Comparing Multiple Sclerosis And Parkinsons Disease Causes
Multiple sclerosis is an autoimmune disease in which the immune system attacks the myelin, causing damage and thus exposing nerve fibers. Like many autoimmune diseases, the exact cause is unknown, but environmental, immunologic, infectious, and genetic factors have all been found to play a role in the onset of multiple sclerosis.
When certain nerve cells in the brain begin to die or break down that is what causes Parkinsons disease, but why this occurs is unclear. Some factors that contribute to nerve cell death include genetics as specific gene mutations have been identified to contribute to Parkinsons disease, environmental factors such as exposure to certain toxins, the presence of Lewy bodies in the brain as well as alpha-synuclein found in Lewy bodies.
Dealing With Overlap Of Primary Studies
Overlap of primary studies within included systematic reviews is a challenge exclusive to umbrella reviews. Currently, there is a lack of guidance on how best to manage this occurrence . To maximise comprehensiveness of this umbrella review, we employed a full inclusion scenario where all Cochrane reviews and non-Cochrane reviews were included . A list of the primary studies included in each systematic review was assembled and a matrix of evidence table was created to determine the amount of overlap between systematic reviews. To avoid double-counting outcome data the following were decided:
-
Any systematic review that contained a relevant primary study that was not in any other systematic review was included so that data were not lost.
-
Any systematic review that did not contain any unique primary study was excluded to minimise duplication of data.
-
In the presence of complete overlap between reviews, the highest quality review, as determined by the A MeaSurement Tool to Assess Systematic Reviews 2 was included in data synthesis and analysis.
-
In cases where there was a complete overlap between reviews and they received the same AMSTAR 2 rating, then the most recently published review was included.
-
In the presence of partial overlap, all reviews were included but the degree of overlap was noted and its implications on the findings of this umbrella review were discussed.
Who Gets Als And Ms
MS is estimated to affect over 2.3 million people worldwide, with approximately 1 million of them in the United States.
Around 30,000 people in the United States live with ALS, according to the Hospital for Special Surgery. Over 5,600 people in the country are diagnosed with ALS every year.
There are several risk factors that may affect who develops ALS and MS.
You May Like: Parkinson Disease And Tooth Extraction
Also Check: Parkinson’s Disease And Sleep Disorders
Research To Find Msa Biomarkers And An Earlier Msa Diagnosis
An important goal of the Coalitions MSA Research Program is to fund and encourage the development of biomarkers to distinguish PD from MSA at a much earlier stage.The stakes are high.An accurate biomarker could lead to quicker development of treatments.In fact, a concern in past clinical trials of MSA treatments that failed is that maybe the patients in the trial are too late stage to show effectiveness.Increasing the number of known early stage MSA patients could improve the likelihood of finding treatments and even a cure.
Benefits Of Inpatient Rehabilitation

Inpatient rehabilitation hospitals are required to provide an interdisciplinary approach to patient caremeaning specialists from many disciplines are involved in creating and implementing a patients care plan. Interdisciplinary team members include physical, speech and occupational therapists, rehabilitation physicians, nurses, case managers, dietitians and pharmacists. Patients participate in three hours of therapy each day for a total of 15 hours per week, and an individualized plan of care is created for each patient to meet their needs while providing necessary intervention to make functional gains. Inpatient rehabilitation can be beneficial for both MS and Parkinsons disease.
Educational sessions with the patient and family members can also improve understanding for all involved in the patients care about the progression of each disease and ways to combat symptoms.
Bethany Moss is a physical therapist at Encompass Health Rehabilitation Hospital of Jonesboro. She is a PWR! certified therapist and a LVST BIG certified clinician.
Also Check: Latest Treatment For Parkinson’s
Multiple Sclerosis Vs Parkinsons Disease: Us Prevalence And Economic Impact
Anyone can develop multiple sclerosis, but it mostly affects 20- to 40-year-olds. Prevalence of multiple sclerosis in the U.S. is estimated at over 400,000 cases, and nearly 200 new cases are diagnosed each week. Rates of multiple sclerosis are highest in areas furthest away from the equator, so the rates are higher in the Northern U.S.
