The Views And Needs Of People With Parkinson Disease Regarding Wearable Devices For Disease Monitoring: Mixed Methods Exploration
1Centre for Gerontology and Rehabilitation, School of Medicine, University College Cork, Cork, Ireland
2Tyndall National Institute, University College Cork, Cork, Ireland
3Research, Development and Innovation Activities & Physiotherapy Education, Karelia University of Applied Sciences, Joensuu, Finland
4School of Computing, Engineering and Intelligent Systems, Faculty of Computing, Engineering and the Built Environment, Ulster University, Magee, United Kingdom
5Department of Public Health and Clinical Medicine, Umeå University, Umeå, Sweden
Instrumented Detection Of Fluctuations With Wearable Devices In Parkinsons Disease
G. Rigas, D. Kakalou, N. Tachos, K. Tsamis, N. Kostikis, A. Marcante, R. Di Mitri, M. Di Pumpo, S. Konitsiotis, D. Fotiadis
Category:Technology
Objective: The objective of this study is to evaluate the efficacy in fluctuations detection of a system consisting of wearable devices embedding Inertial Measurement Units , designed for Parkinsons disease motor symptoms monitoring.
Background: Parkinsons disease management and treatment are largely based on scale-based symptom rating but this is a subjective and coarse-grain approach. To complement clinical evaluation, automated, objective methods of PD symptom monitoring, through wearable sensors and smart technologies, gain popularity among healthcare professionals. This study evaluates the efficacy of a novel wearable system in detecting dyskinesia and ON/OFF fluctuations .
Results: For fluctuations iUMA differences were significant for non-fluctuating versus healthy, low-fluctuating and high-fluctuating. For iAMS the differences were significant between no-dyskinesia patients and patients with either low or high dyskinesia. The ROC analysis demonstrated that fluctuations and dyskinesia were detected with accuracy 86% and 98% by iUMS and iAIMS with thresholds 10.66 and 0.46, respectively.
An IMU-based system of wearables can effectively detect fluctuating PD patients and it can accurately discriminate dyskinesia from daily activities.
To cite this abstract in AMA style:
Mov Disord.
Things To Consider When Buying Assistive Living Devices
Not every Parkinsons patient is the same. We come from all walks of life and age groups with different needs and desires. So there is no one-size-fits-all solution when it comes to selecting the best aids or devices to make living with Parkinsons easier. To help you guide your decision making, here are some factors to consider:
-
Consider what your symptoms are like. The severity and range of symptoms youre experiencing may be different from the next person. For example, if you have severe fine motor skills issues then an app may not be suited to your needs.
-
Do its functions serve the needs youre looking for? Ask yourself what exactly youre looking for in a device or what your goals are. For example, are you looking for a holistic health device? Or something that will help with a specific aspect of your condition?
-
Are there any additional costs to the device? Some devices may come with an app subscription which may add to the long-term cost of using it.
-
Setup and long-term use logistics. Consider if you will be able to use this device independently. If not, will you be able to enlist the help of a caregiver or loved one to assist you?
Also Check: Fitflop Shoes For Parkinson’s
Existing Treatments Target The Brain
The device in this study isnt the first approach that has involved the delivery of vibrations or pulses of energy to the nervous system, the American Parkinson Disease Association notes.
Two surgical procedures, deep brain stimulation and high-intensity focused ultrasound , have been used for years. In FUS, surgeons apply beams of ultrasound waves to a designated target in the brain, creating enough energy to form a small lesion, which can disrupt abnormal circuitry in people with Parkinsons disease.
Meanwhile, in DBS, a surgeon inserts thin electrodes into the regions of the brain that control movement, the ADPA says. These electrodes, which are connected by a wire to a pulse generator that is implanted under the skin in the chest, deliver tiny electrical pulses that allow the brain to maintain normal movement activity.
Researchers have also explored whether having people with Parkinsons disease exercise on a vibrating platform improves tremor and other symptoms. Results have been mixed so far.
Application : Home And Long
To date, as clinical scales are the gold standard for in-clinical setting assessment of PD, the use of patient-completed symptom diaries is the current gold standard for the home monitoring of the pathology . Recent studies proposed the use of commercial devices such as the Microsoft Kinect sensor as a low-cost solution to assess the movement of Parkinsonian patients, not only in clinical settings, but also at home. Nevertheless, the accuracy of these systems can be considered good in the measurement of spatiotemporal features for gross movements, but it is not acceptable compared to validated motion capture systems, which are the gold standard for fine movement analysis of actions such as hand clasping or finger tapping, which is required in the MDS-UPDRS scale for PD severity evaluation.
Table 9. Papers about home and long-term monitoring.
