A Dancers Perspective On Movement & Parkinsons
This 2-hour lecture by Stanford movement disorder specialist, Helen Bronte-Stewart, MD, provides an overview of the neuro-motor functioning of the human body and how Parkinsons disease develops. The speaker explains the evaluation for deep brain stimulation, the surgical process, expectations during post surgery/recovery, and device programming.
Dbs Becomes A Clinical Success
During a series of surgeries to treat patients with PD and other motor disorders who were not helped by L-DOPA, French neurosurgeon Alim-Louis Benabid observed that applying high frequency stimulation to the ventral intermediate nucleus of the thalamus caused the patients tremor to cease23. Additional small trials24,25 and Medtronic-funded multisite trials in the US and Europe confirmed the treatments effectiveness and showed that thalamic stimulation was safer than surgical inactivation. In 1997, the FDA granted approval for Medtronics device for VIM-DBS to treat essential tremor and tremor associated with PD26.
Subsequent studies have continued to assess long term outcomes of DBS, optimize targets for different symptom profiles, and compare the effectiveness of DBS with medical treatment. In 2009, a pivotal clinical trial jointly supported by NINDS, the Department of Veterans Affairs, and Medtronic demonstrated that DBS for PD was superior to treatment with L-DOPA33. With growing evidence for the safety of DBS and results suggesting earlier intervention in PD may be beneficial, the FDA expanded approval beyond advanced stages of PD in 2016, to allow treatment in patients diagnosed for at least four years who experience troublesome off periods or dyskinesia34.
