Vocalizations As Part Of Stereotypies
The precise definition of stereotypies and their exact phenomenological distinction from other repetitive motor behaviors, for example, tics, is difficult. The term denotes a repetitive, often continuous, non-goal-directed movement pattern that is typically distractible. As with echolalic behaviors, stereotypies are also part of physiological development that often abate within the first years of life. Although the persistence of stereotypic vocalizations may still be part of normal development, in many cases it signifies pathology, and indeed stereotypic utterances are part of the diagnostic criteria of ASD . One large case series of 83 patients with Rett syndrome described phonic stereotypies with repetitive sounds, words, or phrases in only 6% of patients. We recently observed loud stereotypic vocalizations in a patient with 15q13.3 microdeletion syndrome and late-treated cases with phenylketonuria. Further, stereotypic vocalizations have been documented in patients with schizophrenia.
What About Natural Therapies And Supplements For Psp
Supplements and vitamins are another topic that is frequently asked about. Surprisingly little is known about these in relation to PSP. Much of what we know is derived from studies on Parkinson disease and may not actually translate to PSP. There is good data recently on coenzyme Q10 , a supplement that helps with energy production in cells and functions also as an antioxidant. Supplementing the energy of brain cells with CoQ10 is thought to help prevent further loss or degeneration, and may slow disease progression. In PSP there is evidence that CoQ10 indeed increases brain energy metabolism and, at least in the short-term, improves symptoms including cognitive function. CoQ10 is not a regulated drug and comes in many forms , resulting in differences in the dose need for effect. Speak to your doctor about recommended doses before taking, but generally 1200 mg/day is needed . As for other vitamins there again is limited data. Vitamin E has been touted as an antioxidant, but there is no good evidence for benefit in PSP and increasing data suggests that high doses may actually increase risk of death. Therefore, we do not recommend specific vitamin supplementation unless you are determined deficient by your doctor.
Vitamin D Insufficiency And Osteoporosis
There is evidence that several HKMDs, including Huntington disease, RLS, and tremor, are associated with low vitamin D serum levels. vitamin D deficiency, an essential factor for altered bone structure and increased fracture risk, was present in 89% of Chorea patients , and in 83% of RLS patients . We found reduced bone mineral density associated with vitamin D insufficiency in Huntington disease but not in RLS patients . For tic disorders, there is only one case report that describes a reduced bone mineral density in a patient with Tourette syndrome. However, the author attributed this pathology not to an altered vitamin D status but rather to neuroleptic-induced hyperprolactinemia .
Table 1
| 1000 IU p.o./d | no improvement |
RCT: randomized controlled trial SCCS: prospective self-controlled case study n.s.: not specified p.o.: per os i.m.: intra muscular /d: daily /w: weekly /m: monthly.
def. pts.: Vitamin D deficient patients.
However, the causal link to neurodegeneration is still a matter of debate, especially with regard to the effect of vitamin supplementation on disease progression . To date, as for HKMDs, real proof of clinical benefits are inconclusive . This highlights that there is a strong need for randomized clinical trials examining vitamin D supplementation in patients with neurodegenerative disorders with the focus to optimize time, efficacy, and appropriate dosing .
Don’t Miss: Early Signs Of Parkinson’s Disease Nhs
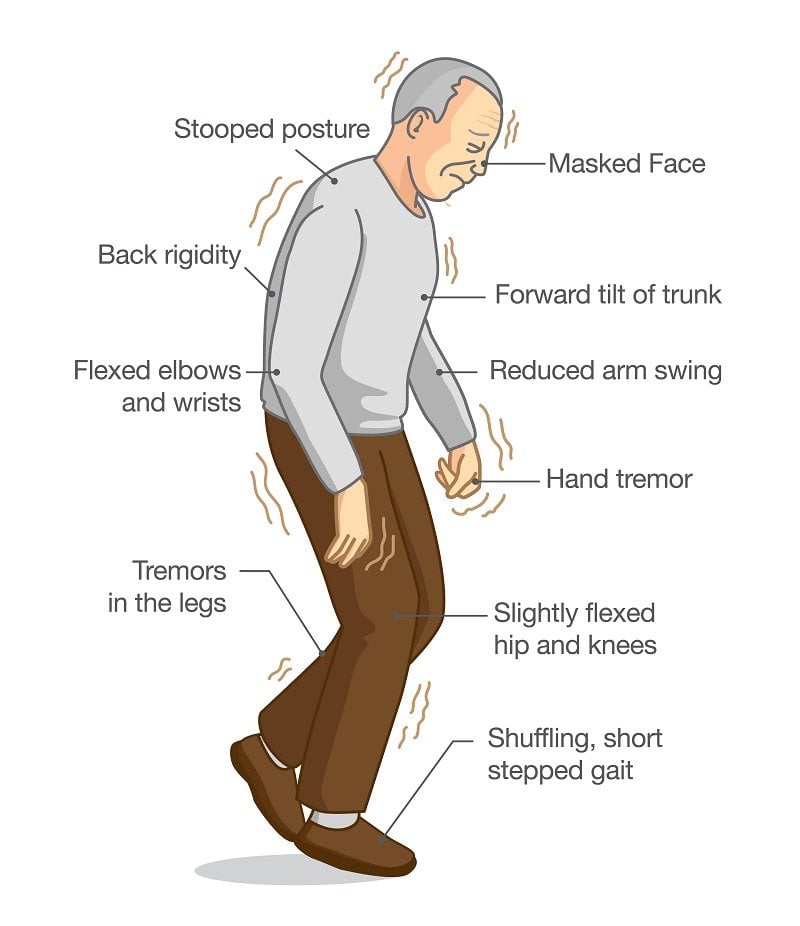
Stiffness And Slow Movement
Parkinsons disease mainly affects adults older than 60. You may feel stiff and a little slow to get going in the morning at this stage of your life. This is a completely normal development in many healthy people. The difference with PD is that the stiffness and slowness it causes dont go away as you get up and start your day.
