One Theory To Explain Them All The Vagus Nerve Infection Hypothesis For Chronic Fatigue Syndrome
Receptors on the vagus nerve that sniff out these alarm signals tell the brain an infection is present, which then shuts the body down by sending out signals that slow the body down, tell it to stop moving, stop eating, stop thinking.
Since Chronic Fatigue is a major symptom of Parkinsons Disease too, what this line of research is revealing should therefore be of significance relevance to PwP. Indeed, viral vectors have also been increasingly implicated in the onset of PD over recent years.
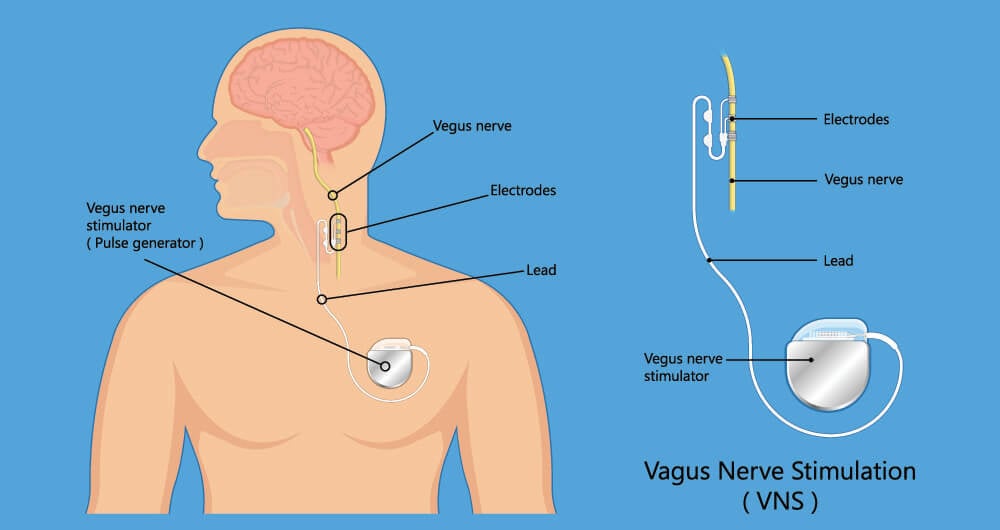
Vagus Nerve Stimulation Techniques
Given all of the above, how do these new understandings help us? Well, the good news is the research tells us we can, after all, do something to help ourselves and to improve our condition/minimize our symptoms. This is because, like muscles, an atrophied Vagus Nerve can be strengthened once more through appropriately exercising and stimulating it. In short, we can improve our Vagal Tone to help us begin to escape from being stuck in the freeze stress response. In other words, we can learn how to relax our way out of the symptoms of PD.
I first learned about this when I found Cheryl Townsleys video on Sparking the Vagus Nerve:
I do this exercise daily, using a standard Pain Gone pen. This re-setting technique demonstrated by Cheryl, shows just how quick and easy VN stimulation techniques can be I spend just 30 seconds a day on this method.
I also quickly learned that deep breathing exercises are integral to VN stimulation, and practising diaphragmatic breathing for a few minutes a day can end up making a large cumulative difference. I particular recommend the method demonstrated by Ellie Drake:
The next video gives a more in depth explanation about the therapeutic values of VN stimulation in tackling illnesses, and suggests coffee enemas as a method for this
Recommended Reading: What Foods Should You Avoid If You Have Parkinsons Disease
The Overlaps Between Stress And Parkinson’s Disease Part 2
However, the details of this are quite involved, so in this first article on the subject, I shall concentrate on the role of the more evolved, or “mammilian”, branch of the VN, but for more information on its Polyvagal nature, please see the pioneering research of Dr Stephen Porges.
The Vagus Nerve is one of the Cranial Nerves, and is by far the largest part of the “parasympathetic” nervous system – see
Also Check: Judy Woodruff Health Problems
The Vital Need To Encourage Relaxation In People With Parkinson’s Disease
for background information on the autonomic nervous systems. The VN regulates the relaxed state of the body and brain, promoting rest, digestion, higher emotionality and sociability. It is responsible for discharging the system from excited states caused by automatic “fight or flight” responses to perceived threats, as governed by the sympathetic nervous system, and also, when the system perceives extreme threat, recovery from the “freeze” or “playing dead” response.
The role of the VN in health should not be understated. When our nervous systems are startled into fight-flight-or-freeze responses, the body quickly becomes inflamed and pain signals result. The ability to rapidly discharge from such a state, once the perceived dangers pass, or not to be hypersensitized to the perception of dangers in the first place, is largely determined by the strength of the VN or “Vagal Tone”. The VN and its functions therefore have major and primary roles in addressing inflammation and detoxifying the body, and in pain reduction.
