Correlational And Regression Analyses
Individual researcher rated apathy scores were analysed with the primary demographic, clinical, cognitive, mood, and personality measures in the Parkinson group using correlation statistics. Because of the number of pairwise comparisons, a conservative criterion was used for significance . Increasing apathy was associated with overall cognitive impairment as measured by the CAMCOG , and specifically with the subscales for language and memory . An association was found between the degree of apathy and measures of executive function including letter fluency , Stroop reading and interference , WCST categories and perseverative errors . A separate analysis of the associations with depression scores showed no significant relations for any of the above measures.
A series of exploratory regression analyses revealed that none of the clinical or demographic variablesalone or in combination predicted researcher rated apathy . Of the cognitive measures, the best set of predictors was the interference trial of the Stroop test and the COWAT verbal fluency .
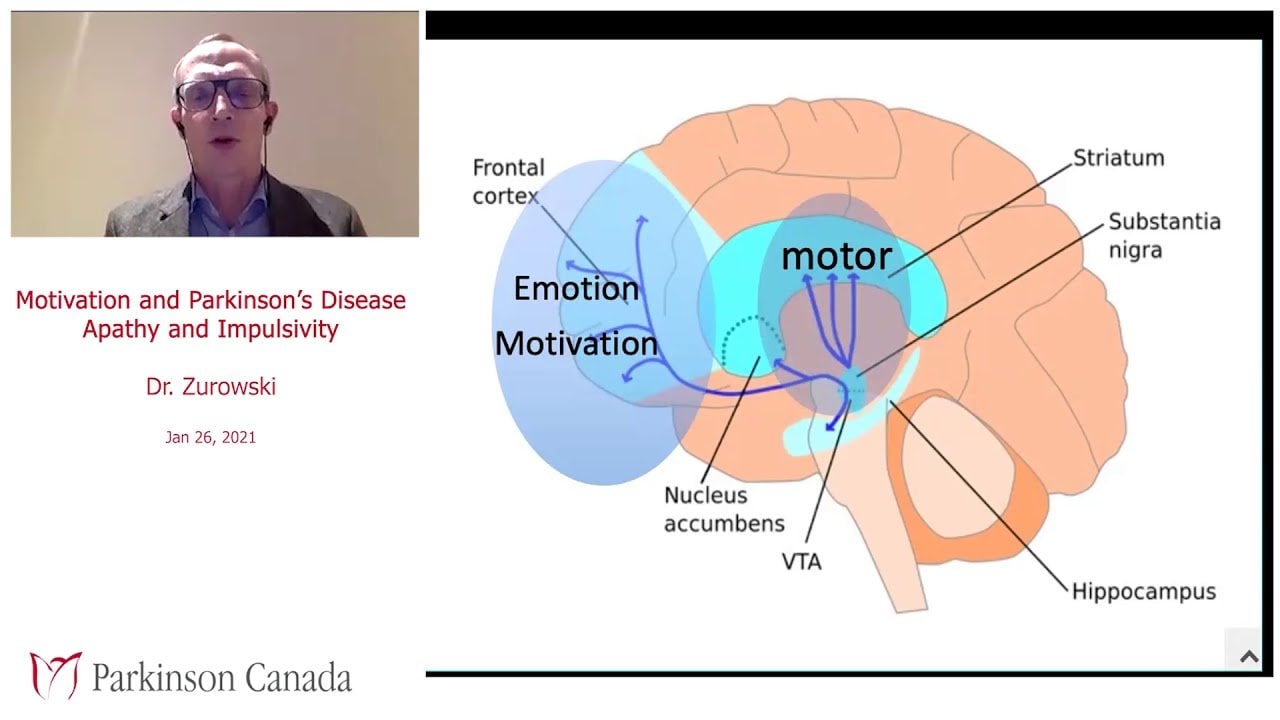
Neuroimaging Of Apathy In Pd
There were 14 neuroimaging studies of apathy in PD . Similar to the studies of depression and anxiety in PD, most imaging studies of apathy in PD utilized either PET or SPECT techniques , , , , , , , , and focused on measuring cerebral glucose metabolism with the exception of two PET studies , and one SPECT study examining dopaminergic changes associated with apathy. Of the 14 studies, five involved T1weighted imaging , , , , , two used RSFMRI , and one study performed DTI in addition to T1weighted imaging . Approximately half of the studies used ROI methods with caudate, putamen and limbic regions being the most common ROIs. All 14 studies excluded patients with cognitive symptoms and seven of them included patients who remained on antiparkinsonian medication during MRI scanning. Additionally, three of the 14 studies recruited patients who were on mood stabilizers. Amongst the 14 studies, five studies clearly excluded patients with depression , , , , , whilst seven studies did not , , , , , , and two did not indicate whether patients with depression were excluded from the studies , .
