Whats Different About Young
The age of diagnosis matters for a variety of reasons, from probable causes of early cases to symptoms and treatment:
- Genetics. As with any case of Parkinsons disease, the exact cause is usually unknown. That said, The young-onset cases of Parkinsons disease are, on average, a bit more likely to be familial or genetic, says Gregory Pontone, M.D., director of the Johns Hopkins Movement Disorders Psychiatry Clinic.
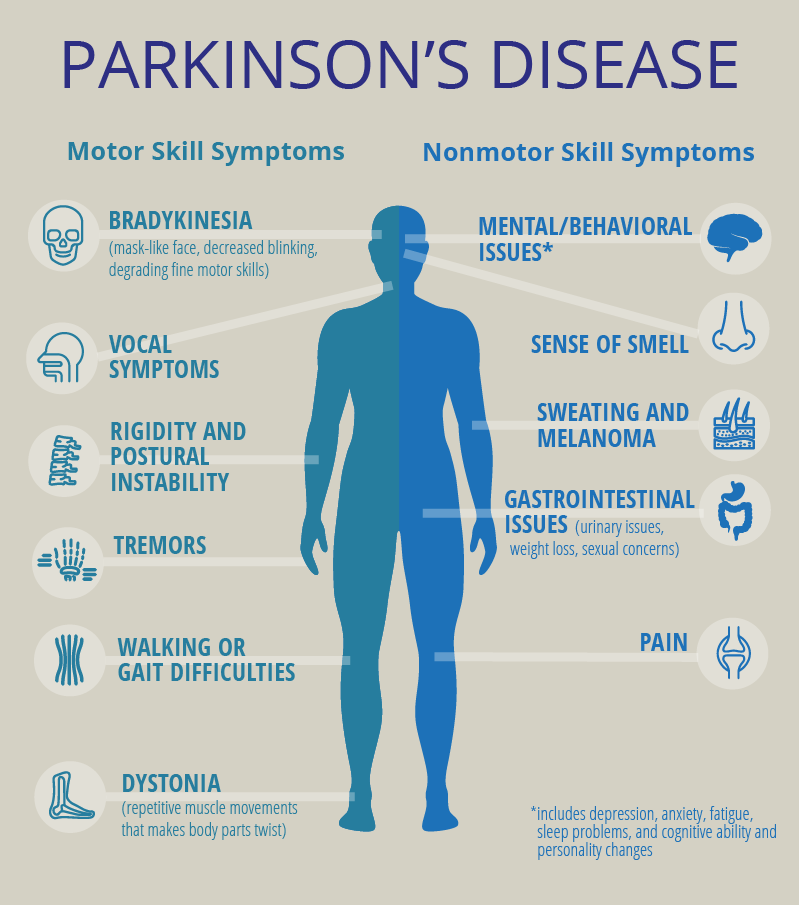
- Symptoms. In many patients with YOPD, dystonia is an early symptom. People with YOPD also report more dyskinesia . They also tend to exhibit cognitive problems, such as dementia and memory issues, less frequently.
- Progression. Patients with young-onset Parkinsons appear to have a slower progression of the disease over time, says Pontone. They tend to have a milder course, staying functional and cognitively intact for much longer.
- Treatment. Most patients with Parkinsons take the medication levodopa. However, other drugs, such as MAO-B inhibitors, anticholinergics, amantadine, and dopamine receptor agonists, may be used before levodopa.
How Is Parkinson Disease Treated
Dopaminergic medications are the mainstay of symptomatic therapy for motor symptoms in Parkinson disease. The mechanisms of action, starting and target doses and adverse effects of medications are summarized in Appendix 2, available at www.cmaj.ca/lookup/suppl/doi:10.1503/cmaj.151179/-/DC1. Discovered in the 1960s, levodopa was the first symptomatic treatment for Parkinson disease, followed by the availability of dopamine agonists and monoamine oxidase B inhibitors. Until recently, the decision regarding which treatment to initiate has been debated. There is no one medication that is recommended for treatment initiation currently, but factors such as symptom severity, embarrassment, ability to perform activities, cost and patient preference should be taken into account. If symptoms are very mild, the patient may choose not to begin therapy.,
Because patients with early-onset disease are more likely to develop levodopa-induced abnormal movements , dopamine agonists are often introduced as initial treatment however, this early advantage of dopamine agonists over levodopa diminishes over time . There is also some controversial evidence for neuroprotection with the monoamine oxidase B inhibitor rasagiline at the 1 mg daily dose however, its cost is not covered in most provinces and may require application to the exceptional access program, as is done in Ontario.
