Supine Hypertension As A Treatment Consideration In Parkinsondisease
Because supine hypertension is another manifestation of thecardiovascular autonomic dysfunction that also causes nOH, it can occur inpatients with nOH regardless of treatment. To complicate matters, the treatmentsthat raise orthostatic BP may also increase BP when supine . Asdescribed in the preceding text, the risk of supine hypertension associated withindividual pressor agents used in the treatment of nOH may vary. In addition tothe appropriate selection of nOH treatment based on the supine hypertension riskprofile, 24-h ambulatory BP monitoring can provide the patient and clinicianwith information on when and under what circumstances the patient experiencesnOH symptoms and supine hypertension, and this information should be consideredwhen initiating or adjusting nOH pharmacotherapy .
Given that both nOH and supine hypertension pose risks to patientsafety, balanced management of the two conditions is often required. Todetermine the best treatment approach for the individual patient, healthcareproviders should consider factors such as comorbidities, concomitantmedications, and prognosis, as well as discuss the benefits and short- andlong-term risks with each patient .
The Effect Of The Anti
One of the initial steps required when assessing a patient who is going to receive any anti-parkinsonian medication/treatment or who needs a dose adjustment is to anticipate the potential effect on his blood pressure, as it is one of the commonly related factors to the appearance of OH .
Several actions could help to improve the detection of this complication, either by the physician or the subject. It seems reasonable to instruct the patient about OH symptoms , although many cases go unnoticed . An initial pressor response assessment could be valuable to have a simple measurement to monitor future changes, as this measurement is one of the easiest ways to appraise OH in various healthcare settings.
Many caveats should be considered prior to establishing the real influence of PD medications on OH. First, there are different diagnostic criteria for defining OH. Additionally, much evidence is based on cross-sectional analyses and other confounding effects, as disease duration or previous autonomous nervous system damage , have not always been considered.
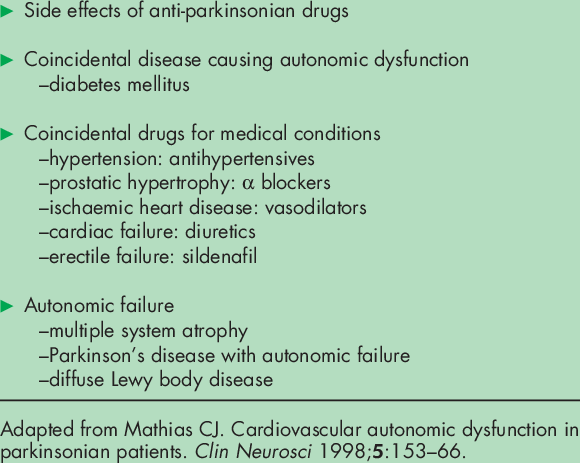
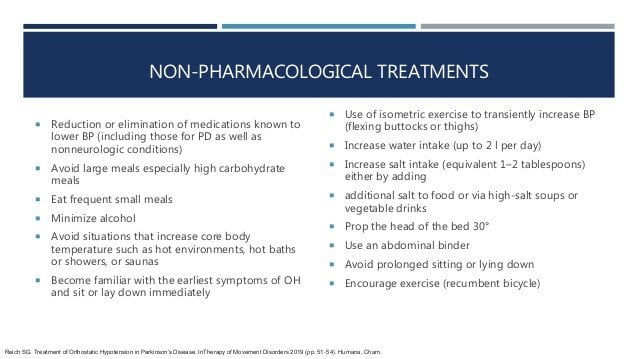
We present the current evidence to estimate the potential role of current PD treatments on OH. The influence of other drugs, such as antidepressants, diuretics, and antihypertensives, is not reviewed here. Nevertheless, they should be considered when dealing with this complication and decreasing the dose or stopping the responsible medication might be advisable.
First Step: Make The Right Diagnosis
Given its unspecific, and sometimes asymptomatic, presentation, OH should be actively screened at bedside by measuring the BP and heart rate supine and after 3 minutes upon standing . OH is diagnosed in case of a systolic BP fall 20mmHg and/or diastolic 10mmHg with respect to baseline . Standing systolic BP values < 90mmHg are also highly suggestive of OH and often predict symptoms of orthostatic intolerance . In case of milder BP falls at the 3rd minute upon standing, it is recommendable to prolong the orthostatic challenge to 510 minutes, in order to screen for delayed OH, a possible precursor of classic OH .
