showed more NMB cholinergic neuronal depletion when compared with AD and non-demented PD.33,34 A greater reduction of choline acetyltransferase activity in frontal and temporal cortex was found in PDD than in PD without dementia.35 Mattila et al reported reduced choline acetyltransferase activity in the hippocampus, prefrontal cortex, and temporal cortex in PD. Reduction in the frontal cortex correlated signicantly with the degree of cognitive impairment.36 Not only pathological studies but also neuroimaging studies have pointed out a role for a cholinergic deficit in cognition in PD. Both PD and PDD have cholinergic neuron decits with vesicular acetylcholine transporter and acetylcholinesterase 37,38 imaging being the decreased VAChT more important and extensive in the cerebral cortex of PDD subjects.39
There are not consistent findings supporting an association between dementia and other monoaminergic systems.
What Are The Symptoms Of Parkinson Disease
Parkinson disease symptoms usually start out mild, and then progressively get much worse. The first signs are often so subtle that many people don’t seek medical attention at first. These are common symptoms of Parkinson disease:
- Tremors that affect the face and jaw, legs, arms, and hands
- Slow, stiff walking
Don’t Miss: Parkinson’s Hallucinations Commercial
What Are The Complications Of Parkinson Disease
Parkinson disease causes physical symptoms at first. Problems with cognitive function, including forgetfulness and trouble with concentration, may arise later. As the disease gets worse with time, many people develop dementia. This can cause profound memory loss and makes it hard to maintain relationships.
Parkinson disease dementia can cause problems with:
- Speaking and communicating with others
- Problem solving
- Forgetfulness
- Paying attention
If you have Parkinson disease and dementia, in time, you likely won’t be able to live by yourself. Dementia affects your ability to care of yourself, even if you can still physically do daily tasks.
Experts don’t understand how or why dementia often occurs with Parkinson disease. Its clear, though, that dementia and problems with cognitive function are linked to changes in the brain that cause problems with movement. As with Parkinson disease, dementia occurs when nerve cells degenerate, leading to chemical changes in the brain. Parkinson disease dementia may be treated with medicines also used to treat Alzheimer’s disease, another type of dementia.
Progression From Normal Cognition To Mci
Throughout the entire sample of 139 non-demented PD patients, the prevalence of PD-MCI at baseline was 44.6% and 39.2% considering only newly diagnosed patients these rates were close to those reported for the whole PACOS cohort , as well as those regarding other studies .
A lower frequency of MCI at baseline was reported in the Norwegian study , while the study by Cholerton et al. reported a higher prevalence of MCI. The latter result is probably due to the lower cut-off point used for the impairment on specific neuropsychological test .
According to literature data, the most frequent type of MCI at baseline was the multiple domain , both amnestic and non-amnestic, representing the 49.1% and 20.0%, respectively.
At follow-up, 33.3% of PD-NC at the baseline developed MCI and considering only the newly diagnosed patients the frequency was 30.3%. These similar rates probably account for the short disease duration and mild motor impairment of the patients enrolled in the study. To the best of our knowledge, incidence rate of MCI among PD-NC was estimated only for the Norwegian study where an incidence rate of 68.9/1000 pyar was recorded. This rate was lower with respect to our study, but it should be underlined that also a lower frequency of MCI at baseline was reported.
Also Check: On Off Phenomenon In Parkinson’s Disease
Patient Selection And Enrollment
Patients were recruited from the Movement Disorders Clinics of the McGill University Health Centre and the Centre Hospitalier de lUniversité de Montréal . Patients with UK Bank Criteriadefined parkinsonism, with idiopathic PD determined as the most likely cause, were included. Patients were excluded if they had baseline dementia according to Movement Disorder Society criteria or if an alternative cause of parkinsonism was diagnosed after comprehensive assessment.
What Is Lewy Body Dementia
LBD is a chronic, neurodegenerative cognitive disorder, and is the 3rd most common form of dementia.3 Unlike most other forms of dementia, people with LBD have Lewy bodies in the brain. Lewy bodies are abnormally-folded proteins found in the nerve cells of the brain.2 Patients with LBD may experience memory/cognitive problems, visual hallucinations, and Parkinsonism symptoms.4
Don’t Miss: Parkinson Silverware
Progression From Mci To Pdd
Considering only the 55 patients with PD-MCI at baseline, 14 developed PDD at follow-up , while 9 reverted to PD-NC. The incidence rate of PDD in patients with MCI at baseline was 123.5/1000 pyar , while the incidence rate of PDD among PD-NC at baseline was 24.3/1000 , giving a RR of 5.09 .
Of the 9 reverters, 3 were aMCIsd, 4 were aMCImd and 2 were naMCImd . No significant differences regarding clinical and demographic characteristics at baseline between reverters and PD-MCI, irrespective of whether the patients developed PDD or not, were found.
Comparison With Other Dementias

Dementia is the result of physical changes in the brain that can lead to memory loss and an inability to think clearly.
Several types of dementia exist, including:
PD dementia has different symptoms to other types.
Alzheimers dementia, for example, impairs memory and language. PD dementiam on the other hand, affects problem-solving, the speed at which thoughts occur, memory, and mood, alongside other important cognitive functions.
Dementia with Lewy bodies and Parkinsons disease dementia are similar in that the Lewy Bodies might be present in both forms.
However, whether the disease causes Lewy bodies or if Lewy bodies cause the disease symptoms is unclear. Researchers also believe that the way the Lewy bodies form in Parkinsons disease dementia is different from those in Lewy body dementia.
Don’t Miss: Pfnca Wellness Programs
What Is Aggressive Parkinsons Disease
As written above, Parkinsons dementia aggression is that form of Parkinsons which makes the patient exhibit aggressive behavior. They vent out their aggression either verbally or physically, in the various forms that have been written above. Besides verbal and physical outbursts, PD Dementia patients are also prone to hallucinating caused by the medication administered. Hallucinations in PD Dementia patients primarily occur because of the effects of dopaminergic agents for motor symptoms.
Loss of dopamine neurons in the ventral tegmental area is one of the likeliest of all neuropathological causes as changes in serotonin and norepinephrine systems are not. For the uninitiated, the ventral tegmental area is the origin of the mesolimbic dopaminergic projection. Plenty of studies have gone into analyzing the cause behind the aggression in PD Dementia patients. Depression in PD Dementia patients has been identified due to changes in the medial frontal cortex and the anterior cingulate. Akinetic-rigid variants have been found in patients showing signs of major depression.