Parkinsons Disease Stem Cell Treatment
Parkinsons disease happens when there is a problem with certain nerve cells in the brain. This disease affects the way you move because of the inadequate production of dopamine, which is an important chemical that sends signals to the part of the brain that controls movement. Parkinsons is a progressive disease whose symptoms take a few years to surface.
Parkinsons is an illness that affects the central nervous system with a direct blow on the brain and spinal cord and usually only affects adults. More specifically, this disease damages a group of nerve cells in the deepest part of the brain called the Basal Ganglia. There are quite a few reasons leading to Parkinsons disease, including aging and poisons in the environment. To cure Parkinsons disease, stem cell treatment is highly popular.
These nerve cells make and use a brain chemical called dopamine to send messages to other parts of the brain to coordinate body movements. When someone suffers from Parkinsons disease, the dopamine levels are low. So, the body doesnt get the right messages required to move normally.
About 1 million people in the United States alone have Parkinsons, and both men and women can be affected by it. It usually affects the elderly population, someone older than 50, and it becomes common as people get older.
- Problems with balance or walking
Tremor, which essentially means shaking or trembling. Tremors may affect your hands, arms, or legs.
Ways To Reduce Parkinsons Freezing Of Gait
Do you sometimes feel like your feet are stuck to the floor or your hips are glued to your chair, despite your best efforts to move them?
This symptom, called freezing, has been seen in 30-67% of people diagnosed with Parkinsons, with a higher rate of incidence in later stages.
While everyone has unique freezing patterns, some common triggers include turning in tight spaces, walking through doorways, walking in narrow hallways or crowded places or changing walking surfaces .
As soon as you notice freezing symptoms creeping up on you, its important to address them so you can prevent them from worsening over time.
The first line of treatment is often dopaminergic medications that aim to keep you in an ON state for longer. However, evidence suggests there is a cognitive component of freezing that medication and deep brain stimulation do not address effectively.
This is why the best long-term treatment option for Parkinsons freezing is non-pharmaceutical, non-invasive and focuses on retraining your brain for success.
Here are six actions you can take to help minimize your freezing of gait.
Challenges In Fog Rehabilitation
Cognitive dysfunction in people with PD in general, and in people with PD+FoG specifically, can create challenges to rehabilitation. Some previous interventions aimed to improve FoG use compensatory strategies, such as providing external cues to trigger and guide movement and encouraging altered allocation of attention . Although this type of compensatory training often improves FoG, the cognitive dysfunction often observed in individuals with PD+FoG may limit their ability to deploy such strategies in daily life. Indeed, recent results suggest that, when cues are removed, people with PD+FoG revert to dysfunctional movement more than people with PDFoG., Alternatively, attempts to improve the underlying dysfunction may be able to reduce the cognitive limitations of this population. For example, training individuals to take larger, more consistent steps may partially circumvent attentional cues such as lines or tones . However, this approach relies, in part, on implicit motor learning, which has been shown to be deficient in people with PD+FoG. Due to the drawbacks of both treatment approaches, we believe that incorporating both restitutive and compensatory approaches will provide the greatest chance of cognitive-motor improvements. Therefore, we have incorporated each of these approaches into the current framework.
Don’t Miss: Gift Ideas For Parkinson Patients
Freezing Of Gait In Parkinson’s Disease
This short webpage explains what freezing of gait is, why it occurs, and treatment. It also offers 10 tips to prevent freezing or get ‘unstuck.’ Finally, there is a discussion of walkers that can prevent injury due to falls when freezing episodes are severe and the future of treatments for freezing of gait.
What Is Freezing Of Gait
Freezing of gait is an abnormal gait pattern that can accompany Parkinsons disease as well as other parkinsonian disorders in which there are sudden, short and temporary episodes of an inability to move the feet forward despite the intention to walk. In a sense, youre stuck. This results in the characteristic appearance of the feet making quick stepping movements in place. However, while the feet remain in place, the torso still has forward momentum which makes falls unfortunately common in the context of freezing of gait. For some, these episodes can simply be frustrating, annoying and perhaps embarrassing for others freezing of gait can become incredibly disabling and lead to injury.
Freezing of gait episodes tend to occur least often when walking on an unobstructed, straight path. Any deviation from that can induce freezing for example, when you first try to start walking, when you go to make a turn, or try to navigate around obstacles or through narrow spaces any of these can cause you to get stuck.
