Lower Back Pain In People With Parkinsons
In a previous blog, we discussed pain and PD in general and highlighted different types of pain that a person with PD might experience.
PD contributes factors that can cause or worsen lower back pain, such as rigidity of the trunk muscles or dystonia of the trunk muscles. Both rigidity and dystonia can fluctuate with medication timing and correlate with ON and OFF time.
In addition, PD can be associated with central pain, which is poorly understood and thought to be due to abnormalities in the brain itself. Some new research suggests that PD can change how the brain feels pain that the loss of dopamine can make pain feel worse or make a person more likely to feel pain.
We know that:
- there is a higher prevalence of lower back pain in people with PD vs aged-matched controls
- certain features of PD such as increased age, depression, rigidity, and stooped posture are associated with lower back pain
- lower back pain can make it harder to deal with the challenges of PD because it is associated with lower activity levels. This can breed a vicious cycle in which lower back pain leads to decreased activity levels and then lower activity levels conspire to make the lower back pain worse
Radiological Examination And Analysis
Scoliosis was evaluated from an upright posteroanterior radiograph of the entire spine of each patient. If a patient was unable to stand upright for a whole-spine scanograph, a simple spine X-ray was performed. The degree, location, and direction of the scoliosis curve were assessed. Digital X-ray films and the Cobb method were used to measure the curve, and the degree of curvature was measured automatically with the aid of a digital X-ray viewing system . Using the findings, we divided patients into those with normal or spinal asymmetry , and those with scoliosis . All digital films were evaluated by a radiologist. Curve location was defined by its center, known as the apex, which is the most lateral disc or vertebra of the curve. The scoliosis cases were then subdivided according to the apical vertebra into cervical, thoracic, and lumbar cases. The direction of curvature was defined as direction of convexity.
Myopathy Associated Postural Deformity In Pd
Inflammatory myopathy of the paraspinal muscles can mimic the appearance of camptocormia in PD. Wunderlich et al.38 have described a 63-year-old man with PD in whom a camptocormia-like deformity developed. They noted hyperintensity within the paraspinal muscles and histopathological features consistent with myositis. The patient was treated with steroids and they noted marked improvement in forward flexion.
Myopathy with nemaline rods, end-stage myopathy with autophagic vacuoles, mitochondrial myopathy, and necrotizing myopathy have all been associated with camptocormia in patients with PD.15,25,30 Gydnia et al.15 have studied 19 consecutive muscle biopsies obtained in patients with PD and either camptocormia or dropped-head syndrome , finding abnormal muscle biopsies in all patients. Although MRI images were not abnormal in all patients, MR imaging generally showed fatty degeneration of the paravertebral musculature or neck extensor musculature in many of them. Electromyography was also generally consistent with myopathy changes.
You May Like: Does 23andme Test For Parkinson’s
Case : Bilateral Gpi Dbs
This patient was a 59-year-old man with PD and severe camptocormia. Parkinson disease was diagnosed based on the initial presenting symptoms of a severe stooped posture, decreased fine finger movements, and bilateral hand tremor. The patient’s camptocormia only minimally responded to dopaminergic medications, and he would fall several times a day. He had begun wearing kneepads to prevent further injury from his frequent falls. He underwent placement of bilateral GPi DBS electrodes to alleviate his parkinsonian symptoms as well as treat his camptocormia. He was discharged to an acute rehabilitation facility on postoperative Day 5 in good condition. At 15-month follow-up, while having some improvement in his parkinsonian symptoms, he continued to suffer from severe camptocormia.
Fasciculations Induced By Systemic Diseases Drugs And/or Intoxication By Heavy Metals
Thyroid disorders such as hyperthyroidism and inappropriate secretion of thyrotropin syndrome can also trigger fasciculations. Similarly, hypophosphatemia and calcium disorders secondary to hyperparathyroidism can sometimes cause the same. With regard to pharmacological treatments, in a pioneering experimental study Wigiton and Masland concluded that neostigmine may cause fasciculations potentials by increasing the concentration of acetylcholine in the neuromuscular junction in felines. Discharges are caused by the direct effect of acetylcholine on motor nerve terminals. Moreover, due to a similar mechanism, the same occurs during the induction of anesthesia with succinylcholine by endotracheal tube.
Finelli described an interesting case under the title of Drug-Induced Creutzfeldt-Jakob-like Syndrome. An elderly manifested rapidly progressive dementia, postural tremor, gait instability, myoclonus and fasciculations caused by a combination of lithium and nortriptyline. Postural tremor, multifocal myoclonus, amyotrophy and fasciculations were also reported in a woman treated with topiramate for migraine without aura. Orsini et al. also presented a case of fasciculations caused by oral corticosteroids at immunosuppressive doses in patients with immune-mediated kidney disease.