Stiffness of the limbs and slow movement appear early on with PD. These symptoms are caused by the impairment of the neurons that control movement. A person with PD will notice jerkier motions and move in a more uncoordinated pattern than before. Eventually, a person may develop the characteristic shuffling gait.
Origins Of Breathing Disorders
The book by Leon Chaitow and co-authors cited above explains how breathing disorders are intrinsically linked to chronic stress and anxiety. The shallow, fast chest breathing through the mouth is a hallmark of the body preparing itself for the exertion of flight or fight due to a stress response. While this adaptive in acute stress situations, when stress is chronic and the body is spending a lot of time in fight or flight, the associated pattern of breathing becomes habitual, and eventually the system gets stuck in the new equilibrium of the CO2 intolerant state. However, the vicious circle work both ways, because overbreathing itself puts the body into a stress response state and feeds anxiety. A very good tutorial about the two way links between anxiety and breathing patterns is given by Robert Litman in the video below.
It is not surprising therefore that people with PD can present with disordered breathing associated with chronic stress and anxiety, since there are very significant overlaps between the other symptoms of chronic stress and those of Parkinsons Diseases, and ingrained fight or flight behaviours are common to the pre-diagnosis background histories of people with PD. Conversely, it is important to note that techniques which have been developed to treat breathing disorders should also help to decrease the symptoms of PD, including reduction of anxiety and increasing resilience to stress.
Recommended Reading: What Does Parkinson’s Disease Do
How Is Psp Diagnosed
Currently there are no tests or brain imaging techniques to definitively diagnose PSP. An initial diagnosis is based on the persons medical history and a physical and neurological exam. Identifying early gait problems, problems moving the eyes, speech and swallowing abnormalities, as well as ruling out other similar disorders is important. Diagnostic imaging may show shrinkage at the top of the brain stem and look at brain activity in known areas of degeneration.
Is There Any Treatment
There is currently no effective treatment for PSP and symptoms usually do not respond to medications.
- Parkinsons disease medications, such as ropinirole, rarely provide additional benefit. In some individuals, other antiparkinsonian medications, such as levodopa, can treat the slowness, stiffness, and balance problems associated with PSP, but the effect is usually minimal and short-lasting.
- Botulinum toxin, which can be injected into muscles around the eyes, can treat excessive eye closing.
- Some antidepressant drugs may offer some benefits beyond treating depression, such as pain relief and decreasing drooling.
Non-drug treatment for PSP can take many forms.
- Weighted walking aids can help individuals avoid falling backward.
- Bifocals or special glasses called prisms are sometimes prescribed for people with PSP to remedy the difficulty of looking down.
- Exercise supervised by a healthcare professional can keep joints limber but formal physical therapy has no proven benefit in PSP.
A gastrostomy may be necessary when there are swallowing disturbances or the definite risk of severe choking.
Deep brain stimulationwhich uses surgically implanted electrodes and a pacemaker-like medical device to deliver electrical stimulation to specific areas in the brain to block signals that cause the motor symptoms of several neurological disordersand other surgical procedures commonly used in individuals with Parkinson’s disease have not been proven effective in PSP.
Don’t Miss: Best Bed For Parkinson’s Patients
Awakened By The Sound Of A Melodic Hum
Minutes to midnight, I awake to the sound of a melodic hum. It is coming from my mother sitting in the dark living room, unaware of the hour. I turn on the light. With one hand on her cane and the other holding a little bundle in her lap, she is as charming as any little old lady can be.