The particular triggers for one person may be different than for another. An episode is typically very brief, often lasting only 1-2 seconds, although they can last longer. Freezing of gait can be affected by anxiety, so if a person feels rushed , freezing may be particularly prominent.
Don’t Miss: Is Memory Loss A Symptom Of Parkinson’s
Coping With Freezing In Parkinson’s Disease
Claudia Chaves, MD, is board-certified in cerebrovascular disease and neurology with a subspecialty certification in vascular neurology.
Around half of people who have Parkinson’s disease experience freezinga temporary inability to move that occurs suddenly and without warning. Such episodes are short-lived, lasting from a few seconds to up to several minutes.
Parkinson’s freezing can affect nearly any part of the body and disrupt nearly any activitychewing for example, or writing. However, it most often occurs when someone is walking, causing them to feel as if their feet are glued to the ground even though the upper part of their body is still mobile. This sometimes is referred to as freezing of gait and can have repercussions ranging from a brief disruption in stride to an increased risk of falling that can lead to broken bones and other injuries.
The exact physiological cause of freezing in Parkinson’s has yet to be determined. What is known is that it’s often associated with lulls in the effectiveness of medication, particularly among people who have mid-to-late stage disease. There also are a number of common triggers of freezing while walking, such as changing direction, approaching a doorway, or navigating a crowded area. Although Parkinson’s freezing can have a negative impact on a person’s quality of life, there are simple and effective ways to manage it.
Understanding The Science Behind Neurobiomedicine And Our Approach To Helping You Restore Proper Function To Ultimately Help You Feel Better Look Better And Recover Your Health
Dr. Farleys Neurobiomedicine Health System can easily be understood when applied to the science of Translational Medicine, Psychosomatic Medicine and Somatopsychic Medicine as described from the National Institutes of Health. Please to learn more about Translational Medicine, Psychosomatic Medicine, Somatopsychic Medicine. Allopathic Medicine and even Integrative Medicine asks, Whats the diagnosis. Neuro-Biomedicine asks, Why you are personally having this happen?, and, What are your specific multifactorial causes?
Most doctors offices rely on outdated protocols that are 17-20 years behind the basic scientific research. The reason for this is lack of initiative by most doctors, and for medical legal reasons, they will not deviate from typical protocols even when they are outdated and produce terrible results for patients. The focus is not on the individual patient and their unique requirements, instead, the patient is literally pushed from office to office with the goal to just move the responsibility to another doctor or office . We do not treat any disease, instead we focus on your functional neuro-metabolic deficits. We will fight for you and your health! We will provide new possibilities and potential for greater healABILITY, greater depth of understanding, more compassionate listening, and ultimately, superior results aimed at restoring proper function. This, in turn, can have profound and positive improvements for the patients that qualify.
Read Also: Pedaling For Parkinson’s Colorado
Box 1 Three Conceptual Categories Of Training Interventions As Based On Their Relevance To Fog
FOG-specific
Exercise or training-based interventions aimed directly at alleviating imminent FOG episodes or better prepare patients for upcoming FOG while the interventions are applied, and possibly in times beyond. This includes mixed intervention studies, of which at least one training component is directly aimed at reducing FOG episodes or circumventing FOG-provoking circumstances. Examples are: cueing offered to help patients overcome FOG episodes action-observation training strategies designed to relieve FOG in FOG-provoking situations and fall-prevention training including strategies to overcome imminent FOG episodes, such as through the use of cueing. FOG was assessed as a primary or other outcome in these studies.
FOG-relevant
Exercise or training-based interventions aimed at training the motor- and/or non-motor correlates of FOG with the aim to reduce the severity or amount of FOG following the intervention, but not aimed at the immediate alleviation of imminent FOG episodes or circumventing FOG-provoking circumstances while the intervention was applied. Examples are cognitive training cognitive-motor dual-task training balance training curved treadmill training regular treadmill training with cueing that was aimed at improving gait parameters other than FOG and obstacle avoidance training. FOG was assessed as a primary or other outcome in these studies.
Transcranial Direct Current Stimulation
In general, anodal tDCS facilitates cortical excitability. In a crossover, double-blind, randomized, sham-controlled study including 10 PD patients with levodopa-resistant FOG, five sessions of 2mA anodal tDCS on primary motor cortex showed benefits on FOG and motor performance after tDCS . However, another crossover double-blind, randomized, sham-controlled study applied one session multibipolar tDCS electrodes stimulating only primary motor cortex in PD patients with FOG didnt improve FOG. But after stimulating both primary motor cortex and left dorsolateral prefrontal cortex, the performance in gait-provoking test, stroop, and time up and go tests were improved . Besides, another double-blinded crossover randomized, sham-controlled study including 10 PD with FOG showed a single dose of anodal tDCS over the SMAs did not improve self-initiated gait in PD and FOG .
