‘brain Pacemaker’ Effective For Years Against Parkinson’s Disease
- Date:
- Loyola University Health System
- Summary:
- A “brain pacemaker” called deep brain stimulation remains an effective treatment for Parkinson’s disease for at least three years.
A “brain pacemaker” called deep brain stimulation remains an effective treatment for Parkinson’s disease for at least three years, according to a study in the June 2010 online issue of Neurology®, the medical journal of the American Academy of Neurology.
But while improvements in motor function remained stable, there were gradual declines in health-related quality of life and cognitive abilities.
First author of the study is Frances M. Weaver, PhD, who has joint appointments at Edward Hines Jr. VA Hospital and Loyola University Chicago Stritch School of Medicine. Weaver was one of the lead investigators of a 2010 paper in the New England Journal of Medicine that found that motor functions remained stable for two years in DBS patients. The new additional analysis extended the follow-up period to 36 months.
DBS is a treatment for Parkinson’s patients who no longer benefit from medication, or who experience unacceptable side effects. DBS is not a cure, and it does not stop the disease from progressing. But in the right patients, DBS can significantly improve symptoms, especially tremors. DBS also can relieve muscle rigidity that causes decreased range of motion.
Story Source:
What Happens After The Surgery
After the surgery, you stay in the hospital for about 10 days. You then go to a rehabilitation clinic. During your stay there, the pacemaker settings are adjusted until the Parkinsons disease symptoms have been reduced as much as possible. The medication is usually already adjusted then too. The rehabilitation treatment also includes things like movement therapy and relaxation techniques.
Strenous physical activities should be avoided in the first few weeks after the surgery. You shouldnt go swimming or take a bath either, because that could affect the wound-healing process.
The follow-up care also includes regular check-ups: You have an appointment every three to six months to see whether the Parkinson’s disease is progressing and how well the pacemaker is working. The battery inside the pacemaker might have to be replaced after three to five years. This can be done through a small cut in the skin after numbing the area. The electrodes in the brain dont have to be replaced for this reason. There are also devices that don’t need batteries. Some can be recharged every week using a recharger.
People who have a brain pacemaker are given a special pacemaker identification card which they should carry on them at all times. Its also important to tell medical professionals that you have a brain pacemaker.
Risks Of Deep Brain Stimulation
As with any medical procedure, there are genuine risks of getting the DBS procedure done.
General risks are seizures, infections, blood clots, excessive bleeding, and anesthesia reactions.
There is a risk that DBS may lead to speech and balance-related afflictions from Parkinsons to worsen.
DBS can also worsen depression in some people with Parkinsons.
Don’t Miss: Parkinson’s Disease Causes Death
Less Medication More Relief
Medtronic DBS therapy may reduce the need for other Parkinsons medications1 and, consequently, medication-related side effects. DBS delivers therapy 24 hours a day and doesnt wear off while sleeping. Its already working when you wake up.
* Signal may not be present or measurable in all patients. Clinical benefits of brain sensing have not been established.
Advances In Dbs Technology

The treatment can be used to tackle additional neurological problems and other disorders, Wodziak said, including epilepsy, seizures and dystonia, which is the sustained, involuntary contraction of muscles and can lead to painful cramping of the feet or hands, curling toes, or turning and twisting of the neck. A version of the same technology can even be used on the spinal cord. This year, Dr. Andre Machado of the Cleveland Clinic performed the first DBS surgery for stroke recovery using the Boston Scientific Vercise system. It is also considered for depression and weight loss.
Although the treatment has been around since the 90’s, there have been some incremental advances to the technology, including leads capable of focusing electricity to increasingly specific parts of the brain and smaller generators capable of connecting to devices using Bluetooth. Abbott’s DBS system was the first to be approved in the United States with a “directional lead,” which allows physicians to direct current more precisely than traditional DBS. It also allows for system control from an iPod Touch.