What Causes Parkinson’s Disease
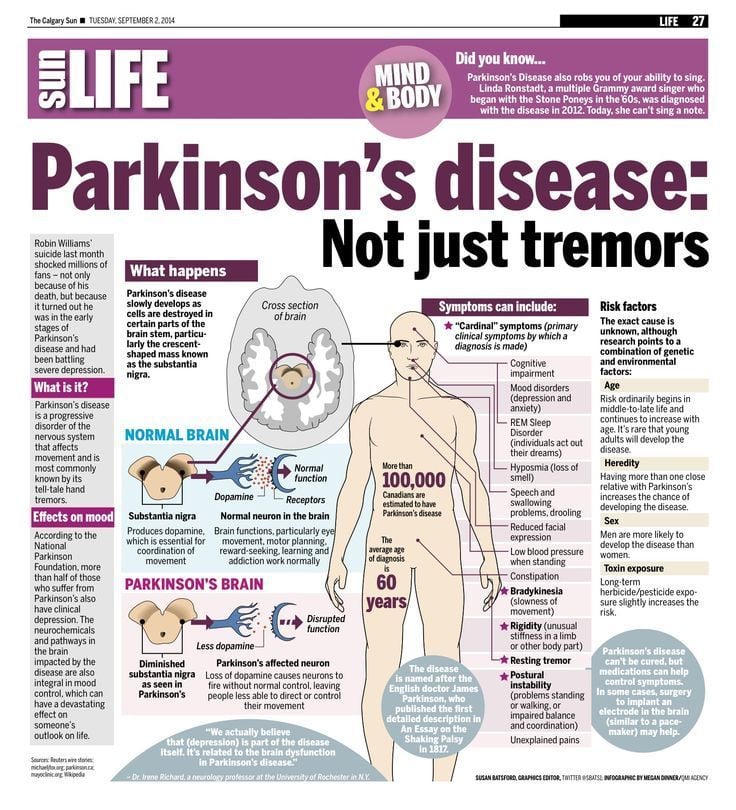
Parkinson’s disease occurs when nerve cells, or neurons, in an area of the brain that controls movement become impaired and/or die. Normally, these neurons produce an important brain chemical known as dopamine. When the neurons die or become impaired, they produce less dopamine, which causes the movement problems of Parkinson’s. Scientists still do not know what causes cells that produce dopamine to die.
People with Parkinson’s also lose the nerve endings that produce norepinephrine, the main chemical messenger of the sympathetic nervous system, which controls many functions of the body, such as heart rate and blood pressure. The loss of norepinephrine might help explain some of the non-movement features of Parkinson’s, such as fatigue, irregular blood pressure, decreased movement of food through the digestive tract, and sudden drop in blood pressure when a person stands up from a sitting or lying-down position.
Many brain cells of people with Parkinson’s contain Lewy bodies, unusual clumps of the protein alpha-synuclein. Scientists are trying to better understand the normal and abnormal functions of alpha-synuclein and its relationship to genetic mutations that impact Parkinsons disease and Lewy body dementia.
Recommended Reading: Parkinson’s And Sense Of Smell
Sidebar: Morris K Udall Centers Of Excellence For Parkinson’s Disease Research
The Morris K. Udall Parkinsons Disease Research Act of 1997 authorized the NIH to greatly accelerate and expand PD research efforts by launching the NINDS Udall Centers of Excellence, a network of research centers that provide a collaborative, interdisciplinary framework for PD research. Udall Center investigators, along with many other researchers funded by the NIH, have made substantial progress in understanding PD, including identifying disease-associated genes investigating the neurobiological mechanisms that contribute to PD, developing and improving PD research models, and discovering and testing potential therapeutic targets for developing novel treatment strategies.