Don’t Miss: Does Parkinson’s Disease Cause Dizziness
Treating Freezing Of Gait For People With Parkinsons
Freezing of gait episodes often occur when a person is under-medicated and can improve with increased amounts of their PD meds, usually carbidopa/levodopa. However, as mentioned earlier, the brain abnormalities that lead to freezing of gait are very complex, so giving more dopaminergic medication is only part of the solution. In fact, some people have what is referred to as ON freezing. This means that freezing of gait episodes occur even when other PD symptoms are well treated with their medication regimen.
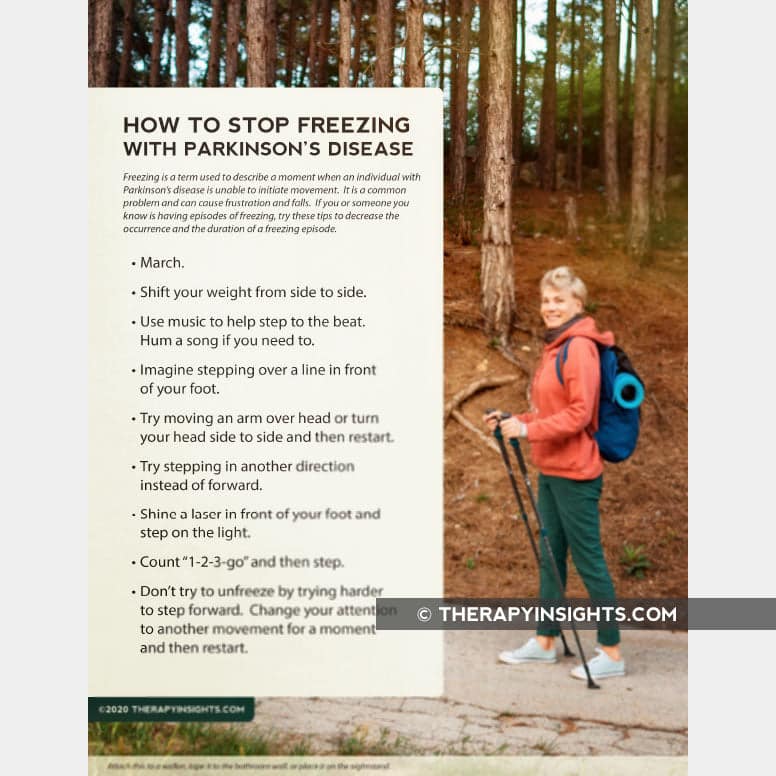
Cueing, or the introduction of an external sensory stimulus to facilitate movement, has been identified as a way to break a freezing episode. Terry Ellis, PhD, PT, NCS, Director of the APDA National Rehabilitation Resource Center at Boston University, and Tami DeAngelis, PT, GCS, compiled this list of cues that can be used to get out of a freezing episode:
What Can Help You Get Unfrozen
There are several tricks you can learn to help you become “unfrozen” when you have a freezing episode from Parkinson’s disease.
- Step toward a specific target on the ground.
Some people use handheld laser pointers to create a target.
- Place a cane or walking stick on the floor in front of you and then step over it.
You can also have someone else place it in front of you.
- Make your first step a precise, stiff-legged, marching-type step, with a long stride.
These or other techniques may help you overcome freezing and get moving again. Specially trained dogs and special devices are available that can help you if freezing is a severe or frequent problem.
Don’t Miss: What Are Some Signs Of Parkinson’s Disease
Is Freezing Related To The Intake Of Dopaminergic Medication
Some people with Parkinsons have on and off periods, when they switch from being able to move when their medication level is higher to being unable to move without difficulty when their medication level is low . Many people notice that freezing is worse when their medication level is low, when they are off. But freezing is not the same as being on or off.
What Causes Freezing Of Gait In Parkinsons
There are significant differences between people with Parkinsons who experience freezing of gait and those who dont. However, there are some commonalities that may help to explain why some people with Parkinsons disease develop this symptom while others dont.
One theory is that freezing of gait occurs when certain brain areas are unable to properly process information from the body regarding movement. This can be due to damage to the parts of the brain that control movement, or it may be due to changes in the way that information is transmitted between the different parts of the brain.