Read Also: What Are The Very First Signs Of Parkinson’s Disease
Like A Pacemaker For The Brain
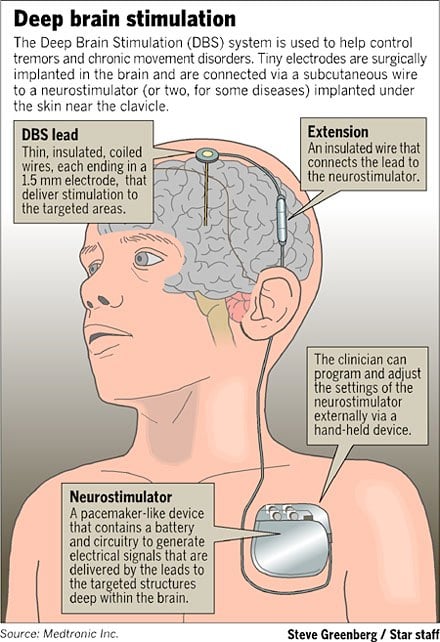
Deep brain stimulation is a surgical treatment sometimes used in Parkinsons and other conditions. In this treatment, small pulses of electrical current are applied to specific locations in the brain through implanted electrodes. These electrodes are connected by wires that run under the skin to a programmable internal pulse generator, which is usually implanted just under the collarbone . It contains a battery and some electronics to generate the pulses, similar to a heart pacemaker. The device delivers electrical stimulation to specific brain areas that are involved in movement control. Electrical stimulation at precise locations in the brain is thought to restore the balance of the circuits that are disrupted in Parkinsons disease.
DBS can alleviate tremor, reduce stiffness, and lessen dyskinesias. It can very effectively smooth out on/off fluctuations.
Prior to the introduction of DBS in the 1990s, the main surgical treatment for Parkinsons disease involved inserting a probe into the brain and heating the tip of the probe to burn a very small region of brain tissue. The burn, known as a lesion, was made at the same targets that we now stimulate. Lesional surgery is still a useful option in some cases where DBS is not possible. Recently it has become possible to create lesions noninvasively using focused ultrasound.
Side Effects Of Brain Stimulation
Deep brain stimulation sometimes leads to changes in behavior, such as increased motivation, mood swings, or even . Other possible side effects include trouble with movements such as walking, balance problems, slurred speech and temporary confusion. They often go away again by adjusting the pacemaker settings or medication. But these problems are sometimes caused by the Parkinsons disease itself. In order to determine whether they are normal symptoms of the disease or side effects of brain stimulation, a thorough medical examination is needed.
Deep brain stimulation can also affect your feelings, relationships with others, and your family life. Some of these effects are positive, but they may also lead to difficult situations or conflicts. Then professional psychological support can help.
If the side effects are too distressing, the brain pacemaker can be removed again.
Don’t Miss: Transcranial Magnetic Stimulation Parkinson’s
Finding Maximum Relief From Symptoms
A few weeks after his DBS system was implanted, John underwent his initial session to turn it on and test different settings to maximize relief of his symptoms.
While DBS is not a cure, and does not stop the condition progressing, it can significantly improve patients quality of life, and has become an important part of the treatment of Parkinsons disease to improve patients movement control. DBS has become the standard of surgical care for appropriately chosen patients like John, extending the time they can experience relief from disease symptoms.
As the use of DBS becomes more widespread, physicians are gaining a better understanding of its efficacy and limitations. Newer targets in the brain are being investigated to capture the symptoms still inadequately controlled by current methods.
Please note: This information should not be used as a substitute for medical treatment and advice. Always consult a medical professional about any health-related questions or concerns.
How Is Deep Brain Stimulation Performed
Before the actual procedure begins, for most patients, a head frame is positioned on your head, which keeps your head still during brain imaging and is used to deliver the electrode to the target in the brain. Surgical pins or screws are used to secure the frame to your head. Sedation is typically given during this portion of the procedure.
Your neurosurgeon will implant the deep brain stimulation system in one to three stages.
First, a small hole is made in the skull. The leads, which have electrodes at the ends, are passed through this hole and surgically implanted in the areas of the brain identified as the site responsible for the movements caused by Parkinsons disease.
Most people with Parkinson’s disease will require one lead placed on each side of the brain unless symptoms are mostly one-sided . Each side of the brain controls the opposite side of the body, so each lead is inserted on the opposite side of where symptoms are occurring. Sometimes this procedure is done in stages one lead is placed at one time followed by another surgery for the other side. In other patients, both leads are placed during the same operation. Many times patients are awake during lead insertion. An intraoperative MRI is also sometimes used to image the lead location.