Direct and indirect costs resulting from multiple sclerosis can range from $8,528 to $54,244.
One million Americans live with Parkinsons disease. The average cost of Parkinsons disease including treatment, lost work wages, and social security payments is $25 billion annually in the U.S.
Ethics Approval And Consent To Participate
The study was carried out in accordance with the recommendations of the Oregon Health & Science University institutional review board with written informed consent from all subjects. All subjects gave written informed consent in accordance with the Declaration of Helsinki. The protocols were approved by the OHSU IRB .
Read Also: Is There Pain With Parkinsons
Don’t Miss: Typical Symptoms Of Parkinson’s Disease
Expert Panel Opinions: Parkinsons Disease Multiple Sclerosis And Cmv Driver Safety
Expert Panel Opinions: Parkinsons Disease, Multiple Sclerosis and CMV Driver Safety
Matthew Rizzo, M.D.
DOT is committed to ensuring that information is available in appropriate alternative formats to meet the requirements of persons who have a disability. If you require an alternative version of files provided on this page, please contact.
U.S. DEPARTMENT OF TRANSPORTATION
Federal Motor Carrier Safety Administration
1200 NEW JERSEY AVENUE, SE
WASHINGTON, DC 20590
Characteristics Of Restless Leg Syndrome
There are certain features of RLS that make it a unique and specific disorder.
Recommended Reading: Most Common Parkinson’s Medications
Comparison Of Static Sway Performance Within One Group Between Different Tasks
Healthy adults showed a significant increase in sway area , velocity in ML direction , acceleration in ML direction and jerk in both AP and ML direction between the side-by-side and tandem stance . The sway area , velocity in ML direction , acceleration in ML direction and jerk in both AP and ML direction significantly increased between the semi-tandem and tandem stance .
Table 4. Significant changes of sway parameters between tasks.
MS patients showed a significant increase in sway velocity , acceleration in ML direction and jerk in ML and AP direction between side-by-side and tandem stance. Moreover, they showed a significant increase in sway acceleration in ML direction and jerk in ML direction between semi-tandem and tandem stance .
PD patients did not show a significant change in any of the sway parameters between the tasks .
What Makes Them Different
MS and Parkinsonâs have different causes. They usually start to affect you at different ages, too.
MS often affects people between ages 20 and 50, but children get it, too. Parkinsonâs usually starts at age 60 or older, but some younger adults get it.
MS is an autoimmune disease. That means your bodyâs immune system goes haywire for some reason. It attacks and destroys myelin. As myelin breaks down, your nerves and nerve fibers get frayed.
In Parkinsonâs, certain brain cells start to die off. Your brain makes less and less of a chemical called dopamine that helps control your movement. As your levels dip, you lose more of this control.
Some genes may put you at risk for Parkinsonâs, especially as you age. Thereâs a small chance that people who are exposed to toxic chemicals like pesticides or weed killers can get it, too.
These symptoms are more common if you have MS. They are not usually found in Parkinsonâs:
Don’t Miss: Parkinson’s Plus Syndrome Icd 10
Is There A Link
Some people have MS and Parkinsonâs.
Research suggests that the damage that MS causes to your brain can lead some people to develop Parkinsonâs later on.
If you have MS, your immune system triggers ongoing inflammation. This can create lesions in your brain that cause Parkinsonâs disease. If lesions form in certain spots in your brain, they can affect how it makes dopamine.
Multiple Sclerosis Vs Parkinsons Disease Differences In Symptoms Causes And Treatment
Written byDr. Victor MarchionePublished onJune 10, 2016
Multiple sclerosis is an autoimmune condition that affects the nervous system, while Parkinsons disease is a progressive neurological disorder affecting movement. Symptoms of multiple sclerosis and Parkinsons disease are quite similar at times, but there are distinct differences setting the two conditions apart.
Causes of multiple sclerosis and Parkinsons disease are not well known, although there is some speculation to their roots. We will outline those speculated causes and highlight the symptoms, risk factors, complications, treatment, and therapies for both multiple sclerosis and Parkinsons disease to raise your awareness on each disorder.