Once a diagnosis of OH is established, non-neurogenic causes and exacerbating factors, such as dehydration, anemia or infections should be ruled out. The medication schedule should be also reviewed for drugs with BP lowering effect, which may have been recently introduced or increased in dose: not only anti-hypertensive agents, but also dopaminergic drugs, tricyclics, opioids, neuroleptics or -blockers.
Fig.1
Management of orthostatic hypotension and supine hypertension in Parkinsons disease. OH, orthostatic hypotension BP, blood pressure HR, heart rate NSAIDs, non-steroidal anti-inflammatory drugs SNRI, serotonin-noradrenaline reuptake inhibitors. Adapted from Fanciulli et al. 2014 and Fanciulli et al., 2016 with permission from Springer and John Wiley and Sons.
Fig.2
Template of a home blood pressure diary for patients with orthostatic hypotension.
Also Check: Does Sam Waterston Have Parkinsons
Clinical Evaluation Of Noh
Routine clinical evaluation of patients with PD should always include an assessment of blood pressure . Although orthostatic hypotension is diagnosed with a reduction of s-SBP of at least 20 mmHg within 3 minutes of standing, lesser drops in s-SBP may still be symptomatic, and orthostatic hypotension may not occur until beyond 3 minutes. Heart rate should normally rise 46 beats per minute upon standing, with a greater increase in response to orthostatic hypotension with autonomic dysfunction, this cardioacceleratory response is typically blunted. Symptomatic nOH may not always correlate with isolated measurements of s-SBP, due to the diurnal circadian rhythm of blood pressure and also to the marked fluctuations in blood pressure that occur throughout the day. Twenty-four hour ambulatory blood pressure monitoring can be helpful in the evaluation of patients with symptomatic nOH to better understand temporal fluctuations in blood pressure, especially when clinical symptoms do not regularly correlate with sporadic blood pressure measurements.
Blood Pressure And Parkinsons: Whats The Connection
This 60-minute audio with slides is an interview of two neurologists and a person with Parkinsons discussing the symptoms, causes, and how to mitigate episodes of low blood pressure, as well as high blood pressure and recent Phase III trial testing of the high blood pressure medication, isradipine, to slow Parkinsons disease progression without lowering blood pressure too much.
Also Check: Yopd Life Expectancy
How Is Noh Diagnosed
Diagnosis of nOH requires blood pressure readings taken while lying flat as well as while standing up. At least a 20 mmHg drop in your systolic blood pressure and a 10 mmHg drop in your diastolic blood pressure when you stand up is required to make the diagnosis.
Some people with Parkinsons dont experience a drop in blood pressure every time they stand up. In these cases, a doctor may use a monitor to measure the persons blood pressure every 30 minutes for an entire day to assist in diagnosis and subsequent management of nOH.
Learn more about managing nOH in the second part of this article.
To learn more about the impact of nOH on people with Parkinsons and their care partners, read results from the Harris Poll Survey here.
Low Blood Pressure And Pd
Neurogenic orthostatic hypotension is a sharp drop in blood pressure that happens when a person gets up from bed or from a chair, causing dizziness or even loss of consciousness. Doctors define it as a blood pressure drop of 20 millimeters of mercury in systolic blood pressure , or a drop of 10 millimeters in diastolic blood pressure , within three minutes after standing up. The condition can put people with Parkinsons at risk of fainting, losing balance, falling and being injured. What can you do? Learn strategies to predict when blood pressure is most likely to fall and also take steps to avoid feeling dizzy in the first place.
Don’t Miss: On Off Phenomenon
Whats Hot In Pd If You Are Dizzy Or Passing Out It Could Be Your Parkinsons Disease Or Parkinsons Disease Medications
This 3-page article, with references, is a personal statement by Dr. Okun describing the mis-diagnoses Parkinsons patients can be given when visiting the ER for symptoms of dizziness or syncope outlining what defines a proper diagnosis of orthostatic hypotension, its frequency in people with Parkinsons, medication and lifestyle changes that can help.