The Udall Centers continue to conduct critical basic, translational, and clinical research on PD including: 1) identifying and characterizing candidate and disease-associated genes, 2) examining neurobiological mechanisms underlying the disease, and 3) developing and testing potential therapies. As part of the program, Udall Center investigators work with local communities of patients and caregivers to identify the challenges of living with PD and to translate scientific discoveries into patient care. The Centers also train the next generation of physicians and scientists who will advance our knowledge of and treatments for PD. See the full list of Udall Centers.
What Is Essential Tremor And How Is It Different To A Parkinsons Tremor
A tremor is a rhythmical, involuntary movement that affects a part of the body, such as the hand.
Essential tremor is the most common type of tremor. Its most noticeable when your hands are doing something and it usually affects both the right and left sides of the body equally. Essential tremors often lessen when your body is resting.
Unlike an essential tremor, a Parkinsons tremor is most obvious when the affected body part is resting and tends to be less noticeable with movement. It usually starts on one side of the body and may progress to the other side as Parkinsons develops.
The time it takes to get a diagnosis can vary from person to person. Some people may receive a diagnosis of Parkinsons quite quickly, but for others it may be a long process. This can be due to a number of things, including your medical history, your age and what symptoms you have.
Your specialist may wish to rule out other causes of your symptoms first and see how you respond to treatment. This may take some time, and, as already mentioned, there is currently no definitive test for Parkinsons.
How you respond to treatment may help your specialist make a diagnosis. Keeping a diary or record of your symptoms will give the specialist more information to guide their decision.
Because the symptoms of Parkinsons are sometimes similar to other forms of parkinsonism, people can sometimes be misdiagnosed.
Also Check: Do I Have Parkinson’s Disease Test
What Is The Average Age To Get Parkinsons Disease
Parkinsons disease indicates a neurodegenerative disorder affecting predominately various dopamine-producing neurons in particular brain areas known commonly as substantia nigra.
Symptoms in this case develop generally slow for many years. In addition, progression of various symptoms is slightly different among different persons because of the diversity prevails in the disease. People suffering from Parkinsons disease problem usually deal with-
Tremor usually while taking rest and pill rolling type of tremor in the hands. However, the patients may even deal with other tremor forms, which are-
- Slow body movements.
- Rigidity in limbs.
- Problems in balance of body and gait.
Main reason behind the Parkinsons disease problem is entirely unknown. Despite no cure is available until now, treatment options in case of Parkinsons disease may vary largely, which may include surgical procedures and medications. The problem itself is not a dreadful one its complications may sometimes become serious.
What Are The Management Options For Canadians Living With Parkinsonism
There is currently no cure for Parkinsons disease and most other parkinsonism cases. However, treatment options are available to help mitigate the symptoms and health impacts associated with these conditions. Most often the primary treatment is pharmacological, but it may also include other therapeutic options and, in the case of Parkinsons disease, surgical interventions. Studies have shown that specially tailored exercise programs, supervised by physiotherapists or other trained professionals, may help affected individuals maintain or improve their physical functionality and general well-being.Footnote 2 Footnote 3 Footnote 4 Footnote 5
Box 1: What’s in the data?
The data used in this publication are from the Canadian Chronic Disease Surveillance System , a collaborative network of provincial and territorial chronic disease surveillance systems, led by the Public Health Agency of Canada . The CCDSS identifies chronic disease cases from provincial and territorial administrative health databases, including physician billing claims and hospital discharge abstract records, linked to provincial and territorial health insurance registry records using a unique personal identifier. Data on all residents eligible for provincial or territorial health insurance are captured in the health insurance registries.
Definition of diagnosed parkinsonism, including Parkinsons disease, in the CCDSS
Also Check: Parkinson’s Disease How Long To Live
How Is Parkinsons Diagnosed
Doctors use your medical history and physical examination to diagnose Parkinson’s disease . No blood test, brain scan or other test can be used to make a definitive diagnosis of PD.
Researchers believe that in most people, Parkinson’s is caused by a combination of environmental and genetic factors. Certain environmental exposures, such as pesticides and head injury, are associated with an increased risk of PD. Still, most people have no clear exposure that doctors can point to as a straightforward cause. The same goes for genetics. Certain genetic mutations are linked to an increased risk of PD. But in the vast majority of people, Parkinsons is not directly related to a single genetic mutation. Learning more about the genetics of Parkinsons is one of our best chances to understand more about the disease and discover how to slow or stop its progression.