In fact, all the major symptoms of Parkinson’s can be mapped easily and directly onto a malfunction of one or more of the cranial nerves. Therefore, I suggest that the disease can now be readily and most succinctly understood through the concept that PwP are stuck in freeze and their cranial nerves are critically weak.
Immobilization Due To Dorsal Vagus Activation
Next, we consider in depth the Freeze/Shutdown/Death Feigning function of the human Nervous System which results in immobilization. Again, the following is adapted from Dr Stephen Porges’ work.
Death Feigning is an adaptive response of the Nervous System to life threatening situations.
Occurs once options for fight-or-flight response is eliminated/unavailable, such as when restrained or no obvious escape routes.
A primitive response, which evolved in extinct reptilian progenitors, characterized by appearing to be inanimate/dead.
Triggered when our “neuroception” deems lethal threat, imminent death.
Biological mechanism is via activation of the primitive branch of the Vagus Nerve , creating a “shutdown” state of the autonomic functions, resulting in low respiration and heart rate.
As humans require very significant amounts of oxygen, time spent in the shutdown state is dangerous and damaging, due to inability to oxygenate the blood and deliver enough oxygen to the brain.
Shutdown now may result in apnea , bradycardia , vasovagal syncope , defecation and/or dissociation .
An episode of Death Feigning can have very long term affects, and is strongly implicated in trauma of many kinds.
Shutdown is not a conscious or voluntary response, in the same way passing out in fear is not voluntary, it is a visceral reaction due to inability to fight or flee from perceived lethal danger.
for further details of these aspects.
Also Check: Adaptive Silverware For Parkinson’s
Neural Exercises And Parkinson’s Disease
for more details and lists of specific exercises which I have found have helped me, based on this concept.
The Dorsal Vagus Nerve framework, however, also sets on us on the path towards exploring and understanding the role of trauma in Parkinson’s Disease, and therefore to seek the connections with other conditions such as Post-Traumatic Stress Disorder and Dystonia. in which Dorsal Vagus activation have a role.. Indeed, in speaking to very many people affected by PD around the world about their history before diagnosis, I’ve found that there is almost universally a major physical or emotional trauma lurking in the background.
For more of the supporting science behind this explanation for PD, including how signalling from the gut to the brain via the Dorsal Vagus nerve influence dopamine production in the Substantia Nigra, see
Noninvasive Vagus Nerve Stimulation May Improve Parkinson Disease Symptoms
Noninvasive vagus nerve stimulation may improve gait and other motor symptoms in patients with Parkinson disease, according to the results of biomarker research published in Nature.
Neurostimulation is already used to treat epilepsy, migraine, and cluster headache. The researchers hypothesized that nVNS may address neuroinflammation in Parkinson disease.
The randomized, double-blind, sham-controlled, crossover study included 36 participants with Parkinson disease, with 17 randomly assigned to receive nVNS group and 19 to receive sham stimulation initially. A total of 21 patients completed both arms of the crossover study. The researchers looked at nVNS as an adjunct to standard of care for 1 month, focusing on the impact of treatment on freezing of gait. The researchers measured serum biomarkers of inflammation and oxidative stress as well as brain-derived neurotrophic factor .
The researchers found that velocity increased by 16% , step length increased by 11% and step time decreased by 16% in the active nVNS group. There were no significant changes in velocity , step length or step time in the sham group.
Clinical scores before and after treatment in the 2 groups separately showed improved clinical outcome measures in both groups. Unified Parkinsons Disease Rating Scale Parts II and III , falls efficacy scale score, and freezing of gait questionnaire scores all improved significantly in both groups.
Reference
You May Like: On Off Phenomenon
Vagus Nerve Stimulation For Parkinsons Disease
Vagus Nerve Stimulation has been shown to improve walking in patients with Parkinsons Disease.
What is Parkinsons Disease?
Parkinsons disease is a progressive, neurodegenerative disorder with no known cure. The majority of medical treatment is aimed at relieving the individual of symptoms rather than attempting to cure the disease. Many are often limited by debilitating symptoms that significantly reduce quality of life. Parkinsons symptoms include the following:
- A tremor
- Slowness and incoordination of movement
- Posture, balance and walking difficulties
- Poor executive function and memory loss
- Loss of smell
- Changes in writing and speech
- Weight loss
The Beginning of Parkinsons
Parkinsons disease actually begins outside of the brain, and travels through nerves, such as the vagus nerve, to enter the brain. Classically, Parkinsons is associated with the loss of the neurotransmitter dopamine due to the degeneration of an area of the brain called the substantia nigra . However, there is actually a decrease in norepinephrine before dopamine becomes depleted. There is degeneration in an area of the brain called the locus coeruleus before there is a problem with the substantia nigra.