I was going for a walk up the street, she offered, but I got tired and I sat down to rest.
Dead bolts on our doors do not prevent my mind from wandering through the what ifs. Eventually, my thoughts drift back to the hum. For me, it is probably the balm that keeps my anxieties in check but what is it for her?
My curiosity leads me to research whether there is any concern about the habit of humming in elderly people. There are a few surprises.
Box : Clinical Features Of Neuroacanthocytosis
-
A multisystem degenerative disorder of unknown aetiology.
-
Variable mode of inheritance.
-
Age of onset: approximately 30 years.
-
Chorea as well as orofacial-lingual dystonia are prominent.
-
Axonal neuropathy in 50% of cases.
-
Presence of acanthocytes on peripheral blood smears.
-
No curative treatment available treatment is largely supportive.
-
Relentlessly progressive .
Also Check: How To Care For Someone With Parkinson’s Disease
Causes And Risk Factors
Essential tremor occurs as the result of abnormal communication between certain areas of the brain. A genetic cause for essential tremor has been identified in 5070% of cases and, as a result, it has a strong tendency to run in families . While essential tremor can affect people of all ages, the average age of onset is 3545 years. The condition may get worse over time. It occurs equally in men and women, and can affect all ethnic groups.
Recently Fred Has Found His Eyes Are Closed Involuntarily Most Of The Time Though If He Makes An
You dont think, Oh, it would be nice to have my eyes closed now?
The mask that is the expressionless face, typical of many people with Parkinsons, probably distresses the people who have to live with it more than it embarrasses the person who has it. It tends to be the position the face falls into when not actively doing something else. Lack of facial expression can be hard for the family.
Don’t Miss: Gift Ideas For Parkinson Patients
Surgical Management Of Hyperkinesis
Some degree of synkinesis, hypokinesis, and hyperkinesis accompanies reinnervation of the face, whether nerve regeneration occurs with nerve grafting or nerve substitution techniques or with spontaneous recovery from a denervating injury. Synkinesis can be improved by sensorimotor re-education, in which the patient practices in front of a mirror, with the help of electromyography, to separate facial muscle activities.19,20 Hyperkinesis may be treated medically or surgically.21 Botulinum toxin injected into muscles involved in hyperkinesis causes temporary paralysis and temporary relief from hyperkinesis. When the effects of the botulinum toxin dissipate , injection can be repeated. Surgically selective neurolysis or regional myectomy can provide longer lasting treatment for hyperkinesis. Selective neurolysis involves weakening or paralyzing innervation to the hyperkinetic muscle. The results of neurolysis are difficult to predict, however, and hyperkinesis may return, even after excision of a segment of nerve. For these reasons, regional myectomy is the currently preferred surgical technique for management of hyperkinesis in patients who fail or who are unwilling to use botulinum toxin.
Adam W. Grasso, Sorin J. Brener, in, 2010
Rem Sleep Behavior Disorder
In vivid dreaming states most peoples bodies are still. However people with RBD lack muscle paralysis resulting in their acting out their dreams. This can include talking, screaming, shouting, hitting, punching or kicking, even propelling them out of bed. This can be scary and dangerous if they strike their partners or other bedside objects involuntarily. RBD is common in and can begin long before the onset of declining motor function. Fortunately it is also a very treatable condition.
Also Check: Nursing Home Care For Parkinson’s Patients
Pathophysiological Aspects Of Movement Disorders: A Link To Psychostimulants
Considerable overlap exists between the mechanisms influenced by psychostimulants and those involved in the pathophysiology of various movement disorders . Movement disorders affect the control of voluntary and involuntary movements and manifest as hypokinetic or hyperkinetic disorders including parkinsonism, tremor, dyskinesias, and myoclonus. Most of these disorders are either directly or indirectly related to the basal ganglia of the brain. Evidence of altered cortical function, white matter tract involvement and widespread neural network dysfunction is also becoming available.
Table 1. Examples of psychostimulants and an overview of their toxic effects mediated by monoaminergic systems.
Basal ganglia are a diverse group of interconnected nuclei that serve an important part in movement execution and the relay of the associated signals. The classical model proposes a direct and indirect pathway within basal ganglia involving subpopulations of striatal projection neurons . The circuits are activated by cortical signals and by regulating gamma aminobutyric acid release, they eventually exert an influence on dopamine-dependent signaling and thus increase or reduce locomotor activity. Selective contributions of these pathways have been verified in animals with dopamine- and cAMP-regulated phosphoprotein Mr 32 kDa loss in nigrostriatal neurons in reaction to cocaine .