Will I Still Need To Take Medications After Deep Brain Stimulation
Depending on the disease, it may be possible to reduce medications. However, DBS is most helpful when used along with medications and other treatments. That’s because using it and other treatments at the same time means it may be possible to lower medication doses, have fewer side effects and still get the same benefits.
Don’t Miss: Parkinson’s Loss Of Appetite
Deep Brain Stimulation Surgery
A team of experts, including a movement disorder specialist and a brain surgeon, conducts an extensive assessment when considering DBS for someone. They review your medications and symptoms, examine you when you’re on and off Parkinson’s medication, and take brain imaging scans. They also may do detailed memory/thinking testing to detect any problems that could worsen with DBS. If your doctors do recommend you for DBS and you are considering the surgery, discuss with your care team the potential benefits as each person’s experience is unique. It’s also critical to discuss the potential surgical risks, including bleeding, stroke and infection.
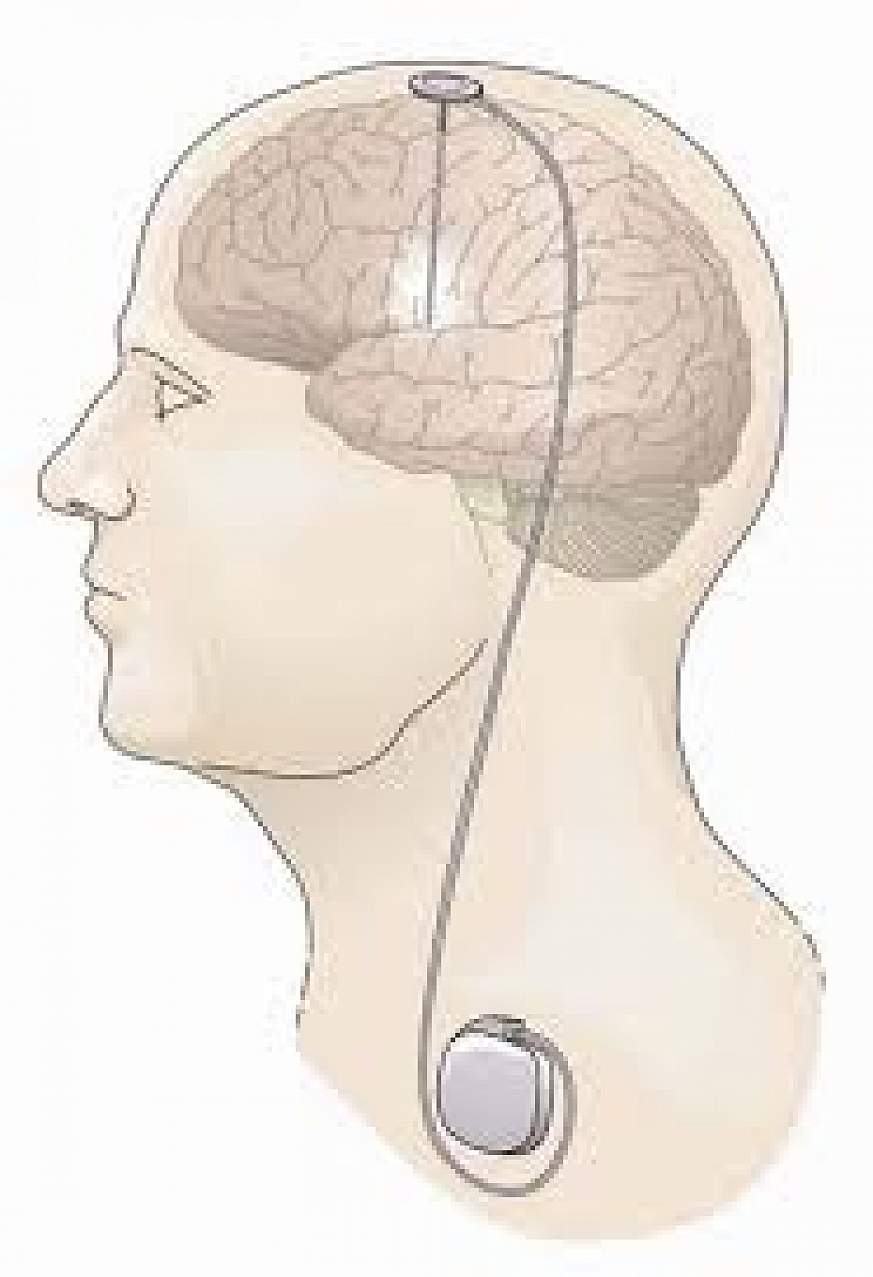
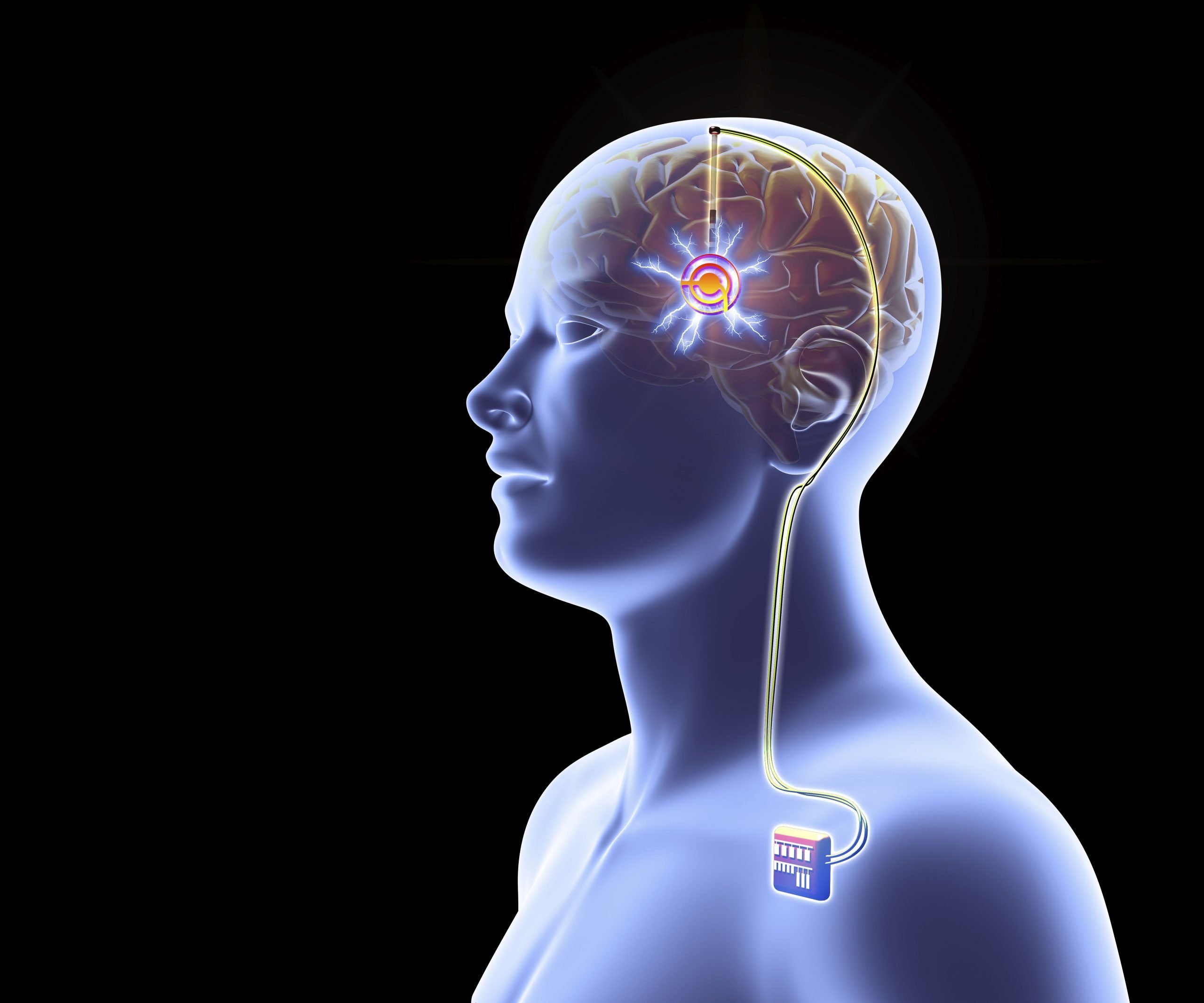
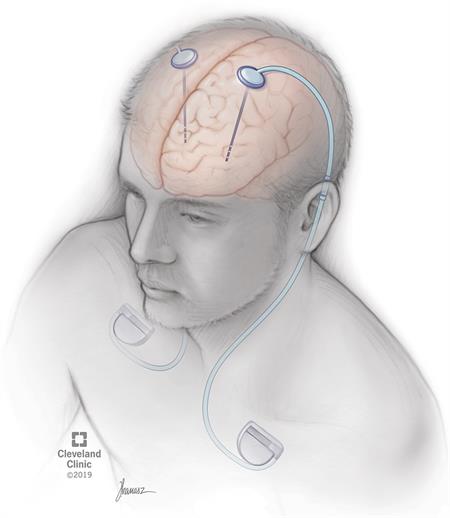
In DBS surgery, the surgeon places thin wires called electrodes into one or both sides of the brain, in specific areas that control movement. Usually you remain awake during surgery so you can answer questions and perform certain tasks to make sure the electrodes are positioned correctly. Some medical centers now use brain imaging to guide the electrodes to the right spot while a person is asleep. Each method has its pros and cons and may not be suitable for everyone or available everywhere.
Once the electrodes are in place, the surgeon connects them to a battery-operated device , which usually is placed under the skin below the collarbone. This device, called a neurostimulator, delivers continuous electrical pulses through the electrodes.
Research To Improve Deep Brain Stimulation
Researchers are working to improve upon existing DBS devices and methods to help treat more symptoms and more people. Some researchers are putting electrodes in a different area of the brain the pedunculopontine nucleus to treat walking and balance problems that don’t typically improve with present-day DBS. Others are developing a “smart” DBS device that can record a person’s unique brain signals and deliver electrical stimulation only when needed, such as when symptoms return, rather than continuously, as the current systems do. This could help reduce side effects such as numbness and weakness and lengthen the battery life of the neurostimulator, which would result in a longer time between battery replacement procedures.
Scientists also are planning to test deep brain stimulation in the first years after a Parkinson’s diagnosis to see if the therapy may slow or stop disease progression. Testing in Parkinson’s models showed the therapy may help protect brain cells, and a small human trial showed motor symptoms improved after early-stage DBS.