Aging is the greatest risk factor for Parkinsons, and the average age at diagnosis is 60. Still, some people get PD at 40 or younger.
Men are diagnosed with Parkinsons at a higher rate than women and whites more than other races. Researchers are studying these disparities to understand more about the disease and health care access and to improve inclusivity across care and research.
Aging is the greatest risk factor for Parkinsons, and the average age at diagnosis is 60. Still, some people get PD at 40 or younger.
The Michael J. Fox Foundation has made finding a test for Parkinsons disease one of our top priorities.
What Are The Different Stages Of Parkinsons Disease
Each person with Parkinsons disease experiences symptoms in in their own unique way. Not everyone experiences all symptoms of Parkinsons disease. You may not experience symptoms in the same order as others. Some people may have mild symptoms others may have intense symptoms. How quickly symptoms worsen also varies from individual to individual and is difficult to impossible to predict at the outset.
In general, the disease progresses from early stage to mid-stage to mid-late-stage to advanced stage. This is what typically occurs during each of these stages:
Early stage
Early symptoms of Parkinsons disease are usually mild and typically occur slowly and do not interfere with daily activities. Sometimes early symptoms are not easy to detect or you may think early symptoms are simply normal signs of aging. You may have fatigue or a general sense of uneasiness. You may feel a slight tremor or have difficulty standing.
Often, a family member or friend notices some of the subtle signs before you do. They may notice things like body stiffness or lack of normal movement slow or small handwriting, lack of expression in your face, or difficulty getting out of a chair.
Mid stage
Mid-late stage
Standing and walking are becoming more difficult and may require assistance with a walker. You may need full time help to continue to live at home.
Advanced stage
Also Check: Ultrasound Treatment For Parkinson’s Disease
Parkinson’s Before Age 50
When someone is diagnosed with Parkinson’s before their 50th birthday, they have what’s called “early onset Parkinson’s disease.” Only about 5% to 10% of everyone with Parkinson’s has the early-onset form of the disease.
Only about 2% of those diagnosed with Parkinson’s are under the age of 40. However, it’s possible that doctors may overlook some people in that age group who actually have Parkinson’s since it’s so unusual to have it so young.
A very few people are diagnosed with Parkinson’s before their 20th birthdays. In these cases, the condition is called “juvenile Parkinson’s disease,” and it tends to run in families. Researchers have identified several genes that are linked to Parkinson’s.
People with early-onset Parkinson’s disease are more likely to have genetic factors that caused their condition. In addition, certain treatments including exercise may be more likely to help younger people with Parkinson’s, because their brains are younger.
Stewart A Factor, DO and William J Weiner, MD. Parkinsons Disease: Diagnosis and Clinical Management: Second Edition Edited by 2008 Demos Medical Publishing.
Parkinson’s Disease Is Difficult To Diagnose
Parkinson’s is a challenge to diagnose since there is no definitive test for it. Blood tests and scans are usually run just to rule out other causes of the symptoms.
If a GP suspects a patient could have Parkinson’s, they may refer them to a neurologist who can make a diagnosis based on medical history, a review of the signs and symptoms and a physical examination. It can help to keep a diary of symptoms leading up to the appointment.
Diagnosing Parkinson’s disease in some people can be a long process.
You May Like: List Of Parkinson’s Drugs
Sidebar: Advances In Circuitry Research
The brain contains numerous connections among neurons known as neural circuits.
Research on such connections and networks within the brain have advanced rapidly in the past few years. A wide spectrum of tools and techniques can now map connections between neural circuits. Using animal models, scientists have shown how circuits in the brain can be turned on and off. For example, researchers can see correlations between the firing patterns of neurons in a zebrafishs brain and precise behavioral responses such as seeking and capturing food.
Potential opportunities to influence the brains circuitry are starting to emerge. Optogenetics is an experimental technique that involves the delivery of light-sensitive proteins to specific populations of brain cells. Once in place, these light-sensitive proteins can be inhibited or stimulated by exposure to light delivered via fiber optics. Optogenetics has never been used in people, however the success of the approach in animal models demonstrates a proof of principal: A neural network can be precisely targeted.
