How Is It Treated And Is There A Cure
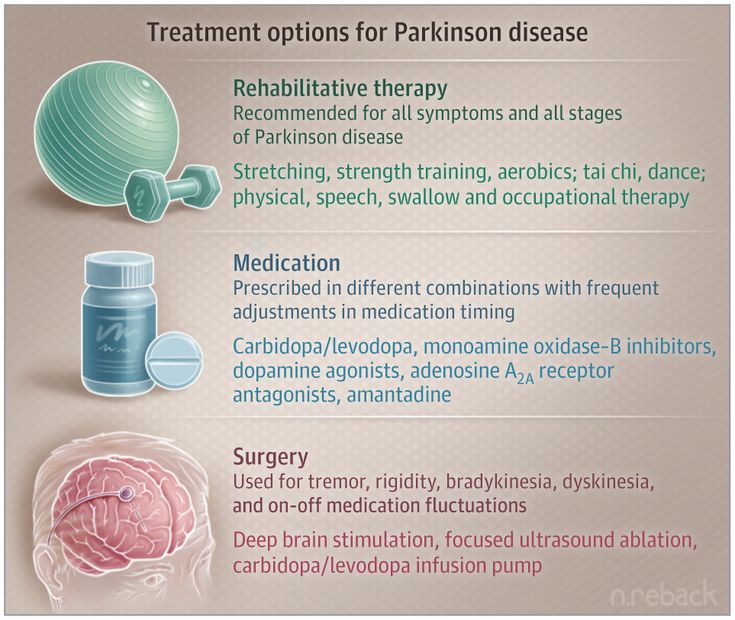
For now, Parkinsons disease is not curable, but there are multiple ways to manage its symptoms. The treatments can also vary from person to person, depending on their specific symptoms and how well certain treatments work. Medications are the primary way to treat this condition.
A secondary treatment option is a surgery to implant a device that will deliver a mild electrical current to part of your brain . There are also some experimental options, such as stem cell-based treatments, but their availability often varies, and many aren’t an option for people with Parkinsons disease.
How Do I Take Care Of Myself
If you have Parkinsons disease, the best thing you can do is follow the guidance of your healthcare provider on how to take care of yourself.
- Take your medication as prescribed. Taking your medications can make a huge difference in the symptoms of Parkinson’s disease. You should take your medications as prescribed and talk to your provider if you notice side effects or start to feel like your medications aren’t as effective.
- See your provider as recommended. Your healthcare provider will set up a schedule for you to see them. These visits are especially important to help with managing your conditions and finding the right medications and dosages.
- Dont ignore or avoid symptoms. Parkinsons disease can cause a wide range of symptoms, many of which are treatable by treating the condition or the symptoms themselves. Treatment can make a major difference in keeping symptoms from having worse effects.
Who Does It Affect
The risk of developing Parkinsons disease naturally increases with age, and the average age at which it starts is 60 years old. Its slightly more common in men or people designated male at birth than in women or people designated female at birth .
While Parkinsons disease is usually age-related, it can happen in adults as young as 20 .
Don’t Miss: Parkinson’s Masked Face Images
Support For People Living With Parkinsons Disease
While the progression of Parkinsons is usually slow, eventually a persons daily routines may be affected. Activities such as working, taking care of a home, and participating in social activities with friends may become challenging. Experiencing these changes can be difficult, but support groups can help people cope. These groups can provide information, advice, and connections to resources for those living with Parkinsons disease, their families, and caregivers. The organizations listed below can help people find local support groups and other resources in their communities.
Studying The Heterogeneity Of Pre

The pre-diagnostic phase of PD is heterogeneous with regards to risk factors, biomarkers and prodromal symptoms . Taking into account this heterogeneity in population-based studies is essential because a lack of insight into interactions between risk factors and subgroup differences in prodromal symptoms precludes our understanding of the different pathophysiological processes involved in PD and hinders early disease recognition.
Important developments regarding the complex interaction between risk factors of PD stem from studies on gene-environment interactions . Studying the interplay between genetics and the environment provides insights into why only certain individuals exposed to environmental risk factors develop PD. The interaction between genetic mutations and pesticides is a major field of study herein . A 2012 study, for example, showed that the association between paraquat exposure and PD was seven times greater in men with homozygous deletions of GSTT1, a gene involved in the metabolism of chemical substances, than in men with functional GSTT1 . Further application of these methods in population-based studies on environmental and lifestyle risk factors is warranted.