Apathy Can Be More Frustrating For Care Partners Than For People With Pd Themselves
A person with PD may be very aware of a change in his/her level of motivation. However sometimes apathy can be accompanied by a lack of self-awareness about the issue. The person with PD may feel content, does not understand why his/her care partner is so insistent that he/she participate in an activity and is not aware that his/her disinterest is actually a symptom of PD or is affecting those around him/her. This can fuel intense frustration and resentment in the care partner who may feel that My husband does not want to help himself! It can also make it hard for those who want to spend time with the person with PD and engage with them because they can be met with indifference or disinterest, which after a time can be discouraging. However, it is important to not give up and to still spend time with the person with PD, even if just sitting quietly together.
Read Also: Parkinson’s Disease Symptoms And Treatment
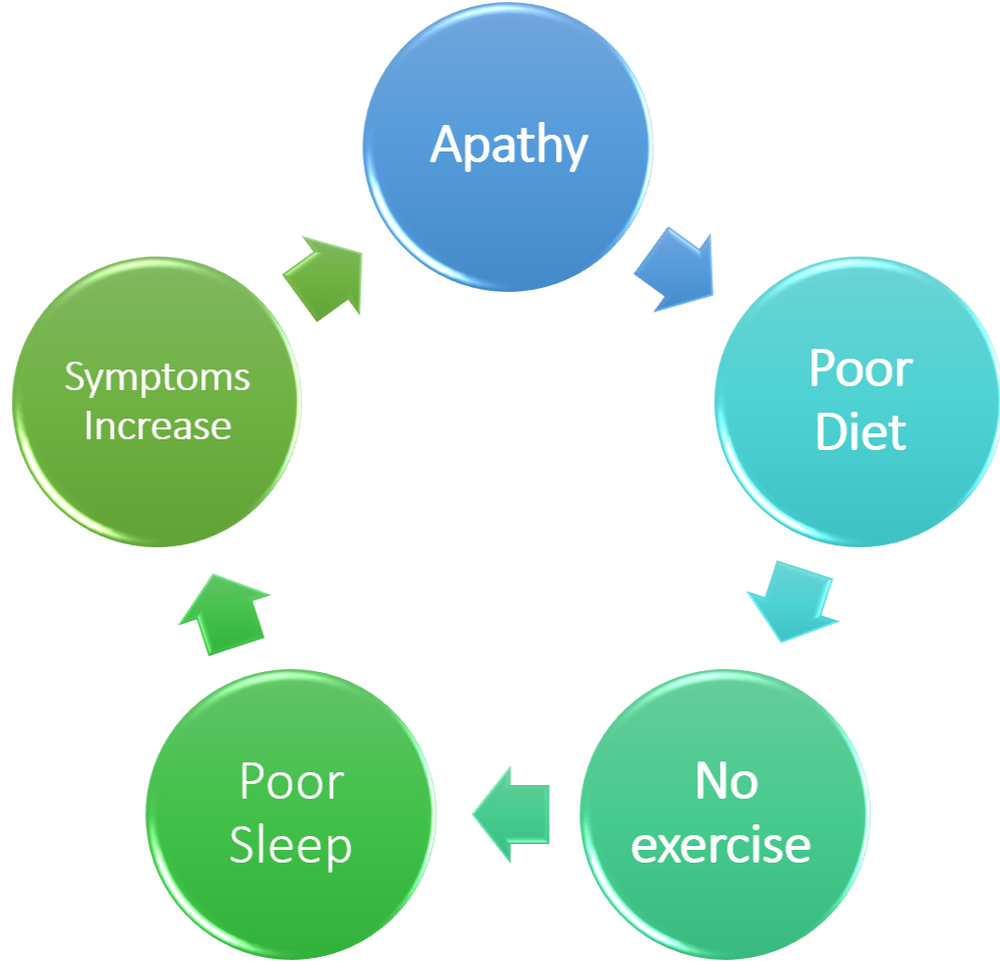
Apathy Can Interfere With Living Your Best Life With Pd
Apathy can interfere with a persons commitment to exercise, participation in therapy, or engagement in social opportunities, which makes it a big challenge for people with PD who, more than most, need to engage in these activities to stay as mobile and cognitively engaged as possible. Withdrawing from the things, activities and people you once enjoyed can have negative effects on your physical and mental health, so it is important to maintain at least some of the these elements despite the challenges of apathy.