Is There Any Treatment
There is no cure for multiple system atrophy with orthostatic hypotension. Treatment is aimed at controlling symptoms. Anti-Parkinson medication such as Sinemet may improve the general sense of well-being. Medications to elevate blood pressure while standing are often used, but may cause high blood pressure when lying down. Individuals should sleep with the head of the bed elevated. An artificial feeding tube or breathing tube may be required for problems with swallowing and breathing.
Also Check: Judy Woodruff Parkinson’s
Stay Informed On Your Parkinsons Journey
Would you like to learn more about nOH and living well with Parkinsons?
Our Every Victory Counts® manual gives people living with Parkinsons, their care partners and their family members the tools they need to take control of their own Parkinsons treatment through a proactive approach to self-care.
a powerful new print edition
Its jam-packed with up-to-date information about everything Parkinsons, plus an expanded worksheets and resources section to help you put what youve learned into action. Color coding and engaging graphics help guide you through the written material and point you to complementary videos, podcasts and other materials on the Every Victory Counts companion website. And, it is still free of charge thanks to the generosity of our sponsors.
Request your copy of the new Every Victory Counts manual by clicking the button below.
Dr. Jose-Alberto Palma is Assistant Professor of Neurology and Assistant Director of the Dysautonomia Center at New York University. His work over the past years has been focused on the diagnosis, management and understanding on autonomic disorders in patients with autonomic synucleinopathies, such as Parkinson disease and multiple system atrophy, as well as in the search for biomarkers for early diagnosis of these disorders. He has been involved in several studies and clinical trials to develop new treatments for autonomic dysfunction, and to describe the premotor phase of Parkinson disease.
Low Blood Pressure In Parkinson’s Disease
This 2-page article discusses the frequency of orthostatic hypotension in those with PD, the cause, symptoms and several simple measures that can be used to restore normal blood pressure regulation, including medication evaluation, increase of fluids and salty foods, caffeine, frequent small meals, environment, clothing, slow position change, bed position and medication options.
Don’t Miss: Parkinson’s Bike Therapy
What Is Neurogenic Orthostatic Hypotension
OH is a sustained fall in blood pressure that happens within 3 minutes of standing. OH can reduce blood flow to organs above the heart, most notably the brain, and its symptoms can have a profound impact on your quality of life. OH is more common in the elderly, and certain medications, dehydration, varicose veins, severe anemia and conditions such as heart disease can lead to OH. OH can also be related to the nervous system. Parkinsons, pure autonomic failure, multiple system atrophy and other types of autonomic dysfunction can all cause OH.
OH can be caused by the body not releasing enough of the neurotransmitter, norepinephrine. When your body doesnt release enough norepinephrine, your blood vessels dont constrict when they need to, lowering your blood pressure and causing you to feel faint when you stand or sit up. When OH is caused by problems in the release of norepinephrine, it is referred to as neurogenic orthostatic hypotension .
Orthostatic Hypotension In Parkinsons Disease Multiple System Atrophy And Lewy Body Dementia
Movement disorder specialist, Dr. Veronica Santini spoke for a half hour on orthostatic hypotension, a common symptom of Parkinsons disease, Multiple System Atrophy and Lewy Body Dementia. Following her talk, moderator Candy Welch, Brain Support Networks MSA caregiver support group leader, presented Dr. Santini with questions from webinar participants for another half hour.
Also Check: Weighted Silverware
Functional Psychosocial And Healthcare Resource Use Impacts
Falls and their consequences are of high clinical concern inpatients with PD. Falls increase the risk of injuries and increase healthcareresource use . In patients with PD, symptoms of nOHare associated with increased risk of falls and impairment of activities ofdaily living . An increased rate of falls has been demonstrated even inpatients with asymptomatic nOH when compared with patients with PD without nOH . The greater risk of falls in patientswith nOH results in more emergency department visits, hospitalizations, and useof outpatient services . In a retrospective cohortstudy, unadjusted medically attended fall-related costs were significantlyhigher for patients with PD and nOH than for patients with PD alone . Similarly, another retrospective study found thatoverall healthcare costs were more than 250% higher in patients with PD and nOHthan in those with PD alone ,even after adjusting for confounding factors .
Preventing And Treating Orthostatic Hypotension: As Easy As A B C
Drug therapy alone is never adequate to treat orthostatic hypotension. A patient-oriented approach that emphasizes education and nonpharmacologic strategies is critical. This article provides easy-to-remember management recommendations, using a combination of drug and non-drug treatments that have proven effective.
