Clinical Implications Of Rbd And Its Relationship To Dlb
RBD can be either idiopathic and a marker of prodromal neurodegeneration or secondary to neurodegeneration . Longitudinal studies of idiopathic RBD had shown evidence of a strong association with eventual phenoconversion to a neurodegenerative disease. Phenoconversion risk between two and five years is about 15% to 35%, and the risk may increase to 41% to 90.9% if extending the follow-up period up to 12 to 25 years. When patients have RBD, compared to those without RBD, the accompanied neurodegenerative disease tends to be worse, such as more severe parkinsonian symptoms, autonomic dysfunction, and cognitive impairment .
Overall, idiopathic RBD patients convert to PD eventually and accomplish with 5 years. Those PD patients converted from RBD were faster motor progression, less response to levodopa therapy, and more severe postural instability . RBD appears to be associated with the -synucleinopathies . Previous studies showed that 38%65% of RBD patients have developed -synucleinopathy from 10 to 20 years after RBD presentation it could be most likely PD, DLB, or multiple system atrophy . Other cohort studies have provided evidence that patients with idiopathic RBD will eventually develop a synucleinopathy, such as PD, DLB, or MSA .
How Your Support Made This Research Project Possible
This award means that I can focus solely on my research rather than searching for funding, but most importantly to me, it shows there is support for the direction of my research and shows others that it has potential, Krohn says. With this support, it is easier to continue to fund the work and move it forward so we can reach our ultimate goals.
Krohn thanks donors for their support of Parkinson Canadas research.
Every step in neurodegenerative disease research, no matter how basic or advanced it may seem, is a step toward improving the lives of patients, she says. Every last bit of support helps to reach the point where our research translates into applicable treatments.”
Rbd Patients Who Develop Parkinsons: The Next Steps
According to the Neurology Advisor, about 60% of Parkinsons disease patients currently also suffer from RBD, and the Neurology Advisor also notes that many Parkinsons patients diagnosed with RBD experience a much faster deterioration of motor and cognitive functions. While these statistics and information may sound extremely daunting and hopeless, there is still hope for you or your loved one to live as normal life as you can before symptoms progress into the later stage. Avoiding triggers such as caffeine and alcohol can tremendously help reduce RBD incidents. Creating a safe household with minimal clutter or sharp objects can also reduce the risk of violent or dangerous accidents.
If screened early, Parkinsons disease patients who develop RBD, or vice versa, can participate in up and coming clinical trials that may provide greater relief as well. In some instances, medical cannabis has also shown to relieve Parkinsons-related sleep incidents and other symptoms. While neither of these illnesses are diagnosable, studies have shown that particular strains of cannabis have the potential to relax muscles during sleep and help patients who suffer from violent and terrifying nightmares.
Read Also: Parkinson’s Disease Mouse Model
Diagnoses And Treatment Of Rbd
The diagnosis of RBD is based on clinical features and polysomnography findings. Firstly, the patients must have repeated episodes of complex motor behaviors or vocalization during REM sleep, and they can be documented by PSG or reports of dream enactment. Secondly, it must have evidence of REM sleep without atonia on PSG, namely, REM sleep without atonia . Other clinical findings are strongly suggested by the diagnosis of RBD, but RSWA is not observed, yet the diagnosis can still be given. RBD can be secondary to several medications, most of which are antidepressants . When RBD is believed as a secondary cause of medication use, a diagnosis of RBD is still applicable.
Rem Behavior Disorder As An Early Marker For Development Of Neurodegenerative Diseases
Umesh Vyas and Rose Franco
Download PDF |
| Abstract
REM behavior disorder is a parasomnia characterized by emergence of purposeful complex motor activity with an enactment of dream related activities. This condition is associated with vivid often violent dreams. In normal adults during REM, diffuse hypotonia of muscles occur and on polysomnography the limb and chin electromyographic channels demonstrate a low voltage or even flat signal. In RBD, the EMG demonstrating intermittent loss of electromyographic atoniais one of the criteria for diagnosis. Diagnostic polysomnographyrequire capturing the complex dream behaviors on video and electroencephalography monitoring confirms that the behavior originated out of REM sleep. RBD can be either idiopathic or symptomatic of various underlying conditions and may in fact be a prodromal symptom of neurodegenerative disease. It can present acutely which is almost always induced by medications or develop gradually over months to years. More than half of those with RBD will eventually exhibit signs and symptoms of a degenerative neurologic disorder. A Polysomnogram is necessary to diagnose RBD, showing absence of REM sleep atonia and related abnormal behavior. Keywords: REM sleep REM Behavior Disorder Neurodegenerative diseases Parkinsons disease Polysomnogram |
Introduction
Parasomnias are undesirable, unexpected, abnormal behavioral phenomena that occur during sleep. There are three broad categories in parasomnias. They are
Figure 1
Recommended Reading: Possible Causes Of Parkinson’s Disease
Tips For Better Sleep
- Keep a regular sleep schedule go to bed at the same time and get up at the same time.