Thanks For Signing Up
We are proud to have you as a part of our community. To ensure you receive the latest Parkinsons news, research updates and more, please check your email for a message from us. If you do not see our email, it may be in your spam folder. Just mark as not spam and you should receive our emails as expected.
You May Like: Average Age Of Parkinson’s Onset
Impact Of Apathy On Prognosis
Prospective longitudinal studies suggest that the presence of an apathy syndrome can worsen prognosis and is associated with a faster rate of cognitive and functional decline . In a 4-year follow-up of a cohort of over 350 AD patients, the rate of apathy was noted to increase as the disease progressed, and those with apathy declined faster and had a more severe course compared with those without apathy . Robert et al. followed a group of 251 patients with amnestic mild cognitive impairment for a year, and found that those who converted sooner to dementia had initial higher rates of apathy. In a group of non-demented PD patients followed-up at a median period of 18 months, more apathy sufferers had converted to dementia compared with those who did not have apathy at baseline . Furthermore, for the group who had not yet converted to dementia at follow-up, higher apathy was associated with more significant cognitive decline. Thus, it appears that apathy may be associated with more aggressive forms of AD and PD. It is not yet clear whether early intervention and amelioration of apathy will alter this poor prognosis.
Mood Hedonia And Personality
Mean scores derived from the assessments of depression, anxiety, hedonic tone, and personality are shown in table 3. Controlling for disability as measured by the SE scale, the total Parkinsons disease group was more depressed than the osteoarthritis group as assessed by the BDI but not by the HADS. Taking a cut off score of BDI 15, 43% of the Parkinsons disease group had possible depression compared with 8% of the osteoarthritis group. However, using the recommended cut off of 11 on the HADS, only two of the Parkinson group were identified as depressed compared with one in the osteoarthritis group. No significant group differences were found for mean anxiety, although a large number in each group scored above the cut off score . The Parkinsons disease and osteoarthritis groups did not differ in mean hedonic tone scores on the SHPS when measured on a Likert scale. Measuring on a binary scale and with a cut off of 3, none of the osteoarthritis group was impaired, compared with three from the Parkinson group. However, all but one scored just above the cut off, and all showed significant comorbid depressive symptomatology. The two groups did not differ on any of the personality scales assessed by the TPQ.
Table 3
Scores for the Parkinsons disease and osteoarthrisits groups on assessments of mood , hedonic tone , and personality
Don’t Miss: Stabilizing Spoon For Parkinson’s
Measurement Of Apathy And Impulsivity
For the purposes of the detailed analysis of the distribution and phenomenology of apathy, we used the 18-item Apathy Evaluation Scale, Clinician version . On this scale, each item is scored on a 4-point Likert scale and higher scores indicate worse apathy. The individual items on the scale have been classified into one of three domains: cognitive, behavioural, or emotional. This scale has previously been used in PD and has been shown to have good internal consistency .
Levels of impulsivity were assessed using the 30-item Barratt Impulsiveness Scale . This is a self-report questionnaire which is not specific to PD. It is rated on a 4-point Likert scale , which can be reported as a total impulsivity score, or as three subscale scores: nonplanning impulsiveness , motor impulsiveness , and cognitive impulsiveness .
How People With Parkinson’s Can Beat Apathy
Following an assessment of your symptoms and diagnosis of apathy, your healthcare provider may discuss medications directed at increasing energy or other medications directed at the dopamine, cholinergic, and serotonergic systems . But more importantly, are the behavioral changes that we must make ourselves.
Read Also: Weighted Silverware For Parkinson’s
How Can I Help Myself
It is important to remember that apathy is a common symptom of Parkinsons and can be effectively treated. Feelings of indifference and lack of motivation may become a vicious circle if untreated, so it is important that you seek help and accept support that is offered to you, both by professionals and your family and carer.