Recommendations and Trends
The principal aim of the home monitoring is to provide an optimal management of PD. According to literature results, this can be done by observing the development of the pathology through the analysis of data acquired by wearable sensors, which seem to be the best type of devices to adopt. The implementation of a Smart Home, in fact, lowered the users acceptance of the technology and resulted in an invasive system that did not provide a sufficiently high accuracy in observations and also measured numerous irrelevant features .
Also Check: On Off Phenomenon In Parkinsons Disease
Recommended Reading: Does Sam Waterston Have Parkinsons
Could Wearable Technology Help People With Parkinsons
Pedometers and activity trackers are popular among people who want to lose weight or just stay in shape. Could similar devices help people with Parkinsons disease monitor their symptoms, and receive more personalized medical care? An opinion piece published September 1 in the Journal of the American Medical Association makes the case for the potential of body-fixed sensors to improve the lives of people with PD.
Doctors diagnose PD based on hallmark movement symptoms, including tremor|, rigidity|, slowness and balance difficulties. People with PD also experience an array of nonmotor symptoms and side effects, including sleep disturbances and mood changes. But not everyone with PD develops all these symptoms, and the symptoms progress at different rates for different individuals. Thus, it is important to keep track of these changes in order to get the best treatment. Currently, doctors evaluate them using standard rating scales and tests, while people with PD may also keep a diary of symptoms.
Anat Mirelman, Ph.D., and co-authors at Tel Aviv University in Israel, note in their editorial that while such tools are valuable for understanding long-term changes in PD, more subtle symptoms, or changes that fluctuate on a daily or weekly basis, might be overlooked. Other symptoms might not occur during the appointment for example, a doctor might not directly observe a persons dyskinesia or freezing episodes when walking.
What Does It Mean?
Reference
Fitness Test For Objective Evaluation Of Rehabilitation
After selecting the type of exercise, the location, approach, and the intensity duration required to achieve motor benefits, the next relevant concern is how to find a robust evaluation test that correctly shows the results of rehabilitation. The assessment of motor activity in PD has been growing in recent years among research communities. Previous rehabilitation tests have varied with every individual, but researchers have considered the timed up and go test as more efficient. In this test, individuals are asked to perform some tailored motor activities and the positive feedback proves the improvement of specific rehabilitation training. However, the TUG test gives promising results by just counting on the total time taken by patients to complete the task, and addresses some lower extremities dysfunctions. These two factors are not enough for evaluation of PD patients motor recovery. Hence, numerous tests have been proposed in recent years. depicts the type of test for each research study used to predict the amount of benefits of each training.
Also Check: On Off Phenomenon
The Pdmonitor Consists Of:
PD Neurotechnology Ltd implements a quality assurance system, which fulfills the requirements of the Council Directive 93/42/EEC concerning medical devices with respect to the PDMonitor® .
Download the CE certificate for the PDMonitor®here.
Intel Wearable Devices To Aid Parkinson’s Disease Research
The chip maker partners with the Michael J. Fox Foundation for Parkinson’s Research to use wearable devices and data analytics to help monitor patient treatment.
Nick Statt
Former Staff Reporter / News
Nick Statt was a staff reporter for CNET News covering Microsoft, gaming, and technology you sometimes wear. He previously wrote for ReadWrite, was a news associate at the social-news app Flipboard, and his work has appeared in Popular Science and Newsweek. When not complaining about Bay Area bagel quality, he can be found spending a questionable amount of time contemplating his relationship with video games.
Intel’s upcoming wave of wearable technology won’t be aimed at helping the chip maker establish itself in the budding consumer electronics’ space now filling up with smartwatches and fitness bands. Rather, Intel’s devices will serve a grander purpose: helping research on and treatment of neurodegenerative brain disease.
Intel announced Wednesday a partnership with the Michael J. Fox Foundation for Parkinson’s Research, the nonprofit founded in 2000 by the “Back to the Future” movie actor and Parkinson’s advocate who has suffered from the illness since 1991. The goal will be to combine Intel’s hardware and software — specifically an upcoming mobile app, new wearable devices, and a data analytics platform — for a multi-phase research study that will take advantage of monitoring techniques unique to technology.
Get the CNET Mobile newsletter
Don’t Miss: Similar To Parkinsons
Demographic And Clinical Characteristics Of The Sample
Recruitment for the first study began in July of 2016 and the last subject for the final PD study completed the last visit in April of 2018. For the first study, we recruited healthy volunteers by drawing from the local community in Andover, MA and Yorktown Heights, NY, respectively . Sixty healthy volunteers with a mean age of 44 years were enrolled, and 33 were female. Compared with PD participants, healthy volunteers were significantly younger , had a higher level of education and were more evenly balanced with regard to gender .