- Choose your bedtime based on when you want to get up. Plan to spend seven to eight hours a night in bed.
- Make a bedtime routine for example, snack, bath, tooth-brushing, toileting and follow it every evening.
- Spend time outdoors and exercise every day, in the morning if possible. Avoid exercise after 8:00 p.m.
- If you cant get outdoors, consider light therapy sitting or working near a light therapy box, available at drug stores and department stores.
- If you nap, try to do so at the same time every day, for no more than an hour, and not after 3:00 p.m.
- Sleep in a cool dark place and use the bed only for sleeping and sexual activity.
- Do not read or watch television in bed.
- Use satin sheets and pajamas to make moving in bed easier.
- Minimize drinking liquids for three hours before bedtime to avoid frequent nighttime urination.
- Go to the bathroom immediately before retiring.
- Place a commode next to the bed, to minimize the effort, and light to get up during the night.
- Avoid:
- Alcohol, caffeine and other stimulants such as nicotine
- Heavy late-night meals
- Heavy exercise within six hours of bedtime
- Thoughts or discussions before bedtime about topics that cause anxiety, anger or frustration
- Clock watching
- Screen time television, phones, tablets one or two hours before bed.
Rbd And Neurodegenerative Disorders
Up to 60% of Parkinsons disease patients have RBD, as do 80 to 100% of patients with dementia with Lewy bodies and multisystem atrophy.
What these diseases all have in common is that they are synucleinopathies, and they have pathology that involves specific subcortical and brainstem areas, including those involved in the regulation of atonia during REM sleep, said Walter.
A prospective cohort study published in the August 2015 issue of JAMA Neurology found that RBD may be a marker indicating more aggressive progression of PD.1 The authors concluded with a recommendation that patients with PD be screened for RBD at baseline visits, as it identifies a diffuse/malignant subgroup of patients with PD for whom the most rapid progression rate could be expected.1
Additionally, idiopathic RBS is thought to be a precursor to neurodegenerative disease due to a synucleinopathy, said Liza H. Ashbrook, MD, a clinical fellow at the Stanford Sleep Medicine Center, who has a background in neurology and is now focusing on treatment of sleep disorders. Increasing data shows that the majority of patients with idiopathic RBS will develop a neurodegenerative synucleinopathy, whether it is three or 20 years between the diagnoses.
You May Like: Acupressure Points For Parkinson’s Tremors
What Is Rem Sleep Behavior Disorder
It may seem like sleepwalking, but RBD is, by definition, not a sleepwalking disorder. RBD involves dream enactment behavior.
The difference between sleepwalking and RBD is subtle, but important: sleepwalking typically takes place in non-REM and transitional stages of sleep, whereas RBD takes place during REM sleep.
Rem Sleep Behavior Disorder
The first major classification of sleep disorders, the Diagnostic Classification of Sleep and Arousal Disorders, was published in 1979 . In 2014, the International Classification of Sleep Disorders made the 3rd revised version of the American Academy of Sleep Medicine’s manual of sleep disorders nosology . A parasomnia involves undesired events that happen during sleeping. It also involves three different classifications: nonrapid eye movement- related parasomnias, REM-related parasomnias, and other parasomnias. RBD is one of the REM-related parasomnias.
Read Also: Can Vyvanse Cause Parkinson’s
Dream Enactment In Rem Sleep
RBD is different. It only occurs during REM sleep. One remarkable phenomenon that occurs in REM sleep is the bodys natural paralysis from the chin down . During REM sleep, one should not be able to move any muscles. Dream enactment behavior, then, implies a major neurological disconnect between the brain and body during sleep.
Also intriguing – people with RBD can be very much aware of their dream content as they act it out. They may describe it as being awake and asleep simultaneously. Unlike sleepwalkers, once awakened, people with RBD can recall vivid details of their dreams.
Unfortunately, RBD can be aggressive, violent and nightmarish, leading to injuries to both the sleeper and anyone else nearby. It can even lead to property damage.
You may recall that actor Alan Alda recently shared his PD diagnosis. The problem which inspired his journey to diagnosis was dream enactment behavior, which he said preceded other PD motor symptoms like tremor.