Another theory is that freezing of gait may be a result of an imbalance in the neurotransmitters in the brain. Neurotransmitters are chemicals that help to transmit signals between the different parts of the brain. If there is an imbalance in the neurotransmitters, it can lead to problems with movement.
Yet, another theory involves the contribution that step length has to FOG.
Freezing of gait has been identified as one of the main contributors to gait disturbances in Parkinsons disease. While the pathophysiology remains enigmatic, several factors such as step length and the sequence effect may lead to the occurrence of FOG.
Recommended Reading: How To Find Out If You Have Parkinson’s
Identify Your Triggers And Retrain Your Brain
Your therapist will evaluate your unique triggers and symptoms and guide you through an exercise program that incorporates cognitive challenges and physical training. This will help retrain your brain to use more effective walking patterns and reduce freezing episodes.
Those with more intense freezing symptoms may benefit from short anti-freezing intensives, like the one they offer at the PWR!Gym in Arizona.
In addition to working with a Parkinsons physical therapist, here are five more general strategies you can try to help avoid a freezing episode.
What Causes Freezing In Parkinsons
Although the precise origin of freezing is unknown, experts believe it has something to do with cognitive issues and the intricate brain circuitry needed for movement. Another common cause of walking-related freezing is changing direction, moving closer to a doorway, or moving through a crowded space. For instance, walking calls for several connections between various brain regions, such as:
- Regions of the frontal lobe of the brain that control and begin movement
- Sections of the brainstem that regulate movement and wakefulness regions of the basal
- Ganglia where dopaminergic neurons that fine-tune and govern movement are found
Parkinsons disease patients brain connections appear to short-circuit at one or more locations. Individual differences may exist in the specific anomalies that give rise to the issue.
Also Check: What Are The Stages Of Parkinson Dementia
Walking Freezing And Falling
The dopamine in your brain is heavily involved in controlling the movement of your body. In Parkinsons, there are reduced levels of dopamine. For this reason the most obvious changes related to Parkinsons are normally those that affect your movement, including walking, falling, and freezing.
In particular, slowed movement, stiff muscles and changes to posture affect all people living with Parkinsons. These issues and others can lead to challenges with walking, freezing and falling.
What Does Freezing In Parkinsons Look Like
The primary symptom of freezing of gait is an inability to take a step, even when there is a strong desire to do so.
This can happen when starting to walk or when turning around. Freezing episodes can last for a few seconds or minutes, and may be accompanied by a feeling of uncertainty or anxiety.
Its very easy to see or even imagine what this looks like. Imagine youre at a football game. The crowd is roaring and you want to stand up to get a better view. But your legs just wont move.
You try to take a step, but your feet feel like theyre glued to the ground. Thats what freezing of gait can feel like.
The basic science is that the message to move from the brain simply does not get to the muscles that are needed to make the motion happen.
Walking demands a complex and balanced recruitment of neuronal systems requiring attention, afferent information processing and intentional adjustments . The motor cortex, midbrain, hindbrain, and basal ganglia are all involved in the decision making and planning of locomotion.
Its as if your brain is saying Get up! or Take a step! but your body isnt getting the message. How annoying is that?!!
Heres a video showing you what this exactly looks like:
Its easy to see how this symptom can impede the persons ability to walk and get around. So much so that they may require the physical assistance of someone to help them.
You May Like: Can Dogs Get Parkinson’s
Risk Factors For Developing Fog
This review included the prospective studies that followed early-stage PD patients over time and the retrospective studies that clearly recorded the clinical manifestation prior to FOG onset. Many studies identified FOG related motor and non-motor symptoms by utilizing cross-section data to compare the clinical symptoms between freezers and non-freezers. Those studies were excluded as they cannot differentiate the symptoms prior to FOG from the accompanying symptoms of FOG. A total of 11 longitudinal follow-up studies were reviewed and summarized . For these studies, cox proportional-hazards regression analyses or logistic regression analysis were performed to identify the factors predictive of FOG except one study that used generalized estimating equations . Here, we elaborated the risk factors including demographic information, motor symptoms, non-motor symptoms, neuroimaging, fluid parameters, and medication use. Current limitations and recommendations for future researches will also be discussed. A list of the evidence supporting and refuting the following variables as risk factors of FOG was provided in Table .
Table 1 A detail summary of risk factors for FOG development in Parkinsons disease