Below are some suggestions that you may find helpful:
- Educate yourself about Parkinsons, its cause and treatment. Being informed generally helps you to feel more in control.
- Try to take an active role in managing your illness.
- Make information available to your carers so that they understand that apathy is the reason for your apparent lack of interest or emotion. For carers, it will be important to continue with their own activities to avoid becoming dispirited by the persons apathy.
- Be open with your doctor and other healthcare professionals this will make it easier for them to help you.
- Try to continue with activities you enjoy. If you have stopped most activities, restart them one at a time. Research shows that keeping active can improve your mood and make you feel more positive about yourself.
- Dont take on too much consider which activities are manageable. Ask your carer to help you plan your time.
- Try to stay relaxed. Complementary therapies such as yoga and Tai Chi may help with this.
- Accept help when you need it.
- Contact your local Parkinsons organisation or other support groups.
Definitions Of Apathy And Diagnostic Criteria
Apathy has been defined as a lack of goal-directed behaviour, which can be divided into: diminished or blunted emotions, loss of or diminished initiative, and loss of or diminished interest . Another, but similar, definition is that apathy represents a lack of goal-directed behaviour, cognition or emotion . Other formal definitions generally support the notion of apathy as a multi-dimensional construct, rather than merely a symptom secondary to other medical, psychiatric or neurologic conditions .
Table 1.
Diagnostic criteria for apathy validated in PD
You May Like: Non Shaking Parkinson’s Disease
Prevalances Of Apathy Depression Anxiety And Fatigue In The Sample Of Pd Patients
With 23.7, 13.4, 15.4, and 17.8%, the prevalence rates of significant apathy, mild-to-severe depression and anxiety and severe fatigue as assessed by the AES, HADS and FSS are comparable to other clinical PD samples albeit at the lower end of the spectrum. It must be noted that there are large ranges in published prevalence rates of psychiatric syndromes in PD possibly due to different measurement methods used in the various studies, different cut-off thresholds and clinical variability of study subjects. With almost ¼ of the patients showing significant apathetic symptoms, followed by severe fatigue, mild-to-severe anxiety and depression, apathy is the most frequent syndrome measured in this population of PD patients as assessed by the selected cut-off thresholds.
Context Setting And Sampling
The use of theoretical thematic analysis, applying the Theoretical Domains Framework and Behaviour Change Wheel , ensured evidence and interventions were directly linked. We estimated between four to six individuals per stakeholder group would be required to reach saturation .
Participants were divided into two groups: i) HCP including physicians, nurses, and allied health professionals and ii) persons with PD and apathy and/or their family caregivers. This was done to understand how different stakeholder groups use knowledge, and to help ensure persons with PD and their family caregivers would feel comfortable sharing their opinions. All participants spoke English, were not aphasic, and were able to provide informed consent.
HCP were recruited via convenience sampling. Practitioners were included if they were a neurologist, psychiatrist, psychologists, nurse, or allied health professional within the Calgary Movement Disorder Clinic , and had experience managing apathy in at least one individual with PD. HCP were contacted via email.
You May Like: Moringa And Parkinson’s Disease
Mbi Classification And Characteristics Of The Sample
The demographic and clinical characteristics of the sample are shown in . Among 60 participants with PD, 20 were categorized as having PD-MBI . In healthy controls, no participants met the MBI cut-point threshold 90% of them scored 0. The PD-MBI group showed higher MBI domain scores than the PD-noMBI group in all domains. The PD-MBI group had higher UPDRS-III scores than the PD-noMBI group and fewer education years than healthy controls.
Four patients of the PD-MBI group scored 8, and 1 participant of PD-noMBI group scored 7. When we compared the group differences after excluding them, the main statistical results remained the same as for the full sample size. We briefly report those results but focus on the full group of 20 with PD-MBI and 40 with PD-noMBI all tables and figures in this article show results based on those groups.
Barriers And Facilitators To Overall Management
Physicians reported they manage apathy based on experience versus evidence, as there are currently no guidelines for care of apathy in PD . Furthermore, it was reported there is a lack of resources available pertaining to apathy treatment in PD . A lack of evidence concerning apathy was part of a larger issue identified overall there is limited information on neuropsychiatric symptoms of PD . This limits the capacity for HCP to provide treatment options to persons with PD .