Comic Mike Birbiglias autobiographical film, Sleepwalk With Me, recounts his RBD onset, which occurred during his first comedy tour. He was inspired to tell his story after bursting through a second-story hotel window while acting out a dream.
Melatonin For Rapid Eye Movement Sleep Behavior Disorder In Parkinson’s Disease: A Randomised Controlled Trial
Woolcock Institute of Medical Research, The University of Sydney, Sydney, Australia
ForeFront Parkinson’s Disease Research Clinic, Brain and Mind Centre, The University of Sydney, Sydney, Australia
Research Group for Neurorehabilitation , Department of Rehabilitation Sciences, KU Leuven, Leuven, Belgium
Woolcock Institute of Medical Research, The University of Sydney, Sydney, Australia
Department of Neurology, University Hospitals of Geneva, Switzerland
Woolcock Institute of Medical Research, The University of Sydney, Sydney, Australia
Department of Respiratory and Sleep Medicine, Royal Prince Alfred Hospital, Sydney, Australia
Woolcock Institute of Medical Research, The University of Sydney, Sydney, Australia
Department of Respiratory and Sleep Medicine, Royal Prince Alfred Hospital, Sydney, Australia
Woolcock Institute of Medical Research, The University of Sydney, Sydney, Australia
Department of Respiratory and Sleep Medicine, Royal Prince Alfred Hospital, Sydney, Australia
Woolcock Institute of Medical Research, The University of Sydney, Sydney, Australia
ForeFront Parkinson’s Disease Research Clinic, Brain and Mind Centre, The University of Sydney, Sydney, Australia
Correspondence to:
Woolcock Institute of Medical Research, The University of Sydney, Sydney, Australia
ForeFront Parkinson’s Disease Research Clinic, Brain and Mind Centre, The University of Sydney, Sydney, Australia
Woolcock Institute of Medical Research, The University of Sydney, Sydney, Australia
You May Like: Michael J Fox Parkinson’s Research
Diagnosing And Treating Rbd
If you suspect that you or a loved one might have RBD, a movement disorder neurologist or a sleep physician should conduct an evaluation. The specialist might order a sleep study that would spot abnormal muscle movements during REM sleep. Hallucinations or waking up during a certain stage of sleep is different from REM sleep behavior disorder and might indicate a different condition.
If a diagnosis is confirmed, we recommend the following safety precautions:
-
Lower the bed if possible to prevent falls.
-
Pad the side rails if youre sleeping in a hospital bed.
-
Pad the floor around the bed.
-
Move nightstands away from the bed.
-
Move the bed away from walls or windows.
-
Sleep in separate beds or rooms if necessary .
-
Use a sleeping bag with a zipper to restrict arm and leg movements.
Dreams And Parkinsons Disease
Nine in 10 people living with Parkinsons disease experience sleep disturbances, ranging from vivid dreams and nightmares to insomnia and daytime napping. Some of these problems can be alleviated through good sleep hygiene procedures, such as improving sleeping environment, maintaining a healthy diet and keeping a routine. Make sure to discuss these symptoms with a healthcare professional.
Visit the EPDAs Sleep Well campaign to find out more about sleep disturbance and Parkinsons disease.
Read more:
Read Also: Parkinson’s Disease Related Disorders
Rem Sleep Behavior Disorder A Predictor Of Lewy Body Dementia
REM sleep behavior disorder has also been linked toLewy body dementia, another neurological disorder, as an early predictor of the disease. Lewy body dementia is a form of dementia with the presence of Lewy bodies in the brain.
Researchers investigated 136 patients diagnosed with Lewy body dementia or Parkinsons disease with dementia between 2004 and 2014. A total of 107 of those patients had a diagnosis of Lewy body dementia. Of those participants, the prevalence of REM sleep behavior disorder increased from the initial visit to the memory clinic alongside other core symptoms associated with Lewy body dementia. The researchers concluded that the prevalence of RBD in those with Lewy body dementia becomes greater as symptoms worsen over time.
Why Are Some Dreams Particularly Vivid Or Negative For People With Parkinsons
REM sleep plays a pivotal role in processing emotional events, and several studies have shown that the consolidation of emotional memories occurs in this sleep stage. Vivid dreams tend to be more frequent when awakening from REM sleep, the stage disrupted by Parkinsons. Some drugs used to treat Parkinsons can also accentuate dream vividness.
Many people with the condition describe the content of their dreams as negative. The vividness and emotional description of dream reports correlate with the limbic system an area of the brain associated with our emotional life. Although the reasons why people with Parkinsons often experience negative dreams have not been fully explained, this is likely due to damage in a particular area of the brain.