Embarrassing Symptoms Of Parkinson’s Disease
Some symptoms that may occur in people with Parkinsons disease are not typical of it and so people noticing them may misunderstand them. These symptoms can be particularly embarrassing in social situations where other people witness their discomfort. They distress some people so much that they avoid company other than close friends or family. Most of these symptoms are caused by Parkinsons but some are side effects of the medicines used to treat it. All the symptoms tend to fluctuate in relation to the medication, and some people had learnt to adjust their medicine regime to minimise these effects.
Eating can cause embarrassment in several ways. Both tremor and dyskinesia affect the physical job of cutting up food and directing it into the mouth . Several people had a problem with a piece of steak or chicken that might fly off the plate as they tried to cut it up, or they had a choking fit if they unwisely took too big a piece into their mouth. Humphrey disliked eating out with friends because he tended to drop things.
You May Like: Parkinson Voice Project Loud Crowd
Equipment And Walking Aids
You might find that equipment can help you to walk, such as a walking stick or a rollator .
Before you start using a walking aid, it’s very important to get advice from a physiotherapist. Some walking aids aren’t recommended for people with Parkinsons as they can affect your walking pattern and make you more likely to fall. But, the correct walking aid can increase your confidence and help you to lift your feet better.
Physiologic Tremor And Enhanced Physiologic Tremor
Everyone has some small degree of tremor that may not be physically apparent but can be recorded electrophysiologically. This tremor is known as physiologic tremor. In some people this tremor can worsen in the setting of stress, anxiety or with stimulants such as caffeine and is known as enhanced physiologic tremor. Enhanced physiologic tremor is not a progressive disorder and needs no treatment.
You May Like: Exercise Class For Parkinson’s Disease
Legends To The Videos
Video 2. Vocalizations as part of stereotypies. Stereotypic vocalizations accompanied by motor stereotypies in a patient with autism spectrum disorder, before , during , and after treatment with botulinum toxin of the vocal cords. Stereotypic shouts accompanied by motor stereotypies in a patient with 15q13.3 microdeletion syndrome and cognitive disability, impulsivity, short stature, cachexia, and mitral valve insufficiency. The stereotypic behavior developed 4years earlier during a stressful period. The patient reported a soothing character of the repetitive shouts and movements, which reduced a feeling of inner distress. The behavior was distractible, although the patient felt that she was not able to suppress the movements and vocalizations.
Video 3. Vocalizations as part of chorea, dystonia, and other dyskinesias. Lip smacking in a patient with tardive dyskinesia. Panting and gasping in a patient with tardive dyskinesia due to chronic metoclopramide intake. Acute-onset hissing and shrieking in a patient with generalized choreodystonia subsequent to lenalidomide treatment for multiple myeloma.
Alzheimer’s Or Normal Aging
Just about everyone has minor memory glitches as they get older. If someone forgets a name or why they walked into the kitchen, that doesn’t mean they have Alzheimer’s.
The main problem that defines the disease is trouble planning and handling day-to-day tasks, like paying bills, managing a checkbook, or using familiar appliances around the house.
You May Like: Does Smoking Help Parkinson’s Disease
Ataxia / Dysmetria / Asynergia
Ataxia is an unsteady and swaying walk, often with feet planted widely apart. People have difficulty walking a straight line with their heel touching the toe of the shoe in front . Ataxia can occur in a number of neurologic conditions.
Dysmetria is misjudging the distance to a target. A person with dysmetria will have problems reaching out and accurately touching a targeted object.
Asynergia is a breakdown of movement, so that movements of the arms and legs become irregular and clumsy.
For more information, visit the National Ataxia Foundation website at www.ataxia.org.
What Are The Primary Motor Symptoms Of Parkinsons Disease
There are four primary motor symptoms of Parkinsons disease: tremor, rigidity, bradykinesia and postural instability . Observing two or more of these symptoms is the main way that physicians diagnose Parkinsons.
It is important to know that not all of these symptoms must be present for a diagnosis of Parkinsons disease to be considered. In fact, younger people may only notice one or two of these motor symptoms, especially in the early stages of the disease. Not everyone with Parkinsons disease has a tremor, nor is a tremor proof of Parkinsons. If you suspect Parkinsons, see a neurologist or movement disorders specialist.
Tremors
Rigidity
Bradykinesia
Postural Instability
Walking or Gait Difficulties
Dystonia
Vocal Symptoms
Also Check: Parkinson’s Loss Of Balance
What Is The Prognosis
The disease gets progressively worse, with people becoming severely disabled within three to five years of onset. Affected individuals are predisposed to serious complications such as pneumonia, choking, head injury, and fractures. The most common cause of death is pneumonia. With good attention to medical and nutritional needs, it is possible for individuals with PSP to live a decade or more after the first symptoms of the disease appear.