Also Check: Restless Leg Syndrome And Parkinson’s Disease
‘brain Pacemaker Has Proven Benefits For Patients With Some Movement Disorders
Among the more than 500 patients who have undergone deep brain stimulation the implantation of a brain pacemaker and electrodes to ease symptoms of movement disorders one of the common observations is that they wish they had done it earlier, says Nader Pouratian, MD, director of UCLAs Neurosurgical Movement Disorders Program.
In the United States, an estimated 10-million people have essential tremor and 1 million have Parkinsons disease. While DBS does not cure or change the trajectory of either disease, it is a safe and effective procedure that provides symptomatic relief to many patients, Dr. Pouratian says. The procedure has most recently been approved for two more conditions, dystonia and obsessive-compulsive disorder. It is also being studied for its potential to help in a number of other conditions.
In DBS, electrodes are strategically placed in the brain while a battery-powered generator is implanted in the chest to emit continuous pulses, correcting the abnormal patterns of brain activity for patients with neurological disease.
Next
Loss Of Dopamine Movement Problems
He was far from alone Parkinsons disease is the second most common neurodegenerative disease. A report in 2017 estimated that it affects over 6 million people worldwide. The main symptoms include stiffness , slowness of movement , problems with gait , instability which may lead to falls, and tremor. Patients often report periods of severe symptoms in between periods of relief when movements are more normal .
Parkinsons is caused by progressive loss of brain cells in a small area of the brain known as the substantia nigra. These cells produce a chemical called dopamine which is important to the normal functioning of brain circuits that control movement. Depletion of dopamine disrupts normal function of these circuits, resulting in the symptoms described above. Dopamine replacement, in the form of a medication called levodopa, is the main medical therapy for Parkinsons.
Initially the symptoms respond well to medication, but after several years of treatment patients often develop more frequent and unpredictable ‘off’ periods, and unwanted and troublesome movements called dyskinesias may appear during ‘on’ periods. It becomes progressively harder to find a good level of medication that is enough to prevent the patient being ‘off’ but without causing dyskinesias.
Also Check: Emotional Symptoms Of Parkinson’s
What To Expect After Dbs
Surgery to implant the leads generally entails an overnight stay, while the IPG is usually implanted as same-day surgery. During recovery, your surgeon will talk to you about caring for your wounds, when you can shower, and any activity restrictions. Its usually recommended that any heavy lifting be avoided for a few weeks.
After another two to four weeks, youll return to have your device programmed. This process will continue for several weeks to ensure the stimulation settings are optimal to control your symptoms. During these visits, you will be shown how to turn the device on and off with the handheld device and check the battery level.
Once the programming has been completed, you will have regular follow-up visits to check and adjust the stimulation to maintain the most benefit for your symptoms.
Dbs Therapy Improves Dystonia
Dystonia is a neurological movement disorder characterized by involuntary muscle contraction, which forces some abnormalities of the body, sometimes painful movement or posture. Dystonia can affect any part of the body, including limbs, trunk, neck, eyelids, face and even vocal cords.
During the implementation of DBS, doctors can use EEG scans to find targeted nerve nuclei by recording the characteristics of different depths and trajectories of the brain, and observe the patients response to stimulation. This EEG scan allows the surgeon to pinpoint the correct area to place the electrode, thereby minimizing side effects. Researchers said that this technique greatly shortens the time of surgery and increases the accuracy of treatment.
During the treatment, the patient is always awake, and after receiving a small dose of sedatives, they can describe the side effects caused by the stimulation. The center also uses a unique acupuncture therapy to relieve the anxiety and pain of patients during the treatment, in order to reduce the patients dose of sedatives and anesthetics. DBS treatment usually takes 3 to 4 hours, and patients are usually hospitalized for 1 to 2 days. The pulse generator can be placed under the clavicle of the patient, and the programmed program can make the pulse last until one week after the operation.
You May Like: Can Parkinson’s Go Away
What Happens After Surgery
After surgery, you may take your regular dose of Parkinson’s medication immediately. You are kept overnight for monitoring and observation. Most patients are discharged home the next day.