Dont Miss: Primidone For Parkinsons Disease
Recommended Reading: Non Tremor Parkinson’s Disease
Key Difference Ms Vs Parkinsons
MS and Parkinsons disease are two diseases affecting the central nervous system. Multiple Sclerosis is a chronic autoimmune, T-cell mediated inflammatory disease affecting the central nervous system. On the other hand, Parkinsons disease is a movement disorder characterized by a decline in the dopamine level of the brain. Although MS is an autoimmune disorder, there is no immune component in the pathogenesis of Parkinsons disease. This is the key difference between MS and Parkinsons.
Also Check: Amino Acids And Parkinsons
Myth : Deep Brain Stimulation Is Experimental Therapy
Fact: Deep brain stimulation, or DBS, is a procedure in which doctors place electrodes in the brain at the point when medications are less effective in masking motor symptoms, such as tremor, stiffness and slowness of movement.
While it may sound frightening and futuristic, its been around and successfully used for decades. DBS works very similarly to a pacemaker, except the wire is in the brain, not in the heart. Its been a standard procedure for the past two decades.
Don’t Miss: Symptoms Of Parkinson’s Disease Tremor
Understanding Parkinsons And Multiple Sclerosis
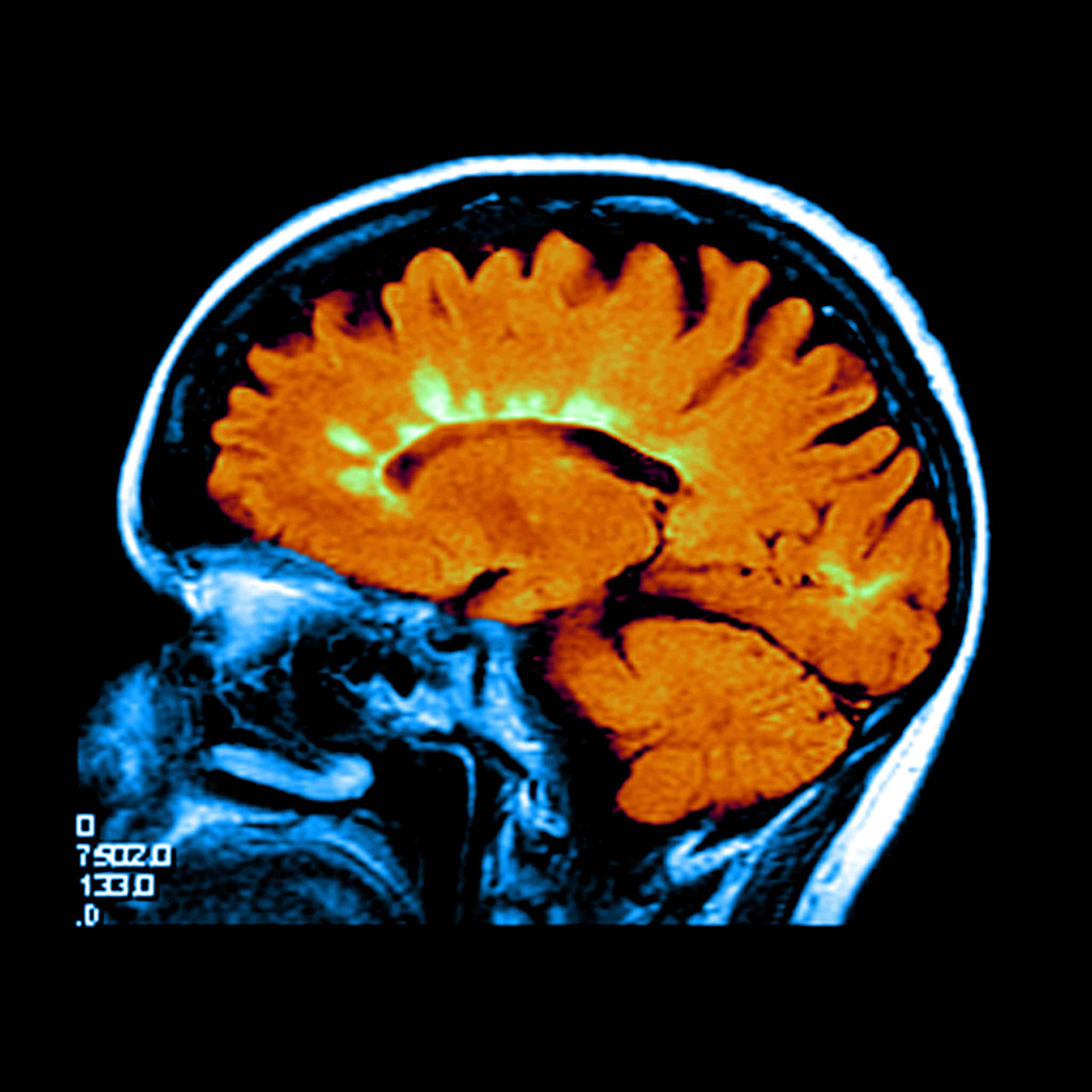
Parkinson’s disease is a neurological illness that impairs mobility. Symptoms appear gradually, sometimes beginning with a barely noticeable tremor in only one hand. It is one of the world’s most common nervous system disorders, which predominantly affects dopamine-producing neurons in the brain.