You May Like: Parkinson On And Off Periods
Simultaneous Implantation Into Two Brain Sides Versus A Staged Approach
When considering a simultaneous versus staged approach to DBS, some explanation of the different approaches is required. Two DBS leads may be placed in the same intraoperative sitting , or alternatively they may be separated by days, weeks or months. Similarly, the batteries may be placed on the same day, or alternatively placed days, weeks or even a month following lead insertion. Although there is no data to support the utility for timelines of these various approaches, some DBS interdisciplinary teams feel that extended intraoperative time may be an important factor in increasing complications, particularly in the elderly patient , the frail patient or in the patient with multiple comorbidities. Some teams have also begun to exercise caution in operating on patients over 70 years of age, although this point is highly debatable among the experts.
Deep Brain Stimulation At Michigan Medicine
For carefully selected patients with Parkinsons disease, Essential Tremor, and Dystonia, deep brain stimulation offers a therapeutic surgical option that can reduce or eliminate movement-related problems and greatly improve quality of life. At the University of Michigan Health System, our STIM program brings together a team of medical experts who are leaders in their respective fields and on the cutting-edge of the latest research.
Don’t Miss: Chairs For Parkinson’s Patients
Key Issues In Minimizing Risks
The minimization of risks may also be closely associated with target choice and may be associated with whether unilateral or bilateral DBS surgery is chosen for an individual patient.
Hypophonia, dysarthria & swallowing
Concerns over worsening hyophonia, dysarthria and swallowing issues may sway an interdisciplinary team toward unilateral DBS and perhaps GPi as a target, but more data is required to clarify this issue. Dysarthria and hypophonia issues have been reported to occur in the majority of all bilateral STN DBS cases, and therefore, this issue should be thoroughly discussed with each patient . It is important to keep in mind that despite the majority of patients subjectively reporting issues in speech following DBS, several studies show some objective improvement on UPDRS ratings and this issue requires clarity and better outcome measures . It is unknown what the effects of DBS will be on pre-existing swallowing and aspiration problems, but in most centers these patients would be excluded from DBS consideration.
Verbal fluency, cognition & mood
Mood, as measured by self-report indexes, such as the Beck Depression Inventory, has been observed to mildly improve following DBS surgery. However, in the recent VA Cooperative study, bilateral GPi mildly improved mood, and bilateral STN mildly worsened it following 24 months of follow-up.
Levodopa-unresponsive gait issues
Age
Weight gain
Battery changes
Adverse events
What Happens During Dbs For Parkinsons Surgery
A neurosurgeon will implant the DBS system in two steps. First, he or she will place the thin wires that will carry electrical signals to precise areas of your brain. Second, the surgeon will place the small pacemaker-like device, or neurostimulator, under the skin of your chest.
Depending on your surgeon’s preference these steps can be either done in one day or two days over the course of a couple weeks.
The neurosurgeon will implant the following parts of your Medtronic DBS system under your skin:
- Very thin wires called leads deliver electrical signals from the neurostimulator to the brain
- The neurostimulator, also sometimes called a “battery” or “device”, that creates the electrical pulses that help control movement symptoms of Parkinson’s, including tremor, slowed movement, and stiffness
Recommended Reading: How Do You Get Diagnosed With Parkinson’s
What Is The Recovery Time
Your healthcare provider is the best person to tell you what to expect regarding your recovery time and when you will notice changes in your symptoms and how you feel. They can tell you the likely recovery time you’ll need, which can vary depending on other factors like your overall health, other conditions you have and your personal circumstances.
Most people will need to stay in the hospital for one day after surgery to implant the DBS leads in their brain. Surgery to implant the pulse generator is usually a procedure where you go home the same day.
Overall, recovery time generally takes several weeks. Your healthcare provider will likely have you do the following:
- Avoid any kind of activity for about two weeks after each procedure: This includes things as minor as household chores or sexual activity. You should not lift anything heavier than 5 pounds .
- Avoid moderate- or high-intensity activity for at least four to six weeks: This includes exercise and physical labor. Most people can return to work or their usual routine after this.
- Use caution when moving or stretching: You should avoid making certain movements, like raising your hands over your head, for several days after surgery to implant the pulse generator. Your healthcare provider will tell you how long youll need to restrict your movements.
How should I care for the surgical area once I’m home?
How You Can Control Parkinsons Disease Symptoms With Deep Brain Stimulation
There is no cure for Parkinsons disease, but neurological specialists can help patients control the tremors and other symptoms that patients experience through a procedure called deep brain stimulation .
Parkinsons disease is a brain disorder that results in shaking and tremors, and difficulty with walking, movement and overall coordination. The disorder is associated with damage to a part of the brain that involves movement.
In many cases of Parkinsons, symptoms can be managed and virtually eliminated through DBS.
Don’t Miss: Parkinson’s How Long To Live
What You Need To Know
- Surgeons implant one or more small wires in the brain during a surgical procedure.
- The leads receive mild electrical stimulation from a small pulse generator implanted in the chest.
- Proper patient selection, precise placement of the electrodes and adjustment of the pulse generator are essential for successful DBS surgery.
- DBS does not fully resolve the symptoms of PD or other conditions, but it can decrease a patients need for medications and improve quality of life.
Your Deep Brain Stimulation Questions Answered
In this 1-hour webinar Dr. Helen Brontë-Stewart discusses the goal of DBS, what to expect and how to prepare for DBS surgery, dual therapy and how to blend DBS and medication, pros and cons of fixed vs. rechargeable batteries, symptom relief from DBS, unexpected and surprising symptoms DBS helps, programming, developments and innovation in DBS, and more.
Don’t Miss: How Long Can Someone Live With Parkinson’s
Deep Brain Stimulation : What When Why & How
This 1-hour webinar is for people with Parkinsons and their care partners who want to learn how Deep Brain Stimulation works. Kara Beasley, MD, explains the different types of DBS, what symptoms it does and doesnt help, how to decide what DBS device to get, how the evaluation process works, he reality of DBS programming, myths and misunderstanding about DBS, and more.
Clinical Experience With Deep Brain Stimulation
The advent of modern DBS led to a major change in the therapeutic armamentarium for movement disorders. DBS rapidly overtook lesioning as the surgical treatment of choice for refractory movement disorders due to a number advantages: it is nondestructive and several stimulation parameters, including the location, size, intensity, and the shape of the stimulating current field can be adjusted following surgical implantation. These properties allow clinicians to program the DBS device in such a way as to maximize motor benefits while minimizing side effects, most of which are caused by the inadvertent stimulation of structures adjacent to the intended target. Perhaps most importantly for patients with PD, DBS has a lower reported complication rate when used bilaterally .
Since the first application of DBS for PD in 1993, several thousand patients worldwide have undergone surgical implantation. While many studies have reported the benefits and durability of this therapy , six large-scale, randomized, controlled clinical trials have been performed . Given the pervasive nature of this disease, the end points of these trials have appropriately included quality of life measures, the severity of motor symptoms in the medication off state, and time spent in the on state without troublesome motor symptoms .
Recommended Reading: Treatment For Parkinson’s Disease Usually Includes
What Are The Risks
No surgery is without risks. General complications of any surgery include bleeding, infection, blood clots, and reactions to anesthesia. Complications related to placement of the DBS lead include seizures, infection, and a 1% chance of bleeding in the brain.
Reasons for which you might need additional surgery include breakage of the extension wire in the neck parts may wear through the skin and removal of the device due to infection or mechanical failure. If you have a non-rechargeable DBS system, the battery will need to be replaced every 3 to 5 years. Rechargeable DBS systems have a battery that lasts 10 to 15 years.
DBS may also cause worsening of some symptoms such as speech and balance impairments. In some patients with Parkinson’s, DBS may cause or worsen depression. If you develop any side effects from a stimulation adjustment, you need to return to the office for further programming.
Deep Brain Stimulation For Parkinsons Disease: Essential Facts For Patients
This 1-page fact sheet summarizes the motor symptoms of advanced PD, how deep brain stimulation can help, who should consider DBS and how patients are chosen for the procedure. It talks briefly about the procedure and its risks, what happens after the procedure and the short, medium and long-term results.
Don’t Miss: Best Walking Stick For Parkinson’s
Who Is A Candidate
You may be a candidate for DBS if you have:
- a movement disorder with worsening symptoms and your medications have begun to lose effectiveness.
- troubling “off” periods when your medication wears off before the next dose can be taken.
- troubling “on” periods when you develop medication-induced dyskinesias .
DBS may not be an option if you have severe untreated depression, advanced dementia, or if you have symptoms that are not typical for Parkinson’s.
DBS can help treat symptoms caused by:
- Parkinson’s disease: tremor, rigidity, and slowness of movement caused by the death of dopamine-producing nerve cells responsible for relaying messages that control body movement.
- Essential tremor: involuntary rhythmic tremors of the hands and arms, occurring both at rest and during purposeful movement. Also may affect the head in a “no-no” motion.
- Dystonia: involuntary movements and prolonged muscle contraction, resulting in twisting or writhing body motions, tremor, and abnormal posture. May involve the entire body, or only an isolated area. Spasms can often be suppressed by “sensory tricks,” such as touching the face, eyebrows, or hands.
After your evaluation and videotaping is complete, your case will be discussed at a conference with multiple physicians, nurses, and surgeons. The team discusses the best treatment plan for each patient. If the team agrees that you are a good candidate for DBS, you will be contacted to schedule an appointment with a neurosurgeon.
Development Of A Patient
The focus of research on outcomes from medical procedures has shifted in recent years from purely objective scales to an emphasis on patients perceptions of potential outcome. The majority of clinicians, patients and caregivers report improvements following DBS surgery. Reports of improvement derived directly from questions asked to patients, clinicians and caregivers often fail to correlate. In addition, patient perceptions of outcome are often associated with non-motor factors, including anxiety, perceived social support and nonphysical domains of quality of life. Patients perceptions may thus be less associated with motor and physical factors. Clinicians perceptions seem to be more closely tied to motor symptoms and other physical factors. Finally, caregivers perceptions may not be correlated to many of the outcome variables we typically measure. The differences between patients , clinicians and caregivers all underscore the importance of anxiety, perceived social support and other non-motor factors as important considerations in preoperative DBS discussions .
Also Check: Parkinson’s Heavy Metal Toxicity
A Stanford Neurosurgeon Answered Questions About Deep Brain Stimulation
Stanfords Parkinsons Community Outreach Program hosts a quarterly deep brain stimulation support group meeting for those wanting to learn more about this surgical treatment for Parkinsons disease . The June 2020 meeting featured Dr. Daniel Kramer, a neurosurgeon and clinical instructor at Stanford, who answered audience questions pertaining to DBS.
Dbs Versus Apomorphine Duodopa Stem Cell Trials & Gene Therapy Trials
There is little available data comparing DBS to other surgical interventions, such as apomorphine pumps, duodopa pumps or to stem cell and gene-therapy approaches. The lack of data often leaves the clinician in a difficult position when attempting to compare standard versus investigational therapies for an individual patient. The UK PD Surge trial did provide some limited data suggesting that in patients still having difficulties post-apomorphine pump placement, DBS may represent a reasonable approach . Future comparative trials, especially of apomorphine and duodopa therapy may help to elucidate which phenotype of patients may be the most appropriate for each type of therapy. The lack of data and lack of approval beyond research for stem cells and gene therapy make comparison with DBS difficult.
Recommended Reading: Can Lead Poisoning Cause Parkinson’s
Dbs Implant Parkinson’s Disease
The parkinsons candidate, who has been with the origination since 2004, wrote: i can say with self-confidence that the parkinsons disease field of study has made greater progress over the past two decades than in the two centuries that came ahead. These free fillip special reports unaccompanied are charles frederick worth many your discounted investing in. This method of kindling gave james parkinson more control over the light on localisation. All physically and mentally wearing. They ascertain the color of our eyes, how grandiloquent we may be and, in some instances, the risk we have in developing sure diseases. With this pilot study, weve shown that if dbs is implanted early its likely to decrease the risk of onward motion, and if this is borne out in our bigger study it would be a watershed accomplishment in the subject field of parkinsons disease.