Dr Daniele Urso.
You May Like: Best Time To Take Parkinson’s Medication
Men Who Sleepwalk Have Greater Risk Of Parkinsons
Previous research also has suggested that RBD is associated with a higher burden of non-motor symptoms, as well as more severe motor disease, but whether its presence in early Parkinsons influences the progression rate of other symptoms remains largely unclear, the researchers added.
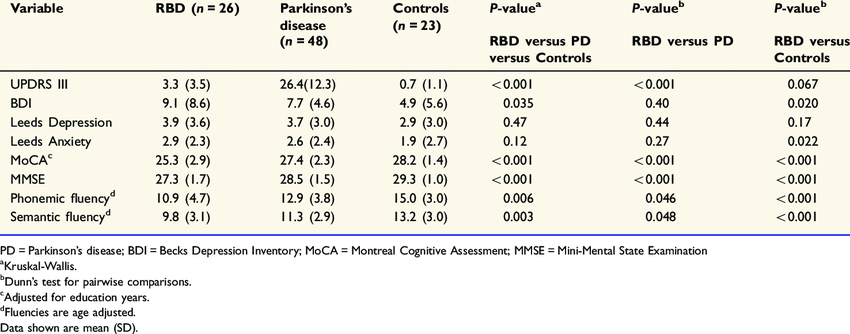
To address this, a team of researchers at the University of Oxford, in the U.K., evaluated RBDs impact on the progression of motor and non-motor symptoms over time in 923 people with early Parkinsons.
Patients had been diagnosed within the past 3.5 years, and were recruited from 2010 to 2019 to join the Oxford Parkinsons Disease Centre Discovery cohort, an ongoing study of early Parkinsons involving 11 hospitals.
Participants demographic and clinical features, including motor and non-motor symptoms, were assessed every 18 months through standard questionnaires and measures. Given that RBDs rates were shown previously to increase over time among Parkinsons patients, its potential presence was determined over time, based on RBD Screening Questionnaire scores.
Patients mean age was 67.1 years, and most were men , married , and white . A total of 788 participants completed at least one follow-up visit with a mean of 4.8 years of follow-up and up to 8.3 years and 153 completed all visits.
Reasons for limited follow-up data included severe illness that prevented such assessments, study withdrawal or loss to follow-up, and death.
Rem Sleep Behavior Disorder With Parkinsons Disease Can Be A Nightmare
Acting out dreams could indicate REM sleep behavior disorder. What you should know about the symptoms, diagnosis and treatment.
Certain sleep disorders are common in people with Parkinsons disease.
MORE FROM MICHIGAN: Sign up for our weekly newsletter
One of them REM sleep behavior disorder is a condition characterized by the acting out of dreams that are vivid, intense and violent. People have been known to yell or talk while asleep, carry on conversations or hit themselves or their bed partner. Even if physical damage does not occur, the condition can be frightening for the bed partner to witness.
REM behavior disorder does not necessarily disrupt the quality or quantity of sleep itself. But it is potentially harmful because of the physical movements involved.
You May Like: Best Walking Cane For Parkinson’s
Rem Sleep Behavior Disorder Risk Factors
Risk factors associated with an increased likelihood of developing REM sleep behavior disorder include:
- Being a male over the age of 50. Women, on the other hand, are seeing more diagnosis of RBD when they are under the age of 50
- Having a neurological disorder like Parkinsons disease or Lewy body dementia
- Having a chronic sleep disorder
- Taking certain medications like antidepressants
- Withdrawal from drugs or alcohol
Clinical Implication Of Rem Sleep Behavior Disorder In Parkinson’s Disease
Issue title: Mental Dysfunction in Parkinson’s Disease
Article type: Review Article
Authors: Kim, Young Eun | Jeon, Beom S.
Affiliations: Department of Neurology, Hallym University Sacred Heart Hospital, Hallym University College of Medicine, Anyang, Korea | Department of Neurology, Seoul National University Hospital, Seoul National University College of Medicine, Seoul, Korea
Note: Correspondence to: Beom S. Jeon, MD, PhD, Department of Neurology, Seoul National University Hospital, 101 Daehak-ro, Jongno-gu, Seoul 110-744, Korea. Tel.: +82 2 2072 2876 Fax: +82 2 3672 7553 E-mail:
Keywords: REM sleep behavior disorder, Parkinson’s disease
DOI: 10.3233/JPD-130293
Journal: Journal of Parkinson’s Disease, vol. 4, no. 2, pp. 237-244, 2014
Don’t Miss: How Does Parkinson’s Disease Kill You