Also Check: Drugs Prescribed For Parkinson’s Disease
Lifestyle Factors And Parkinsons Disease Risk In A Rural New England Case
Angeline S. AndrewAcademic Editor: Received
Abstract
Introduction. Parkinsons disease is an age-related neurodegenerative disease likely caused by complex interactions between genetic and environmental risk factors. Exposure to pesticides, toxic metals, solvents, and history of traumatic brain injury have been implicated as environmental risk factors for PD, underscoring the importance of identifying risk factors associated with PD across different communities. Methods. We conducted a questionnaire-based case-control study in a rural area on the New Hampshire/Vermont border, enrolling PD patients and age- and sex-matched controls from the general population between 2017 and 2020. We assessed frequent participation in a variety of recreational and occupational activities and surveyed potential chemical exposures. Results. Suffering from head trauma or a concussion prior to diagnosis was associated with a fourfold increased risk of PD. Adjustment for head trauma negated any risk of participation in strenuous athletic activities. We observed a 2.7-fold increased risk of PD associated with activities involving lead .. Implicating these factors in PD risk favors public health efforts in exposure mitigation while also motivating future work mechanisms and intervention opportunities.
1. Introduction
2. Methods
3. Results
4. Discussion
Data Availability
Conflicts of Interest
Ethics Approval And Consent To Participate
The study received human research ethics approval by the Griffith University Human Research Ethics Committee . All participants gave written informed consent prior to taking part in the study. All protocols were approved by the Griffith University Human Research Ethics Committee and were conducted in accordance with their regulations and guidelines.
Consent for publication.
Not applicable.
You May Like: Very First Signs Of Parkinson’s
What Tests Will Be Done To Diagnose This Condition
When healthcare providers suspect Parkinsons disease or need to rule out other conditions, various imaging and diagnostic tests are possible. These include:
New lab tests are possible
Researchers have found possible ways to test for possible indicators or Parkinsons disease. Both of these new tests involve the alpha-synuclein protein but test for it in new, unusual ways. While these tests cant tell you what conditions you have because of misfolded alpha-synuclein proteins, that information can still help your provider make a diagnosis.
The two tests use the following methods.
- Spinal tap. One of these tests looks for misfolded alpha-synuclein proteins in cerebrospinal fluid, which is the fluid that surrounds your brain and spinal cord. This test involves a spinal tap , where a healthcare provider inserts a needle into your spinal canal to collect some cerebrospinal fluid for testing.
- Skin biopsy. Another possible test involves a biopsy of surface nerve tissue. A biopsy includes collecting a small sample of your skin, including the nerves in the skin. The samples come from a spot on your back and two spots on your leg. Analyzing the samples can help determine if your alpha-synuclein has a certain kind of malfunction that could increase the risk of developing Parkinsons disease.
Brain Connectomic Studies And Improved Precision Of Neuromodulation Targets
The process of altering brain function through direct manipulation of neural activity has long been used to treat patients with neuropsychiatric disorders and deep brain stimulation has provided clinical benefit to more than 150 000 patients with PD, dystonia and essential tremor . Apart from the conventional application in advanced PD, DBS has also been suggested to exert disease-modifying traits . In multiple preclinical studies on rat models, chronic STN electrical stimulation was shown to result in preservation of SNpc dopaminergic neurons and an increase of brain-derived neurotrophic factors followed by activation of the tropomyosin receptor kinase type B receptor signaling in the nigrostriatal system . Although preclinical experiments suggest potential neuroprotective effects of DBS, results from clinical studies have shown that dopaminergic neuron degeneration remains unaltered , and -syn burden is not reduced in PD patients treated with DBS .
Focused ultrasound as a newly developed neuromodulation technique
Repetitive transcranial magnetic stimulation
Few studies have investigated the effect of rTMS on levodopa-induced dyskinesias, showing only short-lasting or no beneficial effect.
Don’t Miss: The Last Stages Of Parkinson’s Disease
Parkinsons Disease Researchers To Study Brain Circuits Driving Symptoms
Northwestern University scientists have received two awards for Parkinsons disease research from the ASAP Collaborative Research Network, a program of the Aligning Science Across Parkinsons initiative implemented with partner The Michael J. Fox Foundation for Parkinsons Research.
ASAP supports multidisciplinary, multi-institutional research teams to address key knowledge gaps in the basic circuit mechanisms that contribute to the development and progression of Parkinsons disease.
A team led by D. James Surmeier, the Nathan Smith Davis Professor and chair of neuroscience at Northwestern University Feinberg School of Medicine, received a $9 million award over three years. He and his collaborators will investigate how the dysfunction of brain circuits begins and then evolves to cause difficulty in moving and sleeping. This will allow earlier diagnosis of Parkinsons disease and increase the chances of stopping and better treating the disease with pharmacological and genetic therapies once it appears.