Again, there are not many guidelines, I really like evidence based medicine and there are not good guidelines for this . The evidence is very poor. HCP P2
theres a remarkable amount of literature that sort of describes like the 10 cardinal symptoms of PD and you know, this is what PD is and this is what PD patients do. Theres a significant lack of attention to this whole complex of motivation, apathy, joy, reward if they havent been told that this could be a significant problem, theyre certainly lead astray PTC P3
probably not enough facilities, or not enough capacity for all allied health professionals to take on this problem HCP P4
We need a pathway of care that is focused on apathy, we need an algorithm of treatment that makes the approach more standardized and helps interaction with other health professionals. HCP P4
one quick way to try and improve it would be pharmacological. So, and I gauge their acceptance of adding on a medication of that type. HCP P4
Don’t Miss: Physical Therapy For Parkinson Disease Patients
Apathy In Parkinson’s Disease: More Than Just Executive Dysfunction
Published online by Cambridge University Press: 21 February 2013
- Saül Martínez-Horta
- Affiliation:Neurology Department, Movement Disorders Unit, Hospital de la Santa Creu i Sant Pau, Universitat Autònoma de Barcelona. Barcelona, SpainSant Pau Institute of Biomedical Research , Barcelona, Spain
- Javier Pagonabarraga
- Affiliation:Neurology Department, Movement Disorders Unit, Hospital de la Santa Creu i Sant Pau, Universitat Autònoma de Barcelona. Barcelona, SpainSant Pau Institute of Biomedical Research , Barcelona, Spain
- Ramón Fernández de Bobadilla
- Affiliation:Neurology Department, Movement Disorders Unit, Hospital de la Santa Creu i Sant Pau, Universitat Autònoma de Barcelona. Barcelona, SpainSant Pau Institute of Biomedical Research , Barcelona, Spain
- Carmen García-Sanchez
- Affiliation:Neurology Department, Movement Disorders Unit, Hospital de la Santa Creu i Sant Pau, Universitat Autònoma de Barcelona. Barcelona, Spain
- Jaime Kulisevsky*
- Affiliation:Neurology Department, Movement Disorders Unit, Hospital de la Santa Creu i Sant Pau, Universitat Autònoma de Barcelona. Barcelona, SpainSant Pau Institute of Biomedical Research , Barcelona, SpainCentro Investigación Biomedica en Red-Enfermedades Neurodegenerativas , Spain
- *
- Correspondence and reprint requests to: Jaime Kulisevsky, Movement Disorders Unit, Neurology Department, Sant Pau Hospital, Sant Antoni M. Claret 167,08025 Barcelona, Spain. E-mail:
Selection And Appraisal Of Documents
All study designs were included if they used a non-pharmacologic intervention to treat apathy in PD, either as a primary or secondary outcome, and were published in the English language. Initial treatment studies were identified by a previous scoping review on apathy in PD . Two authors independently screened titles and abstracts for the initial scoping search and the updated search . At the abstract stage, any abstract that discussed the treatment of apathy in PD was included. Two authors independently screened full text articles for the initial scoping search and the updated search . At the full text stage, any article that discussed the treatment of apathy in PD with a non-pharmacologic intervention was included.
The quality appraisal of included studies was adapted from Booth and colleagues , which takes into consideration whether included studies address the theory being tested and whether included studies support conclusions drawn by the researchers . Two authors assessed quality of data.
Read Also: What New In Parkinson Treatment
Tips To Stay Motivated
Keeping motivated is important for both the person with apathy and their caregivers. There can be social and emotional tolls on both. Following these tips can help both groups meet the challenges2,6:
- Get support– allow friends and family to help you maintain social and leisure activities and find renewed joy in life
- Follow a schedule that includes fun and enjoyable activities rewarding yourself for participation
- Set attainable goals for getting out of the house and doing fun things
- Exercise and get plenty of sleep. Activity is good for the motor symptoms of Parkinsons and will also make you more tired, helping to maintain a good sleep schedule.
Apathy can be frustrating for people with PD and those that care for them. Focus on achieving realistic steps along the way.2 The lack of motivation that is characteristic of apathy can be addressed by teamwork, trying to make things fun again. Examples of positive activities include cooking or dining out for a favorite meal, watching a movie, and pursuing enjoyable hobbies. Its important to remember apathy is a symptom of Parkinsons disease. The person with PD is not being intentionally difficult, lazy or making excuses.