Thanks in part to the BRAIN Initiative, research on neural circuitry is gaining momentum. The Brain Research through Advancing Innovative Neurotechnologies Initiative is accelerating the development and application of new technologies that enable researchers to produce dynamic pictures of the brain that show how individual brain cells and complex neural circuits interact at the speed of thought.
NIH Publication No. 15-5595
Causes Of Early Onset Parkinsons Disease
Its unclear exactly what causes Parkinsons at any age. Genetic factors, environmental factors, or some combination of the two may play a role. This condition occurs when cells are lost in the part of the brain that produces dopamine. Dopamine is responsible for sending brain signals that control movement.
Certain genes are associated with early onset Parkinsons.
According to the National Parkinson Foundation, studies show that 65 percent of people with Parkinsons who experience onset before age 20 may do so because of a genetic mutation. This organization also suggests this mutation affects 32 percent of people who experience onset between age 20 and 30.
Environmental causes of the condition may include exposure to chemical toxins such as certain insecticides, fungicides, and herbicides.
The U.S. Department of Veterans Affairs recognizes Parkinsons as a disease caused by exposure to Agent Orange. Agent Orange is a synthetic chemical herbicide that was used to spray vegetation and trees during the Vietnam War.
You may have a higher risk of developing Parkinsons if you:
- are a man
Don’t Miss: Parkinson’s Disease And Walking
Incidence Of Parkinsons Disease
Its estimated that approximately four people per 1,000 in Australia have Parkinsons disease, with the incidence increasing to one in 100 over the age of 60. In Australia, there are approximately 80,000 people living with Parkinsons disease, with one in five of these people being diagnosed before the age of 50. In Victoria, more than 2,225 people are newly diagnosed with Parkinsons every year.
How Is Parkinson’s Treated
Although there’s currently no cure for Parkinson’s, treatments are available to help reduce symptoms and maintain quality of life for as long as possible. These include:
- supportive therapies, such as physiotherapy and occupational therapy
- medication
- deep brain stimulation .
If you have mild symptoms of Parkinsons, your doctor might not recommend medication and instead focus on supportive therapy and lifestyle improvements such as exercise and relaxation. As your symptoms progress, you will be prescribed medication.
Don’t Miss: Cluster Headaches Parkinson’s Disease
How Many Canadians Live With Parkinsonism And How Many Are Newly Diagnosed Each Year
Based on the latest estimates available , in 20132014, approximately 84,000 Canadians aged 40 years and older were living with diagnosed parkinsonism and 10,000 Canadians were newly diagnosed with this condition . The age-standardized prevalence was 1.5Footnote i times higher among males than among females , and similarly the age-standardized incidence was 1.7Footnote i times higher among males than females . The epidemiological burden of parkinsonism increases with age. In 20132014, when comparing estimates among Canadians aged 85 years and older vs. those aged 40-44 years, the prevalence of the condition was 169Footnote i times higher in the older age group , while the incidence was 48Footnote i times higher in the older age group .
Figure 1: Prevalence of diagnosed parkinsonism, including Parkinsons disease, by sex and age group, Canada, 20132014
| Age group |
|---|
| 44.7 | 55.1 |
Note: The 95% confidence interval shows an estimated range of values which is likely to include the true value 19 times out of 20. Data source: Public Health Agency of Canada, using Canadian Chronic Disease Surveillance System data files contributed by provinces and territories, July 2017.
How Is The Diagnosis Made
Currently, diagnosis of Parkinson disease is based on clinical features from history and examination, and over time based on the response to dopamine agents and the development of motor fluctuations. Motor manifestations of the disorder begin asymmetrically, and commonly include a resting tremor, a soft voice , masked facies , small handwriting , stiffness , slowness of movements , shuffling steps and difficulties with balance. A classic symptom is resting tremor, usually affecting one upper limb, although 20% of patients do not have it 30% may first present with tremor in a lower extremity, and there may also be a lip, jaw or even tongue tremor at rest., Head and voice tremors are uncommon, and one should consider essential tremor in the differential diagnosis in such cases. Of all the major features, bradykinesia has the strongest correlation with the extent of dopamine deficiency. Diagnosis has been formalized by the criteria of the UK Parkinsons Disease Society Brain Bank, with diagnostic accuracy of up to 90% .
Don’t Miss: Movie Stars With Parkinson’s Disease