Don’t Miss: Parkinson Silverware
What Research Is Being Done
The NINDS supports research on disorders of the autonomic nervous system, including multiple system atrophy with orthostatic hypotension. This research is aimed at developing techniques to diagnose, treat, and prevent these disorders. Currently there are ongoing treatment trials of drugs to treat MSA.
National Institutes of Health National Institute of Neurological Disorders and Stroke
Last reviewed by a Cleveland Clinic medical professional on 02/07/2018.
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services.Policy
Impaired Ans Response To Standing In Noh
In patients with PD and nOH, autonomic dysfunction causes blood pressure to fall upon standing, due to an inappropriate NE response to postural change. Orthostatic hypotension has been defined as a drop in SBP of at least 20 mmHg or a drop in diastolic blood pressure of at least 10 mmHg after 3 minutes of standing. There is often a loss of the cardioacceleratory response too. Non-neurogenic causes of orthostatic hypotension are also common in patients with PD, and contribute to blood pressure drop. These non-neurogenic causes of orthostatic hypotension should be identified first, and include dehydration, medications, and cardiac pump failure. A clinical diagnosis of nOH can be made when these non-neurogenic causes of persistent orthostatic hypotension are excluded, and can be confirmed through autonomic testing and plasma NE levels.
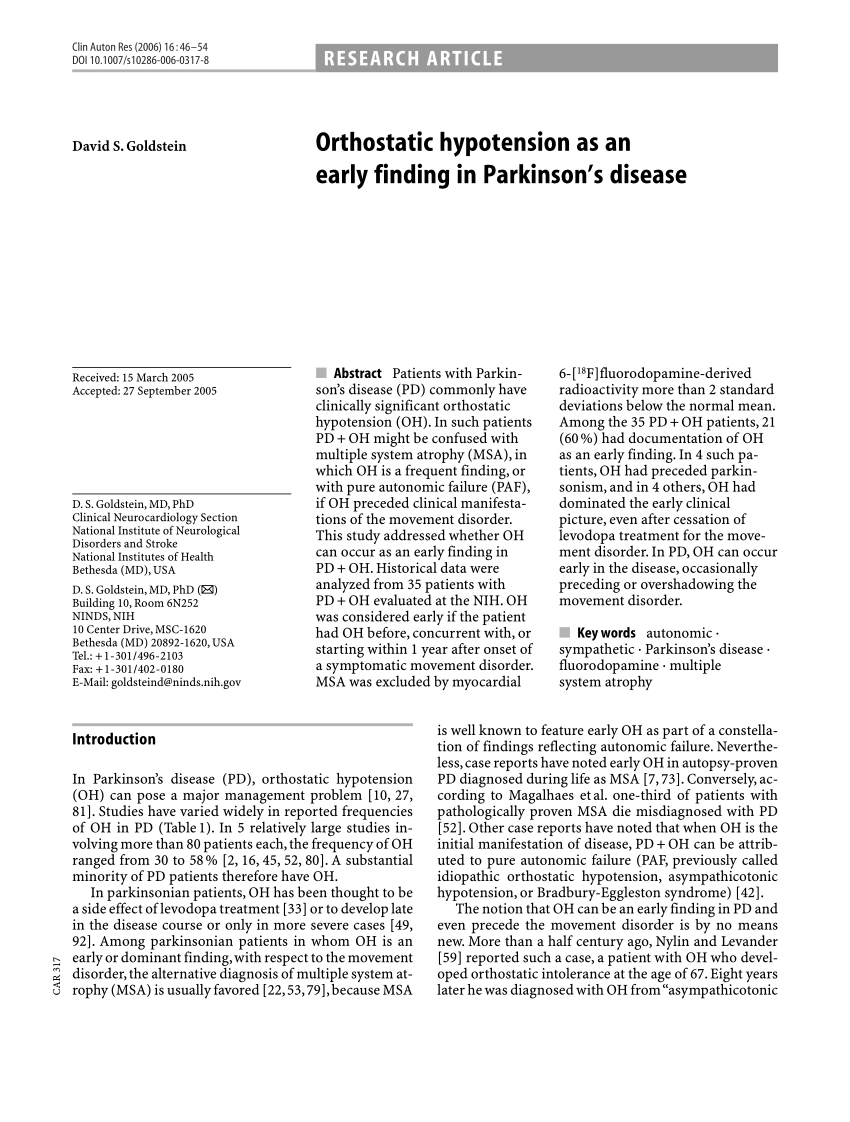
In PD, autonomic dysfunction is mainly a result of cardiac sympathetic denervation with inadequate activation of NE pathways, and also baroreflex failure. This can emerge during the course of PD or can occur early in its course. Parkinsonism due to multiple system atrophy is also accompanied by prominent autonomic dysfunction, but nOH results from failure of central NE pathways.,
Read Also: Sam Waterston Tremor
How Common Is Noh In People With Parkinsons
An estimated 30 to 50% of people with Parkinsons experience nOH. The prevalence of nOH increases with both age and number of years of living with Parkinsons. Although nOH in Parkinsons is relatively common, not everyone will experience symptoms. For that reason, people with Parkinsons should be screened for nOH, even if they have no symptoms.