Existing treatment strategies for Parkinsons disease are purely to relieve symptoms. However, the treatment is often accompanied by terrible side effects. New treatments are vital to developing more effective ways of treating Parkinsons.
Vagus Nerve Stimulation
Extensive Connections Between The Nts With Visceral Organs And Other Brain Structures
The NTS in the brainstem carries and receives visceral primary afferent signals from a variety of visceral regions and organs. Neurons that synapse in the NTS participate into the autonomic reflexes, with a result to regulate the autonomic function. Outputs that go from the NTS are transferred to a large number of other regions of the brain including the paraventricular nucleus of the hypothalamus and the central nucleus of the amygdala as well as to other nuclei in the brainstem . Perhaps, extensive connections between the NTS with visceral organs and other brain structures may elucidate the mechanism of auricular acupuncture.
Therefore, we proposed the auriculovagal afferent pathway both the autonomic and the central nervous system could be modified by auricular vagal stimulation via projections from the ABVN to the NTS .
Auriculovagal afferent pathway : both the autonomic and the central nervous system could be modified by auricular vagal stimulation via projections from the ABVN at the auricular concha to the NTS . NTS: nucleus of the solitary tract DMN: dorsal motor nucleus of the vagus AP: area postrema RVM: rostral ventrolateral medulla LC: locus coeruleus.
You May Like: What Kills A Person With Parkinsons Disease
Read Also: Voice Amplifiers For Parkinson’s
Relationship Between The Abvn And The Nucleus Of The Solitary Tract
The anatomical relationship between the ABVN and the nucleus of the solitary tract has been investigated. After applying horseradish peroxidase to the central cut end of the ABVN in the cat, some labeled neuronal terminals were seen in the interstitial, dorsal, dorsolateral, and commissural subnuclei of the NTS some of these terminals may be connected monosynaptically with solitary nucleus neurons which send their axons to visceromotor centers in the brainstem .
The auricular concha is mainly innervated by the ABVN. The relationship between the acupuncture stimulation at auricular concha and the NTS has also been investigated. In an animal study, acupuncture stimulation at auricular concha induced the hypoglycemic effect by activating the firing activities of the neurons in NTS . It is also found that acupuncture-like stimulation at auricular acupoint CO15 activates the cardiac-related neurons in the NTS to evoke cardiovascular inhibition, whereas the inactivation of the NTS with local anesthetics decreased the cardiovascular inhibitory responses evoked by auricular acupuncture .
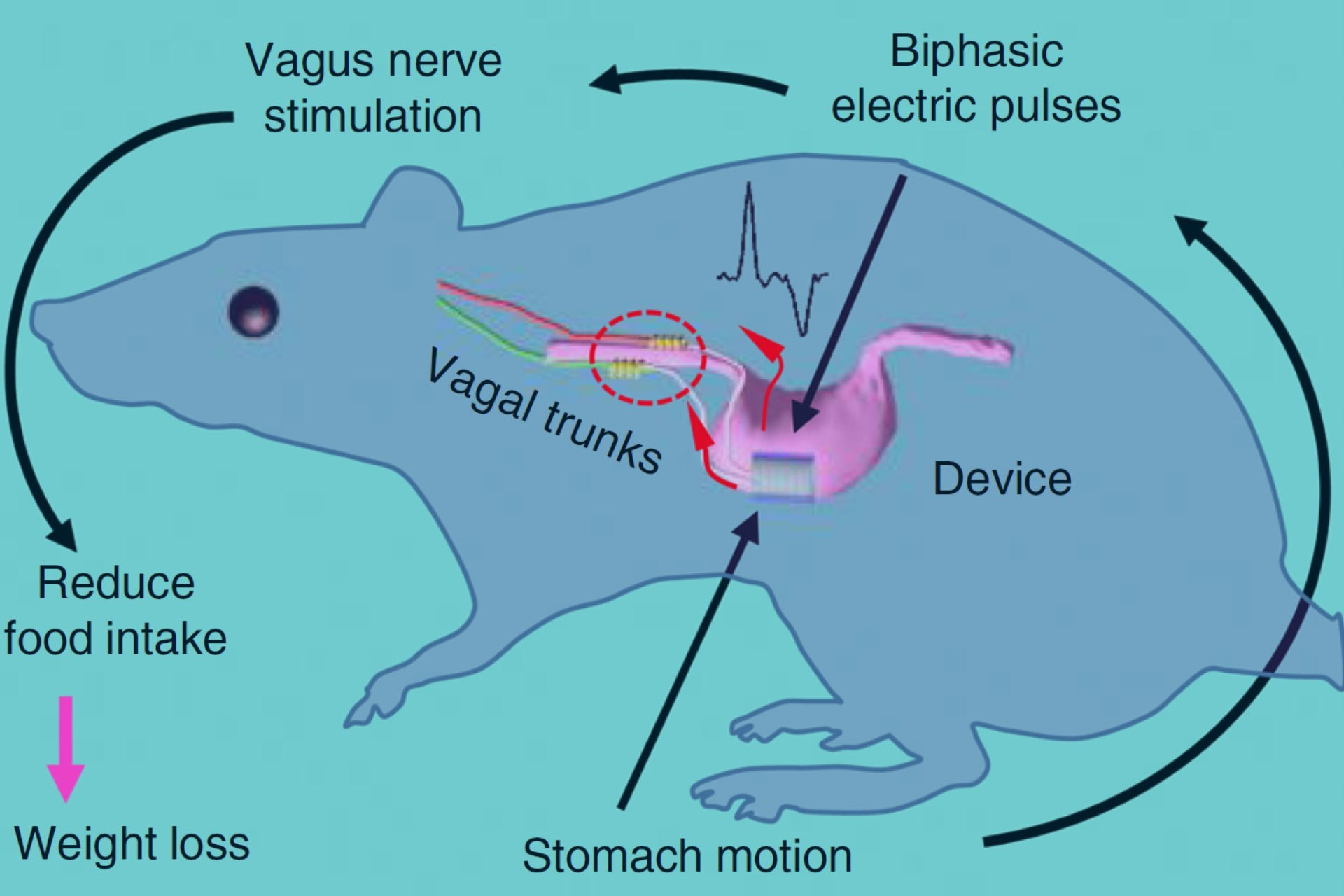
Vagus Nerve Stimulation Improves Locomotion And Neuronal Populations In A Model Of Parkinson’s Disease
VNS increases locomotor activity in a Parkinsons disease lesion model.
-
TH-positive neurons in the LC and SN are increased after vagus nerve stimulation.
-
VNS reduces -synuclein density within TH-positive neurons in the SN of this model.
-
Stimulation results in reduced astrocytes and microglial activation in lesioned rats.
Also Check: Yopd Life Expectancy
What Is The Importance Of Having An Animal Model
Prior to this animal model, we were limited to studying the motor features of Parkinsons disease: the slowness of movement, rigidity and tremor. We now have a model that exhibits almost all of the features of Parkinsons disease observed in humans, ranging from gastrointestinal dysfunction to motor dysfunction to anxiety and depression.
Evaluation Of Targeted Plasticity Therapy As A Treatment For Motor Dysfunction In Parkinsons Disease
Objective/Rationale:
Deterioration of motor function is a debilitating symptom of Parkinsons disease . We have recently developed a novel method that utilizes stimulation of the vagus nerve delivered during rehabilitative training to improve motor function after various types of brain injury. Vagus nerve stimulation enhances plasticity, or the ability to change, within neural circuitry that controls movement. We propose to evaluate whether VNS paired with rehabilitative training can improve motor function in pre-clinical models of PD.
Project Description:
Pre-clinical models will be trained to perform a behavioral task that measures forelimb movement speed. Once they are proficient at the task, each model will receive an injection of 6-OHDA to cause dopaminergic cell loss and impair function of the trained forelimb. Models will undergo implantation of a stimulating cuff around the vagus nerve and be separated into balanced groups. One group will undergo rehabilitative training alone. The second group will undergo identical rehabilitative training, but will also receive stimulation of the vagus nerve paired with training. A third group will undergo identical rehabilitative training, but will receive VNS two hours after the completion of training. For all groups, rehabilitative training will continue for six weeks. We will measure multiple parameters describing forelimb performance throughout the course of testing.
Relevance to Diagnosis/Treatment of Parkinsons Disease:
You May Like: On And Off Phenomenon
Improving Cognitive And Gait Control In Parkinsons With Vagus Nerve Stimulation
Although pharmacological intervention is the current gold standard treatment for many neurodegenerative and neuropsychiatric disorders, they carry many unwanted side effects.