Multiple sclerosis, or MS, is a chronic condition that affects the brain, spinal cord, and optic nerves in the eyes. MS occurs when your immune system attacks the myelin, a fatty substance that wraps around your nerve fibers to protect them. Your nerves are injured if you don’t have this outer shell and scar tissue might occur. Because of the injury, your brain is unable to convey impulses across your body appropriately. Your nerves will also not work well and it will impair the way you move and feel.
Onset Of Als And Parkinsons
There are several different variants of ALS but it generally affects people between the age of 40 and 70. Juvenile onset ALS, however, can start in childhood or typically before the age of 25, although this form of ALS is particularly rare. The onset of ALS is estimated to be 20% more common in men compared with women and in 10% of cases there is likely to be a genetic component.
Parkinsons disease is usually diagnosed in people over the age of 60, though a small percentage exhibit the symptoms before the age of 50.
Once again, men are more likely to develop Parkinsons than women.
Recommended Reading: Latest Medication For Parkinson’s Disease
New Discovery Provides Hope For Lou Gehrigs Disease
Lou Gehrigs disease, also known as ALS , is a fatal neurodegenerative disorder for which there is no official treatment. However, in 2009 researchers reported on a group of patients with ALS and how they responded to being treated with stem cells. The majority of them did unbelievably well. And now, another study is again showing promise with stem cells.
Understanding Parkinsons Disease And Multiple Sclerosis
Parkinsons Disease is one of the most common neurodegenerative conditions in the world. It primarily damages the dopamine-producing neurons in a specific area of the brain called substantia nigra. Trained or well-experienced neurologists can diagnose PD based on early signs and symptoms, which include tremors, issues with balancing, stiffness or rigidity in the torso, legs, or arms.
On the other hand, Multiple Sclerosis is a chronic inflammatory condition of the central nervous system. It is an autoimmune demyelinating disease, which means the immune system mistakenly attacks normal tissues in this case, the myelin, or protective covering around nerve fibers. This leaves scarred tissues or lesions in multiple areas, disrupting electrical impulses throughout the body. When the myelin sheath is damaged, nerve impulses slow or even stop, causing neurological problems.
Multiple Sclerosis typically affects patients between the ages of 20 and 50, whereas the symptoms of Parkinsons usually show beyond the age of 60 and more. Furthermore, the outlook for Parkinsons Disease treatment as well as Multiple Sclerosis treatment varies, since there is no definitive Parkinsons Disease cure. While no single test can be used to diagnose both these conditions, PD focuses more on managing the symptoms and is known to not be reversible. Lifestyle changes, medications, and supportive therapies can always improve issues related to body movement.
Recommended Reading: Is There A Medical Test For Parkinson’s Disease
How Therapy Helps Ms And Parkinsons
While there are differences in Parkinsons and MS, physical, occupational and speech therapy can help both MS and PD patients improve their independence and safety, as well as achieve and maintain optimal function and cognition. Therapy can help prevent complications such as de-conditioning, muscle weakness from lack of mobility and muscle contractures related to spasticity. Training in energy conservation techniques and the use of adaptive tools and devices can help simplify everyday tasks. Therapists can even recommend strategic modifications to your home to ensure accessibility and safety even as the disease progresses.