His project is titled Distributed circuit dysfunction underlying motor and sleep deficits in a progressive mouse model of Parkinsons disease. Surmeier, the principal investigator, will collaborate with Ann Kennedy from Northwestern Rui Costa at Columbia University Yang Dan at University of California, Berkeley Silvia Arber at University of Basel and Jun Ding at Stanford University.
Northwestern scientists discuss their research projects for these awards:
How Soon After Treatment Will I Feel Better And How Long Will It Take To Recover
The time it takes to recover and see the effects of Parkinson’s disease treatments depends strongly on the type of treatments, the severity of the condition and other factors. Your healthcare provider is the best person to offer more information about what you can expect from treatment. The information they give you can consider any unique factors that might affect what you experience.
Also Check: Does Parkinson’s Make You Forget Things
Trends In Ylds Caused By Pd
In 2019, the number of YLDs caused by PD was 1210.09 × 103 globally, with an increase of 154.73% since 1990. The overall ASR of YLDs reported an increasing trend from 1990 to 2019, with the EAPC of 0.53 . Male patients had a higher burden, and undertook a larger increasing trend than female patients . Among the age groups, the highest YLD number was seen in the age group of over 80 years , and the percentage increased pronouncedly among the patients aged 45 years old .
Table 2. The changes in YLDs of Parkinson’s disease worldwide, and in sexes, SDI areas, and regions, 19902019.
The upward trend in the ASR of YLDs occurred in all SDI areas from 1990 to 2019, particularly the middle one . In terms of geographic regions, the largest number of YLDs was seen in East Asia , while the lowest one was in Oceania . The percentage of YLDs number increased from 27.97% in Eastern Europe to 256.90% in Central Latin America during 19902019. The ASR of YLDs ranged from 8.01/100,000 in Eastern SubSaharan Africa to 20.84/100,000 in East Asia. Increasing trends in the ASR of YLDs occurred in most regions, particularly East Asia . However, a minor decreasing trend was found in Oceania . The ASRs of YLDs were positively associated with SDI among the regions in 2019 .
Trends In The Pd Incidence
Globally, the incident number of PD was 1,081.72 × 103 in 2019, which increased 159.73% since 1990. The overall age-standardized incidence rate was 13.43/100,000 in 2019, and it increased with an annual average of 0.61% from 1990 to 2019 . Compared to female patients, male patients had a larger incident number, and a higher increasing trend in ASIR . Among the age groups, the high incident numbers of PD were observed in the patients aged over 65 years, and the largest increasing percentage occurred in the age group of over 80 years .
Table 1. The changes in incidence and prevalence of Parkinson’s disease worldwide, and in sexes, SDI areas, and regions, 19902019.
Figure 1. Trends in the ASR of incidence, prevalence, and YLDs of Parkinson’s disease in global, SDI areas and geographic regions from 1990 to 2019. ASR, age-standardized rate SDI, sociodemographic index YLDs, years lived with disability.
Figure 2. The distribution of Parkinson’s disease incidence in age groups, SDI areas and geographic regions from 1990 to 2019. was the incident number in age groups was the ASIR in SDI areas was the incident number in geographical regions. ASIR, age-standardized incidence rate SDI, sociodemographic index.
Don’t Miss: How Does A Person Get Parkinson’s Disease
What Can I Expect If I Have This Condition
Parkinsons disease is a degenerative condition, meaning the effects on your brain get worse over time. However, this condition usually takes time to get worse. Most people have a normal life span with this condition.
You’ll need little to no help in the earlier stages and can keep living independently. As the effects worsen, youll need medication to limit how the symptoms affect you. Most medications, especially levodopa, are moderately or even very effective once your provider finds the minimum dose you need to treat your symptoms.
Most of the effects and symptoms are manageable with treatment, but the treatments become less effective and more complicated over time. Living independently will also become more and more difficult as the disease worsens.
How long does Parkinsons disease last?
Parkinsons disease isnt curable, which means its a permanent, life-long condition.
Whats the outlook for Parkinsons disease?
Parkinson’s disease isn’t fatal, but the symptoms and effects are often contributing factors to death. The average life expectancy for Parkinson’s disease in 1967 was a little under 10 years. Since then, the average life expectancy has increased by about 55%, rising to more than 14.5 years. That, combined with the fact that Parkinson’s diagnosis is much more likely after age 60, means this condition doesn’t often affect your life expectancy by more than a few years .