Table 1 Participant characteristics.
These results emphasize the significant probability of symptom severity fluctuating at a rate that cannot be captured by using diary entries every 30min. Importantly, the same consideration applies to live observations of individuals with PD experiencing motor fluctuations. In other words, these results suggest that even live assessments that are carried out at time intervals of 30min are insufficient to capture the dynamics of tremor, dyskinesia, and bradykinesia, as they evolve over the medication cycle. This observation underlines an important potential advantage of using wearable sensors to track fluctuations in motor symptoms since this approach has potential for generating continuous estimates of the severity of tremor, dyskinesia, and bradykinesia, hence overcoming the limitations of more traditional approaches.
You May Like: How Do You Treat Parkinsons Disease Naturally
Sensoria Smart Sock: More Accurate Activity Tracking
Sensoria Smart Sock.
What we loved about Sensoria:
-
May help clinicians gather more accurate data about Parkinsons patient mobility
-
Currently measures the number of steps, distance walked, time active, and more
The Sensoria Smart Sock was initially designed to help runners improve their form. And because it saw so much success in the fitness field, its undergoing clinical trials to see how it can improve Parkinsons patients outcomes.
To track movements, Sensoria uses smart textile technology that is infused throughout the sock. You can currently pair the sock with an app, so all the data that is collected from the sensors will be consolidated on the app. It can currently give runners all sorts of detailed information about their running technique .
This technology has many potential benefits for Parkinsons patients as it can provide clinicians with similar information theyre often looking out for during gait assessments. Another great benefit is that it can give clinicians live feedback about their patients daily movements. They can get instant data without the need for patients to come into the clinic to do manual assessments.
Sensoria is already available commercially to the fitness market and is currently undergoing trials with the Parkinsons population. Were hopeful about the possibilities of this sock and its definitely a product to look into over the next few years.
Read Also: Does Vitamin B12 Help Parkinson’s
What Types Of Sensors Are Available
There are also multiple methods of collecting the data:
- Data passively captured without a patient having to wear any new sensors for example, capturing typing data by placing software on a patients computer with the patient continuing to interact with the keyboard as he/she normally does. Typing data that is collected can include how long a patient spends touching a key and how long it takes between touching one key and the next.
- Data passively captured by a sensor without the patient having to do any additional tasks the sensor can be placed on the wrist, ankle or trunk. The sensor can also be in the patients cell phone.
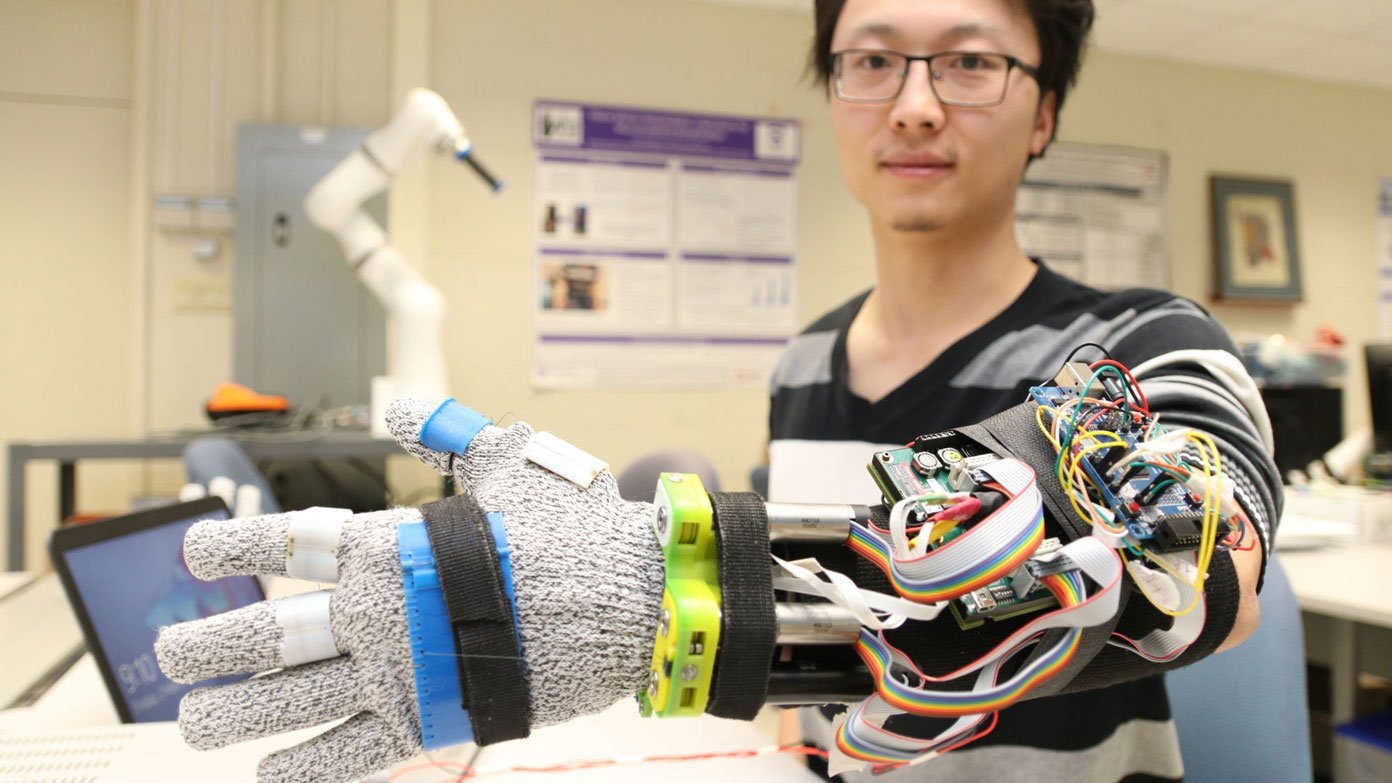
- Data actively captured by a sensor the patient wears the sensor and then performs certain tasks beyond what he/she typically does in his/her daily activities. This could include finger tapping, for example. Sometimes the sensors are too complicated or large for the activities to be performed at home, and the patient needs to come to a neurophysiology lab for the data collection.
B Prognosis/monitoring The Severity Of Symptoms