Don’t Miss: Joy Milne Parkinson’s Disease
What Causes Parkinson’s Disease
The precise cause of Parkinson’s disease isn’t clear. Genetic mutations can cause the condition, but these are rare. More often, genetic factors may increase your risk of developing Parkinson’s disease, sometimes in combination with significant exposure to toxins such as pesticides.
Men are more likely to develop Parkinson’s disease than women, and most cases develop around the age of 60 or older. However, younger people can develop Parkinson’s disease.
Parkinson’s disease is incurable, but the CarePoint Neurosurgery and Spine team offers some highly effective treatment options.
Treatments For Spinal Stenosis
Thankfully, spinal stenosis can often be treated, first with anti-inflammatories, physical therapy, and epidural steroid injections, which can decrease inflammation and pain. Minimally invasive surgery can also be performed in an outpatient procedure with a small incision and no stiches.
When its time to see a doctor for treatment for back pain that wont go away or is worsening, seek out a leader in minimally invasive procedures. Advances in minimally invasive treatments means treating chronic back pain is easier than ever. Between outpatient treatments and minimally invasive surgical procedures using small incisions, you can expect a quicker recovery time instead of a long hospital stay.
For more information, contact DISC Spine Institute, experts in minimally invasive treatments, the most effective medical procedures to treat and eliminate back pain.
Read Also: Gender Differences In Parkinson’s Disease
Operative Procedure & Postoperative Course
Considering the patient’s degree of deformity and pain, we elected to perform revision surgery. Pedicle screws and rods were reinserted from the L1to S1 levels with iliac screws after performing a partial pedicle subtraction osteotomy at the L4 level with removal of the intervertebral discs at the level of L34 . The patient’s intraoperative and postoperative periods were uneventful, and she was able to walk with a straight back without any support a few days postoperatively. Follow-up X-rays obtainedapproximately 18 months after surgery showed significant improvement in her spinal parameters and kyphoscoliosis. Pre and postoperative surgical outcomes were measured with Modified Scoliosis Research Society-23 Outcome Instrument scoring system . A mean postoperative score of 20 out of 25 indicated a satisfactory outcome.
Lateral thoracolumbar X-ray showing PPSO & discectomy performed at the L4 and L34 level, respectively, and lateral thoracolumbar X-ray showing the correction angle of approximately 30 degrees at the same level postoperatively. PPSO : partial pedicle subtraction osteotomy.Follow-up anteroposterior and lateral whole spine X-rays showing satisfactory correction of coronal and sagittal imbalance. *Indicates the lumbar lordosis, **Indicates sagittal vertical axis. PI : pelvic incidence, LL : lumbar lordosis, SVA : sagittal vertical axis.
Is Spinal Stenosis Causing Your Chronic Back Pain
Back pain is something that most people will encounter in their lifetimes. Almost 65 million people in the United States reported experiencing some form of back pain recently, and about 16 million adults have chronic back pain that interferes with their daily activities.
While back pain can be caused by a myriad of factors, one condition tends to afflict aging adults more than any other age groupspinal stenosis. The expert team at Cerebrum MD, led by board-certified neurosurgeon Dr. Joseph Watson, is here to help you understand what causes spinal stenosis and what treatment options are available.
Recommended Reading: Current Treatment For Parkinson’s Disease
Is There A Test For Spinal Stenosis
Doctors use a variety of tools to see if you have spinal stenosis and rule out other conditions, including:
- Medical and family history, which helps to determine if an injury, aging, or an underlying condition is causing your symptoms.
- Physical exam, which may check how you move and walk, when your pain happens, muscle strength in your arms and legs, and your balance.
- Imaging tests such as x-rays, MRI , and computerized tomography scans.
What Are The Symptoms Of Spinal Stenosis
Symptoms of spinal stenosis happen when the spaces within the spine narrow and put pressure on the spine. This occurs most often in the lower back and neck. For most people, symptoms develop slowly, and some people may not have any symptoms.
Symptoms of spinal stenosis in the lower back can include:
- Pain in the lower back.
- Burning pain or ache that spreads down the buttocks and into the legs, that typically worsens with standing or walking and gets better with leaning forward.
- Numbness, tingling, or cramping in the legs and feet. These may get worse when you stand or walk.
- Weakness in the legs and feet.
Symptoms of spinal stenosis in the neck may include:
- Neck pain.