Non-pharmacological alternatives such as electrical stimulation used mostly as an adjunct therapy has gained recent interest. Vagus nerve stimulation is a neuromodulation technique that impacts multiple neurotransmitter systems. VNS involves an invasive surgical implantation of a generator subcutaneously providing direct electrical stimulation of the cervical vagus nerve. VNS is currently an approved adjunct treatment for drug-resistant epilepsy and in patients with treatment-resistant depression. However, the effects VNS exerts may also be beneficial for other neurological disorders.
Recently, non-invasive VNS devices have been developed with the aim of stimulating the vagus nerve transcutaneously, significantly reducing the risk associated with the implantable device.
In this webinar, we will summarise the current literature on non-invasive VNS in Parkinsons disease and discuss preliminary findings of its therapeutic potential with an emphasis on its efficacy in improving cognitive and gait control in people with Parkinsons.
Watch this webinar, to discover:
Poor Eyesight Unfairly Mistaken For Brain Decline
Vagus nerve stimulation promotes resolution of inflammation by a mechanism that involves Alox15 and requires the 7nAChR subunit
Nonresolving inflammation underlies a range of chronic inflammatory diseases, and therapeutic acceleration of resolution of inflammation may improve outcomes.
Neural reflexes regulate the intensity of inflammation , but whether activation of the vagus nerve promotes the resolution of inflammation in vivo has been unknown.
To investigate this, mice were subjected to electrical vagus nerve stimulation or sham surgery at the cervical level followed by zymosan-induced peritonitis.
The duration of inflammation resolution was significantly reduced and efferocytosis was significantly increased in mice treated with VNS as compared with sham. Lipid mediator metabololipidomics revealed that mice treated with VNS had higher levels of specialized proresolving mediators , particularly from the omega-3 docosahexaenoic and docosapentaenoic metabolomes, in peritoneal exudates.
VNS also shifted the ratio between proinflammatory and proresolving LMs toward a proresolving profile, but this effect by VNS was inverted in mice deficient in 12/15-lipoxgenase , a key enzyme in this SPM biosynthesis.
The significant VNS-mediated reduction of neutrophil numbers in peritoneal exudates was absent in mice deficient in the cholinergic 7-nicotinic acetylcholine receptor subunit , an essential component of the inflammatory reflex.
Don’t Miss: Fitflop Shoes For Parkinson’s
Noninvasive Vagus Nerve Stimulation For Parkinson Disease Shows Safety Efficacy
Serum tumor necrosis factor and glutathione levels decreased, and brain-derived neurotrophic factor levels increased significantly after treatment with electroCores gammaCore nVNS device.
Results from a randomized, double-blind, sham-controlled crossover trial using electroCores noninvasive vagus nerve stimulation device showed significant improvements in patients with Parkinson disease on key gait parameters, including walking speed, stance time, and step length compared to sham treatment.1,2
A total of 36 patients with associated freezing of gait were recruited for the study, of whom 17 were randomized to nVNS and 19 to sham stimulation. In the active nVNS group, velocity increased by 16% , step length increased by 11% and step time decreased by 16% , whereas the changes in velocity , step length and step time were not significant in the sham group.
“We are pleased to have successfully completed the first randomized, double-blind sham-controlled trial to demonstrate the efficacy of cervical nVNS as an adjunctive therapy in PD, Lead investigator Hrishikesh Kumar, MD, MBBS, director, Research, and vice chairman, Institute of Neursciences Kolkata, said in a statement.1 Improvements in motor function and gait after 1 month of treatment with nVNS were significant. Our results clearly support additional work to further understand the potential for nVNS in this indication.
READ MORE: Increased Parkinson Disease Risk Associated With Nitrogen Dioxide Exposure
REFERENCES
Lack Of Oxygen To The Brain In Parkinson’s Disease
This mechanism also explains why medicated people with PD seem to “deflate” as a dose of drugs where off – our necks can visibly shorten, our heads move forward and down, our shoulders slump. On the other hand, some people with PD can get symptom relief by exaggerating the head position, and tucking their chin tightly against their chest, opening up the vertebrae at the back of the neck, as exampled in the following video of Michael J. Fox playing the guitar.
“Interventions can release imbalances in the tension of the small muscles that hold the skull and the first two vertebrae in relation to each other, and this repositions the atlas and the occiput. Improved alignment of the vertebrae, especially C1 and C2, improves blood flow to the brain and usually brings a rapid improvement in the function of the five nerves necessary for the state of social engagement.”
“If we can give the body the right information with a soft touch at the right place, the body will balance itself. Because we cannot put C1 and C2 into place and expect them to stay that way permanently, we should repeat balancing techniques frequently, or as needed. Since there is no such thing as a fixed state of balance, it is more useful to think of balancing, an ongoing process.”
You May Like: Sam Waterston Tremor