Clinicians certified in LSVT ® and PWR! therapeutic programs can provide Parkinsons-specific exercises to target weight shifting, posture, trunk rotation and stepping strategies to overcome rigidity and slowness of movement. Education on specific exercises and strategies helps increase safety and slow the progression of the disease.
Differentiating Multiple Sclerosis Symptoms With Parkinsons Disease
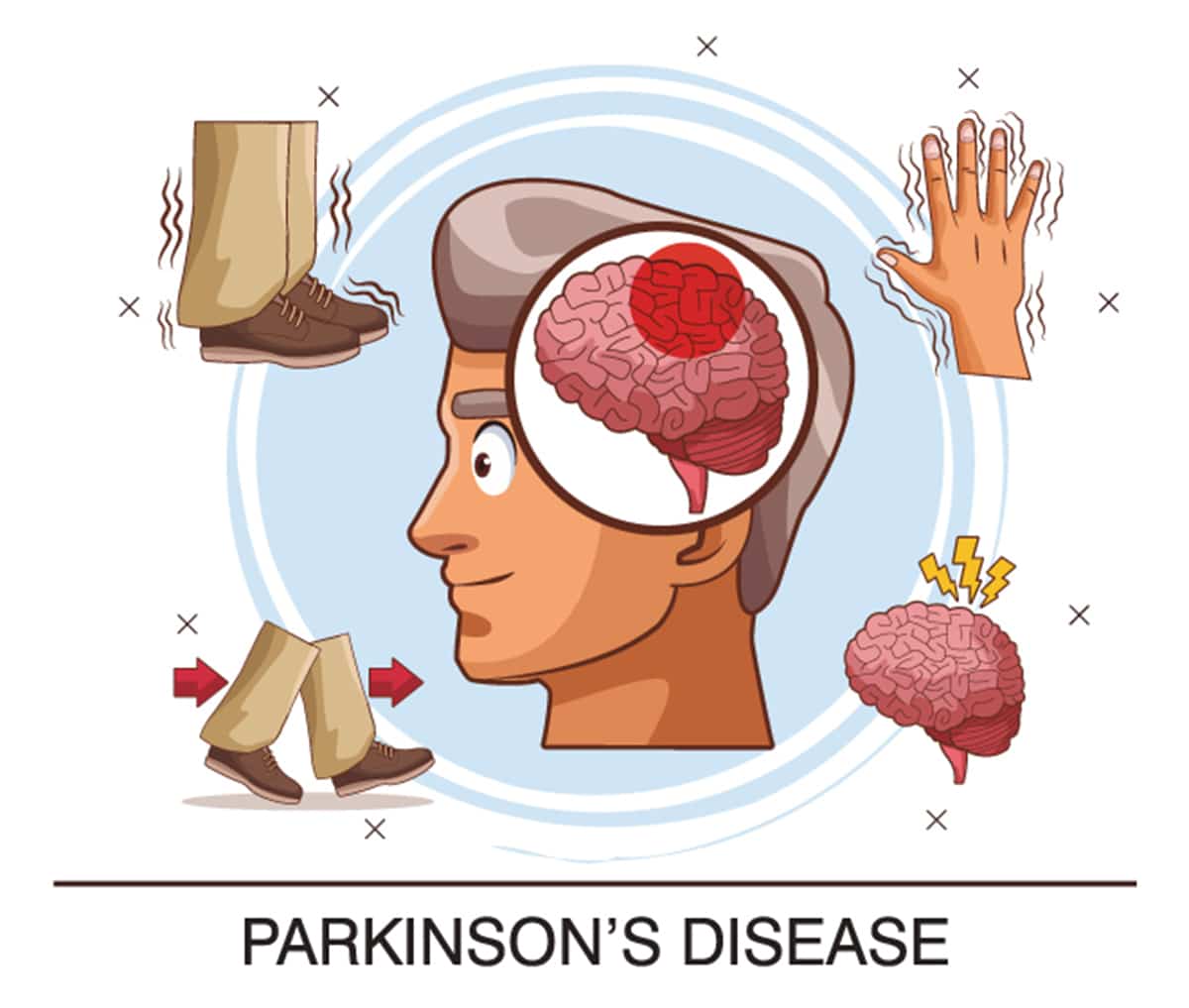
Signs and symptoms of multiple sclerosis include numbness or weakness in one or more limbs, partial or complete vision loss, prolonged double vision, tingling or pain, electric-shock sensations, tremors and lack of coordination, fatigue, dizziness, slurred speech, and problems with bowel and bladder function.