- Numbness or tingling that spreads down the arms into the hands.
- Weakness in a hand, arm, or fingers.
Recommended Reading: Serotonin Syndrome And Parkinson’s
Bottom Line: Only Select Cases Appear To Benefit
This study is the first to characterize clinical and QOL outcomes following cervical decompression among patients with concomitant PD and CSM. Matched-pair analysis showed that patients with PD experienced diminished symptomatic and QOL improvement relative to controls.
Although decompression may have a role in alleviating pain-related disability in the PD population, this intervention appears to offer marginal benefit with respect to improving myelopathy and overall QOL. It is possible that only select patients with coexisting PD and CSM respond favorably to cervical decompression. Accordingly, preoperative pharmacologic optimization of PD should precede surgical correction of the spine. Further studies are needed to determine which patients with PD may benefit from surgical intervention for their myelopathy.
Mr. Xiao and Mr. Miller are medical students at Cleveland Clinic Lerner College of Medicine of Case Western Reserve University.
Dr. Krishnaney is a neurosurgeon in Cleveland Clinics Center for Spine Health and Department of Neurological Surgery.
Causes Of Lower Back Pain

People with PD may have the same lower back issues that affect the general population.
Here is a picture of the spine and its surrounding structures.
There are specific structural problems of the lower spine that can lead to pain. Primarily the structural problems fall into two categories:
- Narrowing of the central spinal canal through which the spinal cord travels. This can cause spinal stenosis and typically manifests as pain with standing or walking that improves with bending forward or sitting.
- Narrowing of the exit holes through which the spinal nerves travel. This can cause what is known as radiculopathy, pinched nerve, or sciatica and typically manifests as pain that travels down a leg.
There are many causes of these narrowings including:
Much less common, are infections of the spine or cancers growing around the spine. Both of these conditions can push on the spine or spinal nerves and cause pain.
Surprisingly, all of these causes together typically account for a small percentage of lower back pain. For most people with lower back pain, no specific structural cause can be identified.
Recommended Reading: Cleveland Clinic Parkinson’s Doctors
Points To Remember About Spinal Stenosis
- Spinal stenosis happens when the spaces in the spine narrow and create pressure on the spinal cord and nerve roots. The narrowing usually occurs over time.
- Depending on the location of the spinal stenosis, symptoms can include pain, numbness, and weakness in your legs, feet, arms, and hands.
- Treatments for spinal stenosis can include nonsurgical treatments such as physical therapy, medications to help manage pain, and, in some cases, surgery.
- To help you live with spinal stenosis, get regular exercise, change activities in your routine that cause pain, maintain a healthy weight, and dont smoke.
A Dilemma Of Symptom Overlap
Patients with Parkinsons disease may exhibit symptoms similar to those observed in cervical spondylotic myelopathy , including ataxia, weakness, and bowel or bladder dysfunction. These similarities present diagnostic and therapeutic challenges when PD and CSM coexist. While CSM is typically treated with surgical decompression , PD requires pharmacologic therapies and is expected to derive little benefit from decompression. This poses a dilemma for both neurologists and spine surgeons treating patients with PD who may have evidence of cervical spondylosis and myelopathy.
Clinical and quality-of-life outcomes following cervical decompression in the PD population remain undefined. Defining these outcomes may improve patient management and help avoid unnecessary surgical intervention. To that end, Cleveland Clinic Center for Spine Health clinicians and researchers recently sought to investigate clinical and QOL outcomes following cervical decompression among patients with CSM with and without coexisting PD. We hypothesized that both groups would benefit from surgery but that patients with concomitant PD would experience inferior outcomes.
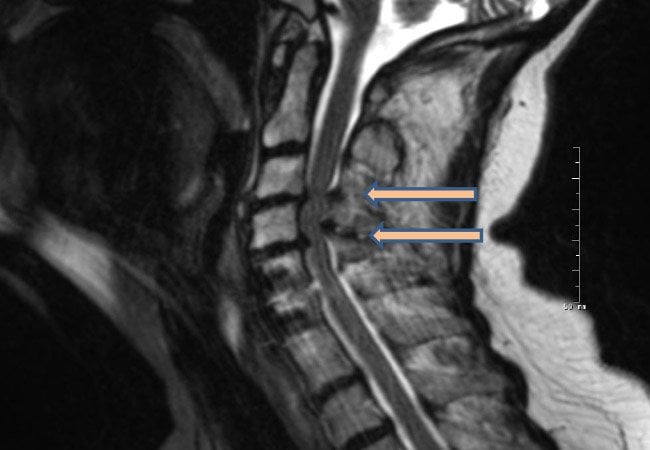
Figure. Preoperative sagittal T2 MRI of a patient with coexistent cervical spondylotic myelopathy and Parkinson disease. Note the severe cervical stenosis and cord compression at C3-4and C4-5 . Postoperative X-ray after the patient underwent laminectomies at C3 through C5 and extension of her fusion to C3 via a dorsal approach.