During the recovery time after implanting the electrodes, you may feel better than normal. Brain swelling around the electrode tip causes a lesion effect that lasts a couple days to weeks. This temporary effect is a good predictor of your outcome once the stimulator is implanted and programmed.
About a week later, you will return to the hospital for outpatient surgery to implant the stimulator in the chest/abdomen. This surgery is performed under general anesthesia and takes about an hour. Patients go home the same day.
Step 7: implant the stimulator You will be taken to the OR and put to sleep with general anesthesia. A portion of the scalp incision is reopened to access the leads. A small incision is made near the collarbone and the neurostimulator is implanted under the skin. The lead is attached to an extension wire that is passed under the skin of the scalp, down the neck, to the stimulator/battery in the chest or abdomen. The device will be visible as a small bulge under the skin, but it is usually not seen under clothes.
You should avoid arm movements over your shoulder and excessive stretching of your neck while the incisions heal. Pain at the incision sites can be managed with medication.
The Symptoms That Dbs Treats
Deep brain stimulation is used primarily to treat the motor symptoms of Parkinsons disease, but this can vary somewhat between the different placement sites. Symptoms treated include:
- Stiffness
- Abnormal movements : Dyskinesias are often a side effect of medications for Parkinsons disease and include involuntary movements such as twisting, head bobbing, squirming, and more.
DBS is not usually helpful with walking problems or balance, though improvements in the symptoms above can indirectly affect walking. It also does not provide significant benefits for non-motor symptoms of Parkinsons such as cognitive changes, mood changes , or problems with sleeping.
The benefits of DBS can be estimated by looking at how a person responds to levodopa. Symptoms that respond to levodopa will often respond to DBS . But symptoms that are not changed with levodopa are unlikely to be improved by DBS.
DBS often allows for a reduction in the dosage of levodopa, which in turn can result in fewer involuntary movements and a reduction in off time. The result is often improved quality of life.
Recommended Reading: What Tests Are Done To Diagnose Parkinson’s
How Common Is Dbs
Dr. Sheth describes DBS as a very standard treatment. These are procedures that we do week in and week out, he said. It’s not investigational or experimental. Around the world, more than 150,000 patients have had DBS for Parkinson’s or tremor with a success rate of 95%.
Patients need to know that there are these alternatives. They need to know that they’re not necessarily stuck with these symptoms, that there may be a different way to get better control. That discussion is, of course, individual-specific, but the availability of these types of surgical treatments is important for patients to know about.
‘more Quality Time With The Girls’
While he is still in recovery, he said it had already made a big difference to his symptoms and he was not as reliant on his medication.
“I always felt like I was still a good dad but now I feel like I can really do that, I feel completely unrestricted,” he said.
“I can have so much more quality time with the girls. It’s just great.
“I feel more confident, my brain isn’t having to work so hard to keep up a facade of what I think I should look like.”
The Parkinson’s community has been welcoming, and people have been happy to talk to Mr Murfitt about their experiences.
“There’s been one person who’s gone through DBS that’s been really helpful,” he said.
“What I noticed the whole time was that there was never a flicker of doubt that she might have done the wrong thing, there’s no regret and I can see where that comes from.”
Recommended Reading: What Age Is Parkinson’s Disease Diagnosed
Stereotactic Dbs Vs Interventional Image
Stereotactic DBS surgery requires the patient to be off their medication. During the procedure, a frame stabilizes the head and provides coordinates to help the surgeons guide the lead to the correct location in the brain. The patient gets local anesthesia to keep them comfortable throughout each step along with a mild sedative to help them relax.
During image-guided DBS surgery, such as with interventional MRI or CT scan, the patient is often asleep under general anesthesia while the surgeon uses images of the brain to guide the lead to its target.
Some advanced centers offer both the stereotactic and iMRI-guided options for DBS surgery. In this case, the doctor and patient will discuss which procedure is better based on a number of factors.
For instance, the doctor may recommend an image-guided procedure for children, patients who have extreme symptoms, those who are especially anxious or fearful or those whose leads are going into certain parts of the brain.
Generally, DBS surgery follows this process: