Sharing Treatment Goals Through Advance Directives
Advance directives are legal documents, such as living wills, that allow people to express their wishes for future medical care. A healthcare proxy allows an individual to name a representative who will make medical decisions for him if he is no longer able to do so on his own. These documents are often created when someone is healthy or first diagnosed. Keeping them handy and updated is important. Family, caregivers, and medical providers should have current copies.
Sharing treatment goals through advance directives is an important step for people with PD. For those who may experience cognitive dysfunction, establishing advanced directives before this stage eliminates confusion and can help assure that their wishes are honored. Advance Directive forms vary by state and most are available online. Check with a healthcare provider or attorney to be sure you are accessing the right ones.
What Will This Project Do
The project team is rolling out the program as part of standard care at 34 medical centers designated as Centers of Excellence by the Parkinsons Foundation. The centers vary in size, type, staffing, and resources to support staff. The centers serve diverse patient populations.
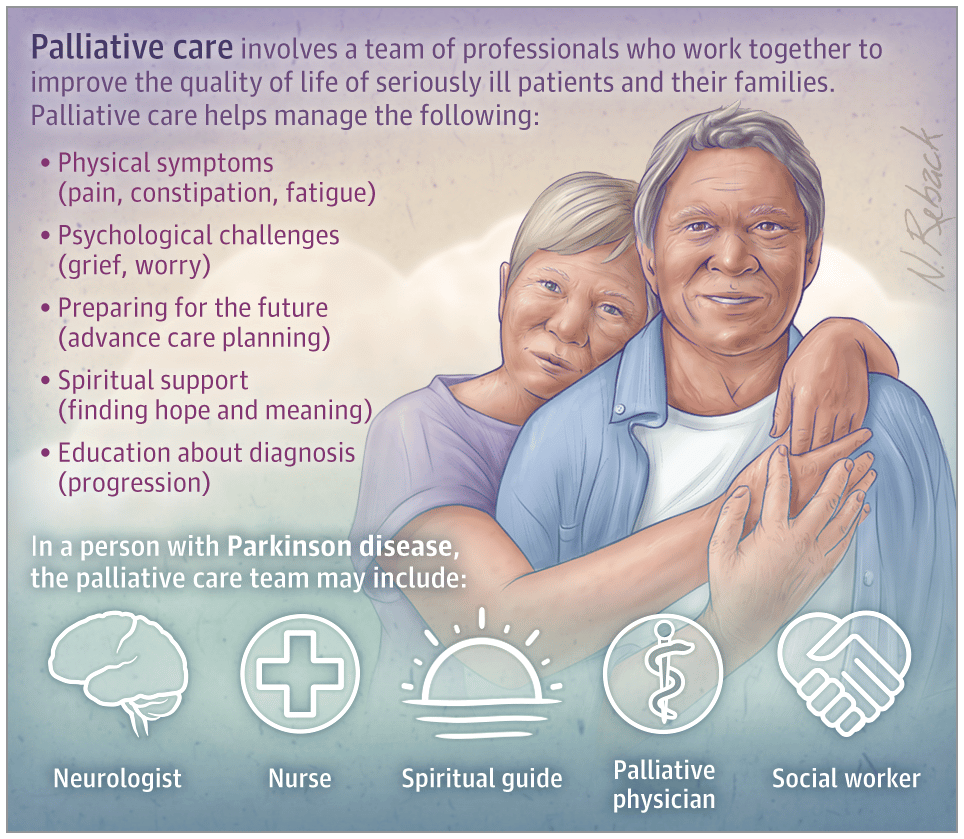
The project team is working with staff at the centers to put the program in place. The team is
- Helping centers develop palliative care teams, which include a neurologist, nurse, social worker, chaplain, and primary care doctor
- Adapting patient screening and other processes for each center
- Adapting clinician checklists and other materials as needed
- Training staff at the centers and providing ongoing coaching, support, and feedback
What Are The Symptoms Of Parkinson’s Towards The End Of Life
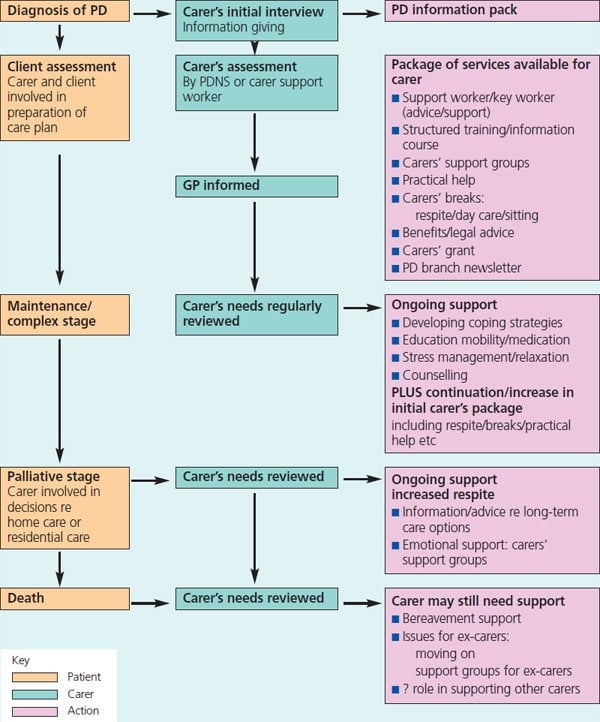
Parkinsons progresses in stages: diagnosis, maintenance, advanced and palliative. Professionals should have talk to people with Parkinsons about advance care planning in the earlier stages of the disease. This can allow them to express their wishes and preferences for their care in the later stages of the disease and make plans for the future.
Although the condition progresses differently and at a different speed for each person, the advanced stage can potentially cover a long period of time.
Problems that affect someone with advanced Parkinsons may include:
- medicines being less effective at managing symptoms than before
- having to take lots of medicines to manage symptoms and side effects
- more off periods when the effects of medication are reduced, and people experience movement fluctuations and involuntary movements
- increased mobility problems and falls
- swallowing difficulties
- less control of their Parkinsons symptoms, which become less predictable
Some of the more advanced symptoms can lead to increased disability and poor health, which can make someone more vulnerable to infection, such as pneumonia. People with Parkinsons most often die because of an infection or another condition, usually caused by Parkinsons.
Don’t Miss: Parkinson’s And Sleep Patterns
Late Stage: Advent Of Significant Disability/hospice To Death/bereavement
In our model, the late stage becomes a matter of implementing plans and preferences identified in the middle stage including hospice when appropriate. Legal paperwork will be available to minimize confusion, misunderstandings, or other bumps in the road. Of course, it is not likely that all developments can be foreseen and planned for, but these should be the exception. If the plan includes contingencies based on the nature of specific health issues as they unfold, there can be course adjustments as opposed to confusion and stress related to confrontation of unanticipated issues.
We recommended that the patients primary neurologist stay engaged with the patient and carepartner in late stage. By that time, a significant relationship based on experience and trust has often been created with both the patient and carepartner. If not, following the Graboys allegory, it should have been. From our perspective it seems that many neurologists are uncomfortable remaining involved after they can no longer fix their patient. Training in palliative care or involvement of palliative medicine specialists could help remedy this issue.
Early Stage: Diagnosis To 5 Years
Given confusion and misperceptions about palliative care, we suggest using the term supportive care and discussing this concept as PD Life Enhancement, or something similar. Palliative care should provide a comprehensive, coordinated, and consistent approach for the medical and PD support communities designed to maximize quality of life for patients, carepartners, and families starting at diagnosis and to reduce stress for the duration of the disease and bereavement period.3
The key points for diagnosis were included in the Graboys allegory. Another important element is sharing informational resources . We recommend scheduling follow-up a month after diagnosis since many patients are shell-shocked and unable to absorb much beyond the words PD. This is an opportunity for the doctor to assess how the patient and carepartner are doing, ask if they have reviewed information resources, and answer questions. The potential value of support groups should be discussed. Finally, it is important for the doctor to outline what information to bring for future appointments to make appropriate care decisions.
Don’t Miss: What Diseases Are Similar To Parkinson’s
Pd Support Organization Proposal
In order for the three-legged stool concept to work consistently and to facilitate development and implementation of programs as well as sharing of best practices, we recommended development of a unified regional program coordinated by a single national entity. Based on our information and experience, we recommended the approach taken by Association of Independent Regional Parkinson Organizations as a model that allows for autonomy and at the same time keeps the benefits of being part of a group, such as timely sharing of information and learning from fellow members successes and failures. As a model for a single region, the Muhammad Ali Parkinsons Center in Phoenix is one potential candidate.
Q: Can You Describe A Typical Initial Visit To The Legacy Care Program
A: Typically, a patient is referred to the Muhammad Ali Legacy Care Program by one of the movement disorder neurologists at the Muhammad Ali Parkinson Center of the Barrow Neurological Institute. Our program coordinator and nurse review the referral and then schedule an appointment for the person in the MDC. Prior to the MDC appointment, I meet with both the person with PD and their care partner over the phone to complete the intake and assessment process.
During the initial MDC appointment, the patient and their family member can expect to meet with their movement disorder neurologist , a member of the outpatient therapy team , our chaplain, and the social worker . Since I meet with the person with PD and care partner ahead of time over the phone, our follow-up conversation is focused on providing any resources that were discussed and/or touching base on any additional needs the patient and/or family might have thought of since we last spoke.
Read Also: Hearing Loss And Parkinson’s
How Hospice Helps People With Parkinsons Disease
During Parkinsons final stages, medications and treatments are generally no longer effective in controlling symptoms of the disease. This is when hospice care can provide care and support that helps both the patient and their loved ones. Care is provided wherever someone calls home a private residence, assisted living or skilled nursing facility, or hospital.
What Do I Need To Do To Get Hospice Care
There are many easy ways to start the process. You can certainly speak with your doctor about getting hospice care. You can also refer yourself or a loved one by filling out our online referral form. You can also call our patient access center at 800-207-6908. Once you refer yourself, or your loved one, a LCFL patient access specialist will be in touch with the next steps. This will include an assessment to determine if you would qualify for the hospice care benefit.
If it isnt quite time for hospice care, they may tell you about our palliative care service that also manages pain and symptoms for people living with advanced illnesses such as Parkinsons Disease.
Recent Posts
Recommended Reading: Will There Ever Be A Cure For Parkinsons Disease
Don’t Miss: Muscle Pain And Parkinson’s Disease
Brightview Senior Living Enrichment Programs
Flourishing at Brightview
The Flourishing at Brightview program before residents move in, Brightview Senior Living associates take the time to learn each residents likes, dislikes, careers, past and present hobbies, and aspirations to ensure they receive the most of what Brightview offers. New residents are introduced to current residents with similar interests, and invitations to meals and other activities make it easier to make friends quickly.
Care Philosophy
Brightviews approach to care is centered on Possibilities, Independence, and Choice. Residents who require a helping hand are encouraged to maintain their independence and choice in their activities of daily living. We believe that each person, no matter how old or frail, has the possibility to grow and experience joy every day.
SPICE in Motion
Bright Minds
Bright Minds is a collection of Brightview community offerings that are designed to improve the overall brain health and cognitive function of our residents. With Bright Minds, we focus on creating and maintaining healthy lifestyle habits from increased exercise, social interaction, and healthy eating to managing chronic health conditions to keep you active, and your brain healthy.
Eversound
Mind & Music
- Improve mood and attention
- Create higher quality of life and well-being
With Mind & Music added to their routines, Wellspring Village® residents living with dementia enjoy these benefits and more for brighter, happier days.
What Are The Surgical Treatments For Parkinsons Disease
Most patients with Parkinsons disease can maintain a good quality of life with medications. However, as the disease worsens, medications may no longer be effective in some patients. In these patients, the effectiveness of medications becomes unpredictable reducing symptoms during on periods and no longer controlling symptoms during off periods, which usually occur when the medication is wearing off and just before the next dose is to be taken. Sometimes these variations can be managed with changes in medications. However, sometimes they cant. Based on the type and severity of your symptoms, the failure of adjustments in your medications, the decline in your quality of life and your overall health, your doctor may discuss some of the available surgical options.
Also Check: Gut Health And Parkinson’s Disease
Palliative Care For Parkinsons Disease
Jeffrey Sheung Ching Ng
Palliative Medicine Physician, Haven of Hope Hospital, Hong Kong, China
Correspondence to:
Abstract: Parkinsons disease is a slowly progressive multi-system neurodegenerative disorder, with no available disease-modifying treatment. The disease is associated with motor and non-motor symptoms leading to impaired quality of life, disability and significant caregiver distress. Patients with PD benefit from palliative care which provides a holistic approach to meet their multi-faceted needs, including symptom control, communication needs and caregiver support. This article would review on recent articles addressing palliative care for PD.
Keywords: Parkinsons disease palliative care prognostication motor symptoms
Submitted Sep 25, 2017. Accepted for publication Oct 26, 2017.
doi: 10.21037/apm.2017.12.02
Q: Will Medicare And/or Private Insurance Cover The Costs Of Palliative Care
A: I can tell you that our Legacy Care Program is covered and does not affect any other payments made by Medicare and/or private insurances. For any other program, I would advise and strongly suggest that you check with the care-providing agency of choice to confirm coverage.
Tips and Takeaways
- Palliative care is a clinical approach that focuses on improving quality of life for people with complex diseases. It can begin at any point during disease progression and work in conjunction with a treatment plan.
- Palliative care programs for PD provide people with PD and their care partners additional resources and check-ins as the disease becomes more complex and difficult to manage. Multi-disciplinary care is provided with a focus on maximizing communication between the team members.
- Palliative care is different from hospice care. Palliative care refers to all treatments throughout the disease course focused on quality of life. Hospice care on the other hand, is provided to improve the quality of life only when end of life is near.
- Discuss the possibility of a palliative care referral with your movement disorders neurologist. A social worker may also be able to connect you with a palliative care program.
You May Like: What Are The Very First Signs Of Parkinson’s Disease
How Can Palliative Care Help In Parkinson’s
As Parkinson’s progresses and symptoms no longer respond well to treatment, daily living and quality of life become more difficult. You and your carer may need more help to manage your symptoms and physical requirements as well as your psychological and emotional needs.
The main principles of palliative care in Parkinsons are:
- focusing on quality of life, including good symptom control
- discontinuing any unnecessary medication or inappropriate interventions such as blood tests and scans
- responding to your psychological, social and spiritual needs
- caring both for you and those close to you
- maintaining open and sensitive communication between you, your family, carer and healthcare team
- respecting the individual choices you and your family make, for example treatment options and deciding where to die.
Can I Afford Hospice Care
Medicare pays for hospice services under the Medicare Hospice Benefit. Under this benefit all care, medications and medical supplies related to the hospice diagnosis are completely covered. The benefit allows for months of care not just during the last weeks of life.
Medicaid and most private insurances also have a hospice benefit that covers costs. For patients not receiving Medicare, Medicaid or private insurance benefits, Lower Cape Fear LifeCare never refuses care based on someones ability to pay.
Read Also: Pesticides And Parkinson Disease A Critical Review
Palliative Care Can Address The Mental Health Challenges Of Parkinsons Disease
Parkinsons disease causes changes in chemicals made by the brain to help regulate mood, motivation, energy, and sleep, among other important factors. As a result, Parkinsons patients have a high rate of depression and anxiety. Medication is often prescribed to replace those chemicals, putting Parkinsons patients in a better position to address their illness.
You cant pick yourself up by the bootstraps if Parkinsons has taken away the bootsand the boots are the coping molecules, says Katz. Sometimes patients are resistant to taking these medications, and I tell them, you wouldnt tell a diabetic to get through your diabetes without insulin.
Harris says that palliative care also teaches additional tools that can help improve the mental health of Parkinsons patients:
Treating The Symptoms Of Parkinsons Diseasehow Palliative Care Can Help
While there is no cure for Parkinsons disease, there are a growing number of treatments that can provide you with relief from its symptoms. People with Parkinsons disease are often prescribed a combination of levodopa and carbidopa, which helps replenish the brains shrinking supply of dopamine.
A new therapy uses electrodes surgically implanted inside the brain, and a small electrical device called a pulse generator to provide electrical deep brain stimulation . Parkinsons patients also benefit from the expertise of physical, occupational and speech therapists to help them manage practical issues in their daily lives.
Other symptoms of Parkinsons disease include a variety of motion-related issues, as well as sleep disturbances, fatigue , constipation and other gastrointestinal problems, and low blood pressure.
Another whole area of Parkinsons symptoms is called cognitive decline, whereby ravages of the disease affect thinking and other uses of the brain. These include troubling mood disorders like depression and anxiety, unclear thinking, difficulty concentrating on a task and the potential emergence of dementia.
Some people become more disabled and dependent over time despite the best treatments. They may come to need so much help with the routine tasks of living that they require 24-hour care. This care may be provided at home or in a setting like assisted living, where they get the personal care they need.
Recommended Reading: Stabilizing Pen For Parkinson’s
Motor Symptoms And Global Disability
Motor symptoms, as measured using the Unified Parkinsons Disease Rating Scale , Hoehn and Yahr Scale and the Progressive Supranuclear Palsy Rating Scale , were significant predictors of mortality in patients with PDRD. Beyer et al found higher mean UPDRS scores, 65 versus 42 , suggesting that greater motor impairment predicted death. Studies with median follow-up times ranging from 4 to 8 years estimated the association of 10-unit increases in baseline motor UPDRS Score on mortality and found statistically significant increased HRs for mortality of 1.17 up to 1.4 for each 10-unit increase in UPDRS Score. Baseline H& Y staging was significantly higher among those who died ) compared with those who survived ). Posada et al went further by splitting H& Y into early and later progression stages at baseline as a predictor for mortality and found that HRs increased by stage, from 1.5 for H& Y stages 1 and 2 to 2.3 for H& Y stages 35, both compared with patients with no PD and after controlling for comorbidities and demographic characteristics. Oosterveld et al stratified UPDRS total motor scores by greater than or equal to 30 compared with less than 30 and found an HR of 1.63 . Chiu et al compared the association of PSPRS scores on mortality and found increased HRs of 1.96 for 3548 on the PSPRS, 2.99 for 4862 and 8.55 for greater than 62 when compared with scores of 034.
Is Parkinsons Disease Fatal
Parkinsons disease itself doesnt cause death. However, symptoms related to Parkinsons can be fatal. For example, injuries that occur because of a fall or problems associated with dementia can be fatal.
Some people with Parkinsons experience difficulty swallowing. This can lead to aspiration pneumonia. This condition is caused when foods, or other foreign objects, are inhaled into the lungs.
Recommended Reading: Tell Me About Parkinson’s
Palliative Care As An Option
If your loved one is not eligible for hospice, the good news is that they can still receive palliative care. This type of care focuses on alleviating symptoms, discomfort, and stress associated with any illness, including PD.
The main difference between palliative care and hospice is that palliative care can be given along with standard treatments, including therapies intended to prolong life.
Disease Burden And Mortality In Pd
PD is a slowly progressive multi-system neurodegenerative disorder, mainly affecting patients in later years of life . It is the second most common neurodegenerative disease worldwide, with its incidence and prevalence on the rise along with aging of the population .
The characteristic classical motor features of PD include bradykinesia, rigidity, resting tremor and postural instability. Patients with PD also suffered from multiple non-motor features including olfactory dysfunction, cognitive impairment, psychiatric symptoms, sleep disorders, autonomic dysfunction, pain and fatigue . As the disease progresses, both motor and non-motor symptoms become prominent and treatment-resistant. Advanced PD is identified by disability requiring help for the activities of daily living, presence of motor fluctuations with limitations to perform basic activities of daily living without help, severe dysphagia, recurrent falls, and dementia . Up to now there are no disease-modifying treatments that can stop or delay the disease process or mortality.
Read Also: What Is End Stage Parkinson’s Disease