Read Also: Is Thumb Twitching A Sign Of Parkinson’s
Results: Pd Attenuates Clinical And Qol Improvements
Fifty-five patients met the studys inclusion criteria: 11 with both PD and CSM and 44 with CSM alone.
We found that symptoms improved postoperatively in both cohorts however, back pain, radiculopathy, and bowel/bladder dysfunction persisted among patients with PD relative to those without PD. Moreover, patients with PD experienced poorer improvement on both the Nurick and mJOA scales. PD was identified as a significant independent predictor of decreased improvement in patients functional status.
In the QOL analysis, while the control cohort experienced improvement across all measures examined, PD patients improved in only one . Despite an absence of significant differences between the cohorts in preoperative QOL, patients with PD had poorer QOL at last postoperative follow-up as measured by the EQ-5D and PDQ , and a smaller proportion of PD patients achieved the prespecified minimal clinically important difference in EQ-5D . No between-cohort differences in achieving a minimal clinically important difference were observed for the PDQ or PHQ-9.
Multivariable regression identified PD as a significant independent predictor of poorer improvement in EQ-5D and of failure to achieve a minimal clinically important difference in EQ-5D . Results of this QOL analysis were recently published in The Spine Journal.
Evaluating Lower Back Pain
When a person develops lower back pain, a neurological history and exam can help rule out serious medical conditions that may need further evaluation and intervention. The neurological history will collect information about other neurological symptoms such as numbness, tingling, weakness, new bowel or bladder symptoms, etc. The neurologic exam will assess strength, sensory changes and reflexes, among other things, which can shed light on spine function and help determine if a serious medical condition is present. Lower back pain caused by a serious medical condition is rare . Nevertheless, be sure to tell your neurologist about any new symptoms that you may have.
For most people, neurologic history and exam will confirm that lower back pain can be managed conservatively. When this is the case, treatment of the pain with exercise and physical therapy is the best course forward. Your neurologist may determine that imaging of the lower back will be helpful. If that is the case, he/she may order an MRI of the lower spine. An MRI will show structural changes to the lower spine but will not visualize PD-specific causes of lower back pain such as rigidity, dystonia, or central pain.
Studies have shown that MRIs can reveal structural changes that do not result in pain at all. So, it is important not to let imaging be the sole guidance of lower back pain management.
You May Like: How Long Do Parkinson’s Patients Live After Diagnosis
Biography Of Charles J Malemud
Charles J. Malemud received the Ph.D. from George Washington University in 1973 and completed postdoctoral studies at the State University of New York at Stony Brook in 1977. Since 1977, Dr. Malemud has been a member of the faculty at Case Western Reserve University School of Medicine where he is presently Professor of Medicine & Anatomy in the Division of Rheumatic Diseases and Senior Investigator of the Arthritis Research Group. He has published over 230 papers, chapters and reviews primarily in the field of chondrocyte biology. Professor Malemud is on the editorial board of several rheumatology, immunology and musculoskeletal journals and is Editor-in-Chief of the Journal of Clinical and Cellular Immunology and Global Vaccines and Immunology.
What Causes Spinal Stenosis
Spinal stenosis can be both an inherited condition, like achondroplasia, a defective bone formation that narrows the spinal canal, said the National Institute of Arthritis and Musculoskeletal and Skin Diseases . It can also be acquired as the result of a condition like scoliosis, in which the curvature of the spine affects the surrounding nerves, tissue, and ligaments. Or, it can be the result of a degenerative condition. Everything from bone spurs to bulging discs to spondylolisthesis to osteoarthritis can cause the spinal cord to narrow.
This reinforces the importance of seeing a doctor for back pain. Its obviously important to continue treatment from a leading back doctor if you were born with a condition that needs to be controlled, both for pain management and so it wont worsen and turn into spinal stenosis. But, going to the doctor for back pain is not something everyone does at the first sign of symptoms knowing how dangerous conditions like spinal stenosis can be should help convince back pain sufferers to allow a professional to do a thorough examination and develop a plan to treat the issue so it does not degenerate.
Don’t Miss: Is Drooling A Sign Of Parkinson’s