Parkinsons disease symptoms typically begin with tremors followed by muscle stiffness, difficulty standing or walking, changes in speech, slow movements, impaired posture and balance, loss of automatic movements, and writing changes.
As you can see, Parkinsons disease and multiple sclerosis do have some symptoms in common, which can make early diagnosis difficult.
Recommended Reading: Computer Mouse For Parkinson’s Patients
Multiple Sclerosis And Parkinson’s Disease
ABSTRACT
REFERENCES
Friese, M.A. Schattling, B. Fugger, L. Mechanisms of neurodegeneration and axonal dysfunction in multiple sclerosis. Nature Reviews Neurology 10, 225.
Thompson, A.J. Banwell, B.L. Barkhof, F. Carroll, W.M. Coetzee, T. Comi, G. Correale, J. Fazekas, F. Filippi, M. Freedman, M.S. Diagnosis of multiple sclerosis: 2017 revisions of the mcdonald criteria. The Lancet Neurology 2018, 17, 162-173.
Mehanna, R. Jankovic, J. Movement disorders in multiple sclerosis and other demyelinating diseases. Journal of the neurological sciences 2013, 328, 1-8.
Etemadifar, M. Afshar, F. Nasr, Z. Kheradmand, M. Parkinsonism associated with multiple sclerosis: A report of eight new cases and a review on the literature. Iranian journal of neurology 2014, 13, 88.
Moccia, M. Erro, R. Montella, S. Carotenuto, A. Pappatà, S. Orefice, G. Diagnostic challenges of parkinsonism occurring in multiple sclerosis. Acta Neurologica Belgica 2015, 115, 513-515.
Daroff, R.B. Jankovic, J. Mazziotta, J.C. Pomeroy, S.L. Bradley’s neurology in clinical practice seven edition ed. Elsevier Health Sciences: 2016.
Andersen, A.D. Binzer, M. Stenager, E. Gramsbergen, J.B. Cerebrospinal fluid biomarkers for Parkinsons disease: A systematic review Acta Neurologica Scandinavica 2016, 135, 34-56.
Gibb, W. Lees, A. The relevance of the lewy body to the pathogenesis of idiopathic Parkinsons disease. Journal of Neurology, Neurosurgery & Psychiatry 1988, 51, 745-752.
How Infections Can Cause Disease Progression
The researchers indicated that the findings could suggest the infections triggered or amplified a pre-existing disease process leading to neurodegenerative disease.
Dr. Melita Petrossian, a neurologist and director of the Movement Disorders Center at Providence Saint Johns Health Center in California, explained the connection.
An easy way to conceptualize the role of systemic inflammation in the risk of neurodegenerative disease is that the body works simultaneously over decades to fight infection and inflammation, and to clear out toxic or metabolic build-up that contributes to neurodegenerative disease, she told Healthline. The more focus the body has on fighting infection or inflammation, the less it can focus on clearing out metabolic building. Its like an army being overwhelmed on multiple fronts.
Another expert has a slightly different interpretation.
I am not convinced that infections cause the observed results concerning and . But, there are examples of infections triggering non-infectious syndromes, for example, rheumatic fever, streptococcal glomerulonephritis, Lyme disease, and Reiters syndrome, said Dr. Charles Bailey, medical director for infection prevention at Providence St. Joseph Hospital and Providence Mission Hospital in California.
The conditions include:
- Multiple system atrophy
- Progressive supranuclear palsy
For example:
Also Check: What Are The 5 Stages Of Parkinson’s