Dysfunctional Protein Clearance Systems
There are two central protein clearance systems within cells responsible for the removal of dysfunctional proteins: the ubiquitin-proteasome system and the autophagy-lysosome pathway. The UPS is primarily responsible for breaking down abnormal proteins, and it does so by tagging them with ubiquitin and transporting them to the proteasome for degradation. The autophagy-lysosome pathway is divided into three constituents: macroautophagy, microautophagy, and chaperone-mediated autophagy . Briefly, in macroautophagy, intracellular components, including cytosolic proteins, are engulfed by the autophagosome, which then fuses with the lysosome, leading to the breakdown of its contents. On the other hand, in microautophagy, the lysosome alone engulfs and destroys cytoplasmic components. CMA is a more selective process, whereby molecular chaperones target specific proteins and transport them to the lysosome for degradation . Monomeric -synuclein is generally cleared by both the UPS and the autophagy-lysosome pathway , and damage in either of their machineries is implicated in the pathogenesis of PD by contributing to the accumulation of defective proteins, in particular soluble misfolded -synuclein .
Read Also: What Prevents Parkinson’s Disease
Glucagonlike Peptide 1 Receptor Agonists And Other Antidiabetic Agents
Biological processes involved in PD share common features with obesity and type 2 diabetes mellitus , including the dysregulation of insulin signaling in the brain. The term brain insulin resistance has been suggested to describe decreased sensitivity of CNS pathways to insulin, followed by disturbances in synaptic, metabolic and immune response functions . Strategies to normalize insulin sensitivity in neurons have thus been in the spotlight of clinical trials aiming to establish whether they may provide neuroprotective actions.
The neuroprotective effect of GLP-1 RAs is assumed to be mediated by improved brain insulin sensitivity however, human studies evaluating their biological effect in the CNS are limited. Functional MRI imaging studies have primarily focused on investigating brain networks involved in the anorectic effect of GLP-1 RAs , but sparse mechanistic data are available for understanding neuroprotective effects of these drugs. In a more recent trial of exenatide in PD, disease modifying effects measured by nigrostriatal dopamine transporter imaging were reported . Subsequently, brain insulin and Akt signaling pathways were also evaluated in neuronal-derived exosomes and it was shown that exenatide treatment, but not placebo, activated these pathways . This significant, secondary analysis of the trial increases understanding of the molecular mechanism underlying the treatment effect and provides a possible biomarker to measure target engagement.
Enhancing Healthcare Team Outcomes
Interprofessional management
PD is the most common motor disorder in the U.S. The disorder has no cure and is progressive. The condition can present with motor abnormalities and a variety of psychiatric and autonomic problems. Almost every organ is affected by this disorder, and as the disease progresses, management can be difficult. An interprofessional team approach is the best way to manage the disorder.
Besides, physicians, nurses, pharmacists, social workers, and physical therapists play a vital role in the daily management of these patients. Nurses have many roles when it comes to looking after patients with PD. The first is the education of the patient and family and encouraging them to participate in decisions regarding the treatment. In addition, nurses are often the first to spot difficulties in daily living and hence should make the appropriate referrals or recommendations. Nurses also provide psychosocial support and referral to a therapist, if required. Finally, the nurse plays a key role in assessing the risk of falls and making referrals to a physical therapist for an ambulatory device. Other issues commonly encountered in these patients that require attention include dysphagia, cognitive decline, depression, and somnolence.
Finally, the nurse should provide information on end of life care, financial planning, disability application, and referral to a nursing home.
These interprofessional team strategies will lead to better outcomes for PD patients.
Outcomes
Recommended Reading: Charity Navigator Parkinson’s Foundation
Evaluation Of Motor Complications In Parkinsons Disease: Understanding The Perception Gap Between Patients And Physicians
Abstract
1. Introduction
Parkinsons disease is a complex, heterogeneous, neurodegenerative disease characterized by progressive motor symptoms, including tremors, rigidity, and bradykinesia, with postural instability often appearing as the disease progresses . PD is also associated with various nonmotor symptoms, such as cognitive and psychiatric disturbances, autonomic dysfunction, sleep disorders, pain, fatigue, and olfactory dysfunction . As PD is an incurable progressive condition, the aim of treatment is to control symptoms for as long as possible, improve mobility and function, and maintain the overall quality of life of patients .
WO is underestimated by physicians. Results from two trials have shown that patients identified the presence of WO on the basis of the self-administered WOQ-9 and WOQ-19 more frequently than did physicians during neurological evaluation. Although several studies have examined the potential differences in the perception of WO between patients and physicians , detailed investigations, particularly in Japan, are lacking. We aimed to explore whether there were any differences in the perception of WO, as well as other health-related outcomes, between patients with PD and their physicians, as assessed in routine clinical practice in Japan.
2. Patients and Methods
2.1. Study Design
2.2. Study Methods
2.3. Eligibility
2.4. Study Endpoints
2.5. Sample Size Calculation and Statistical Analyses
3. Results
3.2. Presence of WO
4. Discussion