Conversely, nOH can be one of the earliest symptoms of Parkinsons and can appear several years even decades before the onset of motor problems like tremor or stiffness. Therefore, people who have nOH, but do not have any significant motor or cognitive symptoms, should also be monitored closely to watch for early signs or symptoms of Parkinsons.
Temporal Variants Of Orthostatic Hypotension
In addition to OH defined as a BP drop within 3 min of standing , thereare two other temporally defined forms of OH that can be identified by clinicalBP measurements. Initial OH is a transient drop in BP that occurs immediatelyupon standing and resolves within 3060 s of active standing, and delayed OH isa sustained drop in BP that occurs beyond 3 min of standing . One large study of delayedOH monitored BP during 45 min of head-up tilt however, there is currently noaccepted standard for the length of time to test in the upright position forthis condition .
Initial OH differs from classical and delayed OH in several ways.Initial OH is defined by a greater magnitude of BP decrease within 15 s of active standing, withrestoration of normotensive BP within 3060 s . Signs and symptoms ofinitial OH are similar to those of the classical form of OH . However, initial OH is notassociated with a particular disease state or with autonomic failure, and theprevalence of initial OH in patients with PD is currently unknown .
Delayed OH occurs in some patients with PD and is thought to be related to, or aprecursor of, classical OH . In one study, more than half ofpatients with delayed OH developed classical OH during 10 years of follow-up. Delayed OH may be a mildor early form of sympathetic adrenergic failure and has been associated with thedevelopment of neurodegenerative disorders andincreased mortality .
Recommended Reading: Zhichan Capsule
When Is Orthostatic Hypotension Treated
Not all forms of orthostatic hypotension require treatment. If you experience a drop in blood pressure when you stand up, but have no other symptoms you probably won’t need treatment. Sometimes all it takes is sitting on the edge of the bed for a minute or steadying yourself for a moment after you stand up. But, if you feel dizzy or lightheaded to the point where you might lose your balance or lose consciousness, you will need treatment.
Because some drugs can cause severe orthostatic hypotension, your doctor may first try reducing some of your medicine or may switch you to another type of medicine. If you have significant symptoms of orthostatic hypotension, and it is not possible to change your medications, then your doctor will likely treat the orthostatic hypotension itself.
What Are The Symptoms Of Noh
nOH can appear with or without symptoms. The typical symptoms of nOH are lightheadedness, dizziness, blurry vision and, when theres a significant drop in blood pressure upon standing up, fainting. Symptoms almost always occur when standing up, less frequently when moving from standing to sitting and abate when lying down. People with nOH may also experience weakness, fatigue, leg buckling, headaches, neck and shoulder discomfort and shortness of breath. Severity of symptoms varies from day to day and fluctuates throughout the day. Often, mornings tend to be most difficult since nOH symptoms are aggravated by overnight urination, which is common in people with Parkinsons. Meals, particularly those rich in carbohydrates and sugars, also cause drops in blood pressure.
In people with Parkinsons, symptoms of nOH can also be non-specific, including fatigue and difficultly concentrating, and may sometimes mimic a levodopa off state. Its easy to miss nOH unless your physician measures your blood pressure while you are in a standing position. Conversely, it is important to realize people with Parkinsons can experience lightheadedness that mimics nOH, but may instead be caused by balance problems or other issues. For this reason, careful evaluation of your symptoms by a movement disorder specialist is strongly advised.
You May Like: Pfnca Wellness Programs