Assessing the patients condition and severity of symptoms depend primarily on the clinicians judgment and the patient feedback from diaries and memory. The clinicians judgment is subjective , while the patients diary and memory are limited by compliance and recall bias , , . Since this approach may not be completely reliable, objective remote monitoring of PD symptoms is needed to assess disease progression, evaluate the severity of the symptoms, and continuously monitor the PD patients in unsupervised environments. To address these issues, recent work on PD prognosis focuses on the following areas:
-
Home-based or remote monitoring of patients with PD
-
Evaluating the progression of PD for a diagnosed patient
-
Evaluating the severity of PD symptoms for a diagnosed patient
You May Like: Parkinson’s Bike Therapy
Patients And Healthcare Professionals Want Wearable Technology That Eases And Refines Treatments
When asked healthcare professionals about their expectations and outlooks from potentials monitoring and assessment solutions, remarkably all interviewees shed new light on their expectations that the solution could lead for a better or new treatment, and as discussed in section that objective data is needed for expensive treatment as reliable markers therefore, the solution could help improving current treatments or leading for new ones. The expected solution could be used to evaluate treatments efficacy in terms of medications and rehabilitation.
If the nurse altered the medication, and you can detect if the medication reduced patient tremor a bit or knew it did not, or the tremor is bit worse, and that is what you kind of go on, and that is enough, you know, because then you can either try medication try relaxation techniques.
There were some suggestions from healthcare professionals that the solution should be easier to use, provide very concise information, and be easy to interpret. As mentioned in section, one of the main reasons that interviewed healthcare professionals are not using devices available commercially the complexity of interpreting their data and results.
It might be ideal to have something that measured tremor in some way or whether somebody was having an off and on, but it just needs to tell us that quickly and simply, without needing a degree in mastery the charts
Something that could make our life easier
Top Technology Devices For Parkinsons To Know About In 2022
Co-Author: Peter Griffith. helloEd Products & Partnerships. Peter is a specialist in Data Analytics and Technology, living and working in the UK, USA, and Australia. He was diagnosed with Parkinsons in 2017.
I cannot teach anybody anything. I can only make them think. Socrates
Every day, millions of people and their families live with Parkinsons. They strive to stay well and strong and to support each other. Millions more people, as health professionals and medical researchers, dedicate themselves to treat Parkinsons, and find cures.
Using a combination of medication, physical therapy, and lifestyle changes, it may be possible to reduce or delay the impact that Parkinsons Disease has on our lives. We have choices with specialist Parkinsons technology devices, that previous generations never had.
To help you through the process, weve selected 6 well-performing and awarded technology products for the different needs of those living with Parkinsons. We used our smart algorithm to scan over 2000+ health-related technologies and devices and narrowed down the top products based on overall benefit, quality, and features.
View the interactive Parkinsons collectionof 50+ products to consider.We are encouraged at how some of these products allow individuals to achieve things they thought werent possible and by the inspiring stories of people striving to create a better quality of life, and maybe one day a world without Parkinsons.
These include:
Read Also: Adaptive